Abstract
Purpose
Groin hernia repair is one of the most frequent operation performed worldwide. Chronic postoperative inguinal pain (CPIP) is the most common and challenging complication after surgical repair with subsequent high socio-economic impact. The aim of this study was to compare the one-year CPIP rates between Lichtenstein, trans-inguinal pre-peritoneal (TIPP), trans-abdominal pre-peritoneal (TAPP) and totally extra-peritoneal (TEP) repair techniques on the French Hernia Registry.
Methods
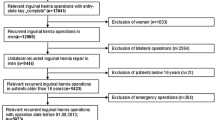
Between 2011 and 2021, 15,161 primary groin hernia repairs with 1-year follow-up were available on the register. Using propensity score (PS) matching, matched pairs were formed. Each group was compared in pairs independently; Lichtenstein versus TIPP, TEP and TAPP, TIPP versus TEP and TAPP and finally TEP versus TAPP.
Results
After PS matching analysis, Lichtenstein group showed disadvantage over TIPP, TAPP and TEP groups with significantly more CPIP at one year (15.2% vs 9.6%, p < 0.0001; 15.9% vs. 10.0%, p < 0.0001 and 16.1% vs. 12.4%, p = 0.002, respectively). The 1-year CPIP rates were similar comparing TIPP versus TAPP and TEP groups (9.3% vs 10.5%, p = 0.19 and 9.8% vs 11.8%, p = 0.05, respectively). There was significantly less CPIP rate after TAPP versus TEP repair (1.00% vs 11.9%, p = 0.02).
Conclusion
This register-based study confirms the higher CPIP risk after Lichtenstein repair compared to the pre-peritoneal repair techniques. TIPP leads to comparable CPIP rates than TAPP and TEP repairs.








Similar content being viewed by others
Data availability
The datasets analysed during the current study are available from the corresponding author on reasonable request.
References
Simons MP, Aufenacker T, Bay-Nielsen M et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403. https://doi.org/10.1007/s10029-009-0529-7
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Alfieri S, Amid PK, Campanelli G et al (2011) International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia 15:239–249. https://doi.org/10.1007/s10029-011-0798-9
Powell R, Johnston M, Smith WC et al (2012) Psychological risk factors for chronic post-surgical pain after inguinal hernia repair surgery: a prospective cohort study. Eur J Pain 16:600–610. https://doi.org/10.1016/j.ejpain.2011.08.010
Bittner R, Arregui ME, Bisgaard T et al (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc 25:2773–2843. https://doi.org/10.1007/s00464-011-1799-6
Koning GG, Keus F, Koeslag L et al (2012) Randomized clinical trial of chronic pain after the transinguinal preperitoneal technique compared with Lichtenstein’s method for inguinal hernia repair. Br J Surg 99:1365–1373. https://doi.org/10.1002/bjs.8862
Bökkerink WJV, Koning GG, Malagic D et al (2019) Long-term results from a randomized comparison of open transinguinal preperitoneal hernia repair and the Lichtenstein method (TULIP trial). Br J Surg 106:856–861. https://doi.org/10.1002/bjs.11178
Sharma P, Boyers D, Scott N et al (2015) The clinical effectiveness and cost-effectiveness of open mesh repairs in adults presenting with a clinically diagnosed primary unilateral inguinal hernia who are operated in an elective setting: systematic review and economic evaluation. Health Technol Assess 19:1–142. https://doi.org/10.3310/hta19920
Suwa K, Onda S, Yasuda J et al (2021) Single-blind randomized clinical trial of transinguinal preperitoneal repair using self-expanding mesh patch vs. Lichtenstein repair for adult male patients with primary unilateral inguinal hernia. Hernia 25:173–181. https://doi.org/10.1007/s10029-020-02301-8
El-Dhuwaib Y, Corless D, Emmett C et al (2013) Laparoscopic versus open repair of inguinal hernia: a longitudinal cohort study. Surg Endosc 27:936–945. https://doi.org/10.1007/s00464-012-2538-3
Demange MK, Fregni F (2011) Limits to clinical trials in surgical areas. Clinics (Sao Paulo) 66:159–161. https://doi.org/10.1590/s1807-59322011000100027
Grose E, Wilson S, Barkun J et al (2020) Use of propensity score methodology in contemporary high-impact surgical literature. J Am Coll Surg 230:101-112.e2. https://doi.org/10.1016/j.jamcollsurg.2019.10.003
Reinpold W (2017) Risk factors of chronic pain after inguinal hernia repair: a systematic review. Innov Surg Sci 2:61–68. https://doi.org/10.1515/iss-2017-0017
Mattei A (2009) Estimating and using propensity score in presence of missing background data: an application to assess the impact of childbearing on wellbeing. Stat Methods Appl 18:257–273. https://doi.org/10.1007/s10260-007-0086-0
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 46:399–424. https://doi.org/10.1080/00273171.2011.568786
McCaffrey DF, Griffin BA, Almirall D et al (2013) A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Stat Med 32:3388–3414. https://doi.org/10.1002/sim.5753
Austin PC (2014) A comparison of 12 algorithms for matching on the propensity score. Stat Med 33:1057–1069. https://doi.org/10.1002/sim.6004
Austin PC (2011) Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat 10:150–161. https://doi.org/10.1002/pst.433
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28:3083–3107. https://doi.org/10.1002/sim.3697
Rubin DB (2021) Multiple imputation for nonresponse in surveys | SpringerLink. https://link.springer.com/article/https://doi.org/10.1007/BF02924688. Accessed 23 Aug 2021
Hori T, Yasukawa D (2021) Fascinating history of groin hernias: comprehensive recognition of anatomy, classic considerations for herniorrhaphy, and current controversies in hernioplasty. World J Methodol 11:160–186. https://doi.org/10.5662/wjm.v11.i4.160
Andresen K, Rosenberg J (2018) Management of chronic pain after hernia repair. J Pain Res 11:675–681. https://doi.org/10.2147/JPR.S127820
Köckerling F, Hoffmann H, Adolf D et al (2020) Female sex as independent risk factor for chronic pain following elective incisional hernia repair: registry-based, propensity score-matched comparison. Hernia 24:567–576. https://doi.org/10.1007/s10029-019-02089-2
Romain B, Fabacher T, Ortega-Deballon P et al (2021) Longitudinal cohort study on preoperative pain as a risk factor for chronic postoperative inguinal pain after groin hernia repair at 2-year follow-up. Hernia. https://doi.org/10.1007/s10029-021-02404-w
Yang X-F, Liu J-L (2016) Anatomy essentials for laparoscopic inguinal hernia repair. Ann Transl Med 4:372. https://doi.org/10.21037/atm.2016.09.32
Bilsel Y, Abci I (2012) The search for ideal hernia repair; mesh materials and types. Int J Surg 10:317–321. https://doi.org/10.1016/j.ijsu.2012.05.002
Gillion JF, Soler M, Chollet JM, Club-Hernie members (2021) A registry-based 2-year follow-up comparative study of two meshes used in transinguinal preperitoneal (TIPP) groin hernia repair. Langenbecks Arch Surg 406:197–208. https://doi.org/10.1007/s00423-020-01993-x
Hoffmann H, Walther D, Bittner R et al (2020) Smaller inguinal hernias are independent risk factors for developing chronic postoperative inguinal pain (CPIP): a registry-based multivariable analysis of 57, 999 patients. Ann Surg 271:756–764. https://doi.org/10.1097/SLA.0000000000003065
Memon MA, Cooper NJ, Memon B et al (2003) Meta-analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg 90:1479–1492. https://doi.org/10.1002/bjs.4301
O’Reilly EA, Burke JP, O’Connell PR (2012) A meta-analysis of surgical morbidity and recurrence after laparoscopic and open repair of primary unilateral inguinal hernia. Ann Surg 255:846–853. https://doi.org/10.1097/SLA.0b013e31824e96cf
Chung RS, Rowland DY (1999) Meta-analyses of randomized controlled trials of laparoscopic vs conventional inguinal hernia repairs. Surg Endosc 13:689–694. https://doi.org/10.1007/s004649901074
Grant A, Go P, Fingerhut A et al (2000) Laparoscopic compared with open methods of groin hernia repair: systematic review of randomized controlled trials. Br J Surg 87:860–867
Schmedt CG, Sauerland S, Bittner R (2005) Comparison of endoscopic procedures vs Lichtenstein and other open mesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Surg Endosc 19:188–199. https://doi.org/10.1007/s00464-004-9126-0
Aiolfi A, Cavalli M, Micheletto G et al (2019) Primary inguinal hernia: systematic review and Bayesian network meta-analysis comparing open, laparoscopic transabdominal preperitoneal, totally extraperitoneal, and robotic preperitoneal repair. Hernia 23:473–484. https://doi.org/10.1007/s10029-019-01964-2
Lyu Y, Cheng Y, Wang B et al (2020) Comparison of endoscopic surgery and Lichtenstein repair for treatment of inguinal hernias: A network meta-analysis. Medicine (Baltimore) 99:e19134. https://doi.org/10.1097/MD.0000000000019134
Bullen NL, Massey LH, Antoniou SA et al (2019) Open versus laparoscopic mesh repair of primary unilateral uncomplicated inguinal hernia: a systematic review with meta-analysis and trial sequential analysis. Hernia 23:461–472. https://doi.org/10.1007/s10029-019-01989-7
Balshem H, Helfand M, Schünemann HJ et al (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64:401–406. https://doi.org/10.1016/j.jclinepi.2010.07.015
Atkins D, Best D, Briss PA et al (2004) Grading quality of evidence and strength of recommendations. BMJ 328:1490. https://doi.org/10.1136/bmj.328.7454.1490
Bragais LCG, Faylona JMV (2020) Adherence to international guidelines for Groin Hernia Management: a retrospective cross-sectional study in a tertiary government training hospital. Hernia 24:969–975. https://doi.org/10.1007/s10029-020-02207-5
Kennedy-Martin T, Curtis S, Faries D et al (2015) A literature review on the representativeness of randomized controlled trial samples and implications for the external validity of trial results. Trials 16:495. https://doi.org/10.1186/s13063-015-1023-4
Bhide A, Shah PS, Acharya G (2018) A simplified guide to randomized controlled trials. Acta Obstet Gynecol Scand 97:380–387. https://doi.org/10.1111/aogs.13309
Niebuhr H, Wegner F, Hukauf M et al (2018) What are the influencing factors for chronic pain following TAPP inguinal hernia repair: an analysis of 20,004 patients from the Herniamed Registry. Surg Endosc 32:1971–1983. https://doi.org/10.1007/s00464-017-5893-2
Kyle-Leinhase I, Köckerling F, Jørgensen LN et al (2018) Comparison of hernia registries: the CORE project. Hernia 22:561–575. https://doi.org/10.1007/s10029-017-1724-6
Köckerling F, Maneck M, Günster C et al (2020) Comparing routine administrative data with registry data for assessing quality of hospital care in patients with inguinal hernia. Hernia 24:143–151. https://doi.org/10.1007/s10029-019-02009-4
Prasad A, Shin M, Carey RM et al (2020) Propensity score matching in otolaryngologic literature: a systematic review and critical appraisal. PLoS ONE 15:0244423. https://doi.org/10.1371/journal.pone.0244423
Yao XI, Wang X, Speicher PJ et al (2017) Reporting and guidelines in propensity score analysis: a systematic review of cancer and cancer surgical studies. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djw323
Willaert W, De Bacquer D, Rogiers X et al (2012) Open preperitoneal techniques versus lichtenstein repair for elective inguinal hernias. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD008034.pub2
Sajid MS, Craciunas L, Singh KK et al (2013) Open transinguinal preperitoneal mesh repair of inguinal hernia: a targeted systematic review and meta-analysis of published randomized controlled trials. Gastroenterol Rep (Oxf) 1:127–137. https://doi.org/10.1093/gastro/got002
Li J, Ji Z, Li Y (2014) Comparison of laparoscopic versus open procedure in the treatment of recurrent inguinal hernia: a meta-analysis of the results. Am J Surg 207:602–612. https://doi.org/10.1016/j.amjsurg.2013.05.008
Köckerling F, Bittner R, Kofler M et al (2019) Lichtenstein versus total extraperitoneal patch plasty versus transabdominal patch plasty technique for primary unilateral inguinal hernia repair: a registry-based, propensity score-matched comparison of 57,906 patients. Ann Surg 269:351–357. https://doi.org/10.1097/SLA.0000000000002541
Belyansky I, Tsirline VB, Klima DA et al (2011) Prospective, comparative study of postoperative quality of life in TEP, TAPP, and modified Lichtenstein repairs. Ann Surg 254:709–714. https://doi.org/10.1097/SLA.0b013e3182359d07. (discussion 714–715)
S C, S van C, O U et al (2021) Quality of life after open versus laparoscopic preperitoneal mesh repair for unilateral inguinal hernias. Asian J Surg. https://doi.org/10.1016/j.asjsur.2021.03.014
Haroon M, Al-Sahaf O, Eguare E et al (2019) Postoperative outcomes and patient’s satisfaction after hybrid TIPP with UHS and TEP repair for inguinal hernias: a single-centre retrospective comparative study. Chirurgia (Bucur) 114:57–66. https://doi.org/10.21614/chirurgia.114.1.57
Aitola P, Airo I, Matikainen M (1998) Laparoscopic versus open preperitoneal inguinal hernia repair: a prospective randomised trial. Ann Chir Gynaecol 87:22–25
Romain B, Gillion J-F, Ortega-Deballon P et al (2018) Patient’s satisfaction at 2 years after groin hernia repair: any difference according to the technique? Hernia 22:801–812. https://doi.org/10.1007/s10029-018-1796-y
Pélissier EP, Ngo P, Gayet B (2011) Transinguinal preperitoneal patch (TIPP) under local anesthesia with sedation. Am Surg 77:1681–1684
Gillion J-F, Chollet J-M (2013) Chronic pain and quality of life (QoL) after transinguinal preperitoneal (TIPP) inguinal hernia repair using a totally extraperitoneal, parietalized, Polysoft ® memory ring patch : a series of 622 hernia repairs in 525 patients. Hernia 17:683–692. https://doi.org/10.1007/s10029-013-1121-8
Rives J, Lardennois B, Flament JB, Convers G (1973) The Dacron mesh sheet, treatment of choice of inguinal hernias in adults. Apropos of 183 cases. Chirurgie 99:564–575
Kler A, Sekhon N, Antoniou GA, Satyadas T (2021) Totally extra-peritoneal repair versus trans-abdominal pre-peritoneal repair for the laparoscopic surgical management of sportsman’s hernia: a systematic review and meta-analysis. Surg Endosc 35:5399–5413. https://doi.org/10.1007/s00464-021-08554-3
Goksoy B, Yilmaz G, Azamat IF, et al (2021) Laparoscopic Inguinal Hernia Repair-TAPP versus TEP: Results of 301 Consecutive Patients. Surg Technol Int 39:sti39/1427
Chen L-S, Chen W-C, Kang Y-N et al (2019) Effects of transabdominal preperitoneal and totally extraperitoneal inguinal hernia repair: an update systematic review and meta-analysis of randomized controlled trials. Surg Endosc 33:418–428. https://doi.org/10.1007/s00464-018-6314-x
Gass M, Banz VM, Rosella L et al (2012) TAPP or TEP? Population-based analysis of prospective data on 4,552 patients undergoing endoscopic inguinal hernia repair. World J Surg 36:2782–2786. https://doi.org/10.1007/s00268-012-1760-4
Gass M, Scheiwiller A, Sykora M, Metzger J (2016) TAPP or TEP for recurrent inguinal hernia? population-based analysis of prospective data on 1309 patients undergoing endoscopic repair for recurrent inguinal hernia. World J Surg 40:2348–2352. https://doi.org/10.1007/s00268-016-3545-7
Wei FX, Zhang YC, Han W et al (2015) Transabdominal preperitoneal (TAPP) versus totally extraperitoneal (TEP) for laparoscopic hernia repair: a meta-analysis. Surg Laparosc Endosc Percutan Tech 25:375–383. https://doi.org/10.1097/SLE.0000000000000123
Kukleta JF (2019) Why I prefer TAPP repair for uncomplicated unilateral groin hernia in adults. Hernia 23:617–620. https://doi.org/10.1007/s10029-019-01938-4
Rodha MS, Meena SP, Premi K et al (2022) Pain after transabdominal preperitoneal (TAPP) or totally extraperitoneal (TEP) technique for unilateral inguinal hernia: a randomized controlled trial. Cureus 14:e24582. https://doi.org/10.7759/cureus.24582
Funding
The present research did not receive any financial rewards.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by RH and YR. Data were managed by JFG. Statistical analysis was performed by LB and Dr CB. The first draft of the manuscript was written by RH and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. Editorial assistance, in the form of language editing and correction, was provided by XpertScientific Editing and Consulting Services.
Corresponding author
Ethics declarations
Conflict of interest
YR declares scientific support for BD® and Medtronic®. YR declares his position as board member of the EHS. All other authors declare that they have no conflict of interest.
Ethics approval
Every patient is informed that their anonymized data are registered in online data bank. The registry complies with requirements of the French national commission of information and liberties (CNIL; registration number 1993959v0).
Human and animal rights
The study including human participants has been performed in accordance with the ethical standards of the Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all patients prior to all surgical procedures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hurel, R., Bouazzi, L., Barbe, C. et al. Lichtenstein versus TIPP versus TAPP versus TEP for primary inguinal hernia, a matched propensity score study on the French Club Hernie Registry. Hernia 27, 1165–1177 (2023). https://doi.org/10.1007/s10029-023-02737-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-023-02737-8