Abstract
Purpose
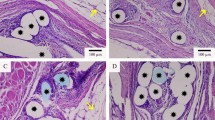
This study evaluated the manufacturing method and anti-adhesion properties of a new composite mesh in the rat model, which was made from sirolimus (SRL) grafts on a poly(l-lactic acid) (PLLA)-modified polypropylene (PP) hernia mesh.
Methods
PLLA was first grafted onto argon-plasma-treated native PP mesh through catalysis of stannous chloride. SRL was grafted onto the surface of PP-PLLA meshes using catalysis of 1-(3-dimethylaminopropyl)-3-ethylcarbodiimide hydrochloride (EDC) and 4-dimethylaminopyridine (DMAP) in a CH2Cl2 solvent. Sprague–Dawley female rats received either SRL-coated meshes, PP-PLLA meshes, or native PP meshes to repair abdominal wall defects. At different intervals, rats were euthanized by a lethal dose of chloral hydrate and adhesion area and tenacity were evaluated. Sections of the mesh with adjacent tissues were assessed histologically.
Results
Attenuated total reflection Fourier transformed infrared (ATR-FTIR) spectroscopy indicated the existence of a C=O group absorption peak (1724.1 cm−1), and scanning electron microscope morphological analysis indicated that the surface of the PP mesh was covered with SRL. Compared to the native PP meshes and PP-PLLA meshes, SRL-coated meshes demonstrated the greatest ability to decrease the formation of adhesions (P < 0.05) and inflammation.
Conclusions
The SRL-coated composite mesh showed minimal formation of intra-abdominal adhesions in a rat model of abdominal wall defect repair.







Similar content being viewed by others
References
Bosanquet DC, Ansell J, Abdelrahman T, Cornish J, Harries R, Stimpson A, Davies L, Glasbey JC, Frewer KA, Frewer NC, Russell D, Russell I, Torkington J (2015) Systematic review and meta-regression of factors affecting midline incisional hernia rates: analysis of 14,618 patients. PLoS One 10(9):e0138745. https://doi.org/10.1371/journal.pone.0138745
Zinther NB, Wara P, Friis-Andersen H (2010) Intraperitoneal onlay mesh: an experimental study of adhesion formation in a sheep model. Hernia J Hernias Abdom Wall Surg 14(3):283–289. https://doi.org/10.1007/s10029-009-0622-y
Jamry A, Jalynski M, Piskorz L, Brocki M (2013) Assessment of adhesion formation after laparoscopic intraperitoneal implantation of Dynamesh IPOM mesh. Arch Med Sci AMS 9(3):487–492. https://doi.org/10.5114/aoms.2013.35345
Muysoms FE, Bontinck J, Pletinckx P (2011) Complications of mesh devices for intraperitoneal umbilical hernia repair: a word of caution. Hernia J Hernias Abdom Wall Surg 15(4):463–468. https://doi.org/10.1007/s10029-010-0692-x
Shankaran V, Weber DJ, Reed RL 2nd, Luchette FA (2011) A review of available prosthetics for ventral hernia repair. Ann Surg 253(1):16–26. https://doi.org/10.1097/SLA.0b013e3181f9b6e6
Anderson JM, Rodriguez A, Chang DT (2008) Foreign body reaction to biomaterials. Semin Immunol 20(2):86–100. https://doi.org/10.1016/j.smim.2007.11.004
Poppas DP, Sung JJ, Magro CM, Chen J, Toyohara JP, Ramshaw BJ, Felsen D (2016) Hydrogel coated mesh decreases tissue reaction resulting from polypropylene mesh implant: implication in hernia repair. Hernia J Hernias Abdom Wall Surg 20(4):623–632. https://doi.org/10.1007/s10029-016-1481-y
Deeken CR, Faucher KM, Matthews BD (2012) A review of the composition, characteristics, and effectiveness of barrier mesh prostheses utilized for laparoscopic ventral hernia repair. Surg Endosc 26(2):566–575. https://doi.org/10.1007/s00464-011-1899-3
Practice Committee of the American Society for Reproductive Medicine (2006) Control and prevention of peritoneal adhesions in gynecologic surgery. Fertil Steril 86(5 Suppl 1):S1–S5. https://doi.org/10.1016/j.fertnstert.2006.07.1483
Langer JC, Liebman SM, Monk PK, Pelletier GJ (1995) Mast cell mediators and peritoneal adhesion formation in the rat. J Surg Res 59(3):344–348. https://doi.org/10.1006/jsre.1995.1174
Li L, Zheng X, Fan D, Yu S, Wu D, Fan C, Cui W, Ruan H (2016) Release of celecoxib from a bi-layer biomimetic tendon sheath to prevent tissue adhesion. Mater Sci Eng C Mater Biol Appl 61:220–226. https://doi.org/10.1016/j.msec.2015.12.028
Chisari A, Pistritto AM, Piccolo R, La Manna A, Danzi GB (2016) The ultimaster biodegradable-polymer sirolimus-eluting stent: an updated review of clinical evidence. Int J Mol Sci 17(9):1490. https://doi.org/10.3390/ijms17091490
Motse KG, Mashabane MJ (2016) Sirolimus-induced lymphoedema. S Afr Med J Suid-Afrikaanse tydskrif vir geneeskunde 106(9):886–887. https://doi.org/10.7196/SAMJ.2016.v106i9.10636
Zhang Z, Zhang T, Li J, Ji Z, Zhou H, Zhou X, Gu N (2014) Preparation of poly(l-lactic acid)-modified polypropylene mesh and its antiadhesion in experimental abdominal wall defect repair. J Biomed Mater Res Part B Appl Biomater 102(1):12–21
Maciver AH, McCall MD, Edgar RL, Thiesen AL, Bigam DL, Churchill TA, Shapiro AM (2011) Sirolimus drug-eluting, hydrogel-impregnated polypropylene mesh reduces intra-abdominal adhesion formation in a mouse model. Surgery 150(5):907–915. https://doi.org/10.1016/j.surg.2011.06.022
Gomathi N, Neogi S (2013) Surface modification of polypropylene using argon plasma: statistical optimization of the process variables. Appl Surf Sci 51(6):1273–1278
Jayanth ST, Pulimood A, Abraham D, Rajaram A, Paul MJ, Nair A (2015) A randomized controlled experimental study comparing chitosan coated polypropylene mesh and proceed mesh for abdominal wall defect closure. Ann Med Surg 4(4):388–394. https://doi.org/10.1016/j.amsu.2015.10.002
Zhang L (2015) Incidence of abdominal incisional hernia in developing country: a retrospective cohort study. Int J Clin Exp Med 8(8):13649–13652
Usher FC, Ochsner J, Tuttle LL Jr (1958) Use of marlex mesh in the repair of incisional hernias. Am Surg 24(12):969–974
Vorst AL, Kaoutzanis C, Carbonell AM, Franz MG (2015) Evolution and advances in laparoscopic ventral and incisional hernia repair. World J Gastrointest Surg 7(11):293–305. https://doi.org/10.4240/wjgs.v7.i11.293
Rastegarpour A, Cheung M, Vardhan M, Ibrahim MM, Butler CE, Levinson H (2016) Surgical mesh for ventral incisional hernia repairs: understanding mesh design. Plast Surg (Oakville, Ont) 24(1):41–50
Turza KC, Butler CE (2012) Adhesions and meshes: synthetic versus bioprosthetic. Plast Reconstr Surg 130(5 Suppl 2):206S–213S. https://doi.org/10.1097/PRS.0b013e3182638d48
Arung W, Drion P, Detry O (2016) Sepramesh and postoperative peritoneal adhesions in a rat model. Acta Chir Belg 116:1–5. https://doi.org/10.1080/00015458.2016.1181322
Guler S, Cimen S, Hu Q, Venkatachalam AB, Alwayn I (2016) Effects of mTOR inhibitors in prevention of abdominal adhesions. J Investig Surg Off J Acad Surg Res 29(5):275–281. https://doi.org/10.3109/08941939.2016.1149643
Skalsky I, Filova E, Szarszoi O, Parizek M, Lytvynets A, Maluskova J, Lodererova A, Brynda E, Lisa V, Burdikova Z, Capek M, Pirk J, Bacakova L (2011) A periadventitial sirolimus-releasing mesh decreased intimal hyperplasia in a rabbit model. Physiol Res 60(3):585–588
Laschke MW, Haufel JM, Roller J, Schorr H, Menger MD (2009) Rapamycin, but not cyclosporine A, inhibits vascularization and incorporation of implanted surgical meshes. Transpl Int Off J Eur Soc Org Transplant 22(6):654–662. https://doi.org/10.1111/j.1432-2277.2009.00841.x
Scheuerlein H, Rauchfuss F, Gharbi A, Heise M, Settmacher U (2011) Laparoscopic incisional hernia repair after solid-organ transplantation. Transplant Proc 43(5):1783–1789. https://doi.org/10.1016/j.transproceed.2011.03.082
Acknowledgements
This work was financially supported by the Fundamental Research Funds for the Central Universities (2242016k40145) and National Natural Science Foundation of China (81600407).
Funding
This work was financially supported by the Fundamental Research Funds for the Central Universities (2242016k40145) and National Natural Science Foundation of China (81600407).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Shenglin Lu, Wanjun Hu, Zhigang Zhang, Zhenling Ji, and Tianzhu Zhang declare that they have no conflict of interest.
Ethical approval
All applicable international, national, and institutional guidelines for the care and use of animals were followed.
Human and animal rights
All animal experiments were approved by the Institutional Animal Care and Use Committee of Southeast University and were in compliance with all regulatory guidelines.
Informed consent
For this type of article informed consent is not required.
Rights and permissions
About this article
Cite this article
Lu, S., Hu, W., Zhang, Z. et al. Sirolimus-coated, poly(l-lactic acid)-modified polypropylene mesh with minimal intra-peritoneal adhesion formation in a rat model. Hernia 22, 1051–1060 (2018). https://doi.org/10.1007/s10029-018-1782-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-018-1782-4