Abstract
Purpose
The aim of this study was to evaluate the outcome, with a special reference to recurrence and postoperative chronic pain, of the modified Kugel herniorrhaphy (MKH) using standardized dissection of the preperitoneal space.
Patients and methods
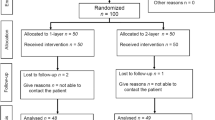
Operative results were examined based on medical records and questionnaire surveys in 340 consecutive cases of MKH performed at a single institution. The operation was performed with an original 3-stage dissection of the preperitoneal space only via the internal inguinal ring.
Results
The mean follow-up period was 50.5 ± 24.3 months. The mean operating time was 42.2 ± 13.1 min, and by Nyhus classification, significant difference was observed between types IIIA and IIIB (39.5 ± 10.8 vs. 45.6 ± 15.6 min, P = 0.0279). Eight surgeons performed 10 or more operations, and no significant difference was found in their operating time. Thirty-one patients used additional analgesics postoperatively (9.1 %) and the length of postoperative stay was 1.2 ± 0.7 days. Seven patients (2.1 %) developed complications related to the hernia operation, but none of them required re-operation. The period required to return to normal daily activities was 3 ± 3.2 days. Questionnaire forms were returned from 77.7 % of all the patients, in which 12 patients reported chronic pain (4.7 %). Visual analog scale for patients with chronic pain scored 3.8 ± 2.4, with no patient indicating restrictions on daily life. Recurrence was observed in only one case (0.3 %).
Conclusion
MKH using standardized dissection of the preperitoneal space is a highly reproducible procedure with acceptable rate of postoperative chronic pain and recurrence.




Similar content being viewed by others
References
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Franneby U, Sandblom G, Nordin P et al (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244:212–219
Bay-Nielsen M, Perkins FM, Kehlet H (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 233:1–7
Hair A, Duffy K, Mclean J et al (2000) Groin hernia repair in Scotland. Br J Surg 87:1722–1726
Aasvang EK, Bay-Nielsen M, Kehlet H (2006) Pain and functional impairment 6 years after inguinal herniorrhaphy. Hernia 10:316–321
Callesen T, Bech K, Kehlet H (1999) Prospective study of chronic pain after groin hernia repair. Br J Surg 86:1528–1531
Grant AM, Scott NW, O’Dwyer PJ, MRC Laparoscopic Groin Hernia Trial Group (2004) Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair of groin hernia. Br J Surg 91:1570–1574
Douek M, Smith G, Oshowo A et al (2003) Prospective randomized controlled trial of laparoscopic versus open inguinal hernia mesh repair: five year follow up. BMJ 326:1012–1013
Koninger J, Redecke J, Butters M (2004) Chronic pain after inguinal hernia repair: a randomized trial comparing Shouldice, Lichtenstein and TAPP. Langenbecks Arch Surg 389:361–365
Kumar S, Wilson RG, Nixon SJ, Macintyre MC (2002) Chronic pain after laparoscopic and open mesh repair of groin hernia. Br J Surg 89:1476–1479
Collaboration EH (2000) Laparoscopic compared with open methods of groin hernia repair: systematic review of randomized controlled trials. Br J Surg 87:860–867
Neumayer L, Giobbie-Hurder A, Jonasson O, Veterans Affairs Cooperative Studies Program 456 Investigators et al (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
Pavlidis TE (2010) Current option on laparoscopic repair of inguinal hernia. Surg Endosc 24:974–976
Grant AM (2002) Laparoscopic versus open groin hernia repair: meta-analysis of randomized trials based on individual patients data. Hernia 6:2–10
Pélissier EP (2006) Inguinal hernia: preperitoneal placement of a memory-ring patch by anterior approach. preliminary experience. Hernia 10:248–252
Li J, Zhang Y, Hu H, Tang W (2008) Early experience of performing a modified Kugel repair with local anesthesia. Surg Today 38:603–608
Li J, Zhang Y, Hu H, Tang W (2008) Preperitoneal groin hernia repair with Kugel patch through an anterior approach. ANZ J Surg 78:899–902
Stoppa R, Diarra B, Mertl P (1997) The retroparietal spermatic sheath—an anatomical structure of surgical interest. Hernia 1:55–59
Read CR (1992) Cooper’s posterior lamina of transversalis fascia. Surg Gynecol Obstet 174:426–434
Alfieri S, Amid PK, Campanelli G, Izard G, Kehlet H, Wijsmuller AR et al (2011) International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia 15:239–249
Stoppa R, Diarra B, Verhaeghe P, Henry X (1998) Some problems encountered at re-operation following repair of groin hernias with pre-peritoneal prosthesis. Hernia 2:35–38
Cooper AP (1804) The anatomy and surgical treatment of inguinal and congenital hernia. Longman, London
Mirilas P, Mentessidou A, Skandalakis JE (2008) Secondary internal inguinal ring and associated surgical planes: surgical anatomy, embryology, applications. J Am Coll Surg 206:561–570
Arregui ME (1997) Surgical anatomy of the preperitoneal fasciae and posterior transversalis fasciae in the inguinal region. Hernia 1:101–110
Usher FC, Fries JG, Ochsner JL, Tuttle LL Jr (1959) Marlex mesh, a new plastic mesh for replacing tissue defects. II: clinical studies. Arch Surg 78:138–145
Rives J (1967) Surgical treatment of the inguinal hernia with Dacron patch. Int Surg 47:360–361
Schroder DM, Lloyd LR, Boccaccio JE, Wesen CA (2004) Inguinal hernia recurrence following preperitoneal Kugel patch repair. Am Surg 70:132–136
Misawa T, Sakurai M, Kanai H, Matsushima M, Yamazaki Y, Yanaga K (2005) Kugel herniorrhaphy: clinical results of 124 consecutive operations. Surg Today 35:639–644
Maillart JF, Vantournhoudt P, Piret-Gerard G, Farghadani H, Mauel E (2011) Transinguinal preperitoneal groin hernia repair using a preperitoneal mesh performed with a permanent memory ring: a good alternative to Lichtenstein’s technique. Hernia 15:289–295
Pélissier EP, Blum D, Ngo Ph, Monek O (2008) Transinguinal preperitoneal repair with Polysoft patch: prospective evaluation of recurrence and chronic pain. Hernia 12:51–56
Grant AM (2002) Open mesh versus non-mesh repair of groin hernia meta-analysis of randomized trials based on individual patient data. Hernia 6:130–136
Berrevoet F, Sommeling C, De Gendt S, Breusegem C, de Hemptinne B (2009) The preperitoneal memory-ring patch for inguinal hernia: a prospective multicentric feasibility study. Hernia 13:243–249
Berrevoet F, Maes L, Reyntjens K, Rogiers X, Troisi R, de Hemptinne B (2010) Transinguinal preperitoneal memory ring patch versus Lichtenstein repair for unilateral inguinal hernias. Langenbecks Arch Surg 395:557–562
Koning GG, Koole D, de Jongh MACK, de Schipper JP, Verhofstad MHJ, Oostvogel HJM, Vriens PWHE (2011) The transinguinal preperitoneal hernia correction vs Lichtenstein’s technique; is TIPP top? Hernia 15:19–22
Bay-Nielsen M, Nordin P, Nilsson E, Kehlet H (2001) Operative findings in recurrent hernia after a Lichtenstein procedure. Am J Surg 182:134–136
Hollinsky C, Rusnov B, Hollinsky KH, Kohlberger PD (1999) Static tension measurements of inguinal hernia repair models. Hernia 3:11–14
Lowham AS, Filipi CJ, Fitzgibbons RJ et al (1997) Mechanism of hernia recurrence after preperitoneal mesh repair. Ann Surg 225:422–431
Felix E, Scott S, Crafton B et al (1998) Causes of recurrence after laparoscopic hernioplasty. Surg Endosc 12:226–231
Nienhuijs SW, van Oort I, Keemers-Gel ME, Strobbe LJA, Rosman C (2005) Randomized clinical trial comparing the prolene hernia system, mesh plug repair and Lichtenstein method for open inguinal hernia repair. Br J Surg 92:33–38
Heikkinen T, Bringman S, Ohtonen P, Kunelius P, Haukipuro K, Hulkko A (2004) Five-year outcome of laparoscopic and Lichtenstein hernioplasties. Surg Endosc 18:518–522
Schmedt CG, Sauerland S, Bittner R (2005) Comparison of endoscopic procedures versus Lichtenstein and other open mesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Surg Endosc 19:189–199
Lau H (2006) Day-case endoscopic totally extraperitoneal inguinal hernioplasty versus open Lichtenstein hernioplasty for unilateral primary inguinal hernia in males: a randomized trial. Surg Endosc 20:76–81
Lau H (2005) Fibrin sealant versus mechanical stapling for mesh fixation during endoscopic extraperitoneal inguinal hernioplasty: a randomized prospective trial. Ann Surg 242:670–675
Cunningham J, Temple W, Mitchell P, Nixon JA, Preshaw RM, Hagen NA (1996) Cooperative hernia study: pain in the post repair patient. Ann Surg 224:598–602
Gillion JF, Fagniez PL (1999) Chronic pain and cutaneous sensory changes after inguinal hernia repair: comparison between open and laparoscopic techniques. Hernia 3:75–80
Poobalan AS, Bruce J, King PM, Chambers WA, Krukowski ZH, Smith WCS (2001) Chronic pain and quality of life following open inguinal hernia repair. Br J Surg 88:1122–1126
Bay-Nielsen M, Nilsson E, Nordin P, Kehlet H, The Swedish Hernia Data Base (2004) Chronic pain after open mesh and sutured repair of indirect inguinal hernia in young males. Br J Surg 91:1372–1376
O’Dwyer PJ, Kingsnorth AN, Molloy RG, Small PK, Lammers B, Horeyseck G (2005) Randomized clinical trial assessing impact of a light weight or heavy weight mesh on chronic pain after inguinal hernia repair. Br J Surg 92:166–170
Sanjay P, Harris D, Jones P, Woodward A (2006) Randomized controlled trial comparing Prolene hernia system and Lichtenstein method for inguinal hernia repair. ANZ J Surg 76:548–552
Amid PK, Lichtenstein IL (1998) Long-term result and current status of the Lichtenstein open tension-free hernioplasty. Hernia 2:89–94
Acknowledgments
We thank Dr. Shintaro Sakurai of St. Luke’s International Hospital (Tokyo) for his valuable guidance in the fascial structure of the preperitoneal space.
Conflict of interest
KS, SN, KH, TS, TO and KY declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suwa, K., Nakajima, S., Hanyu, K. et al. Modified Kugel herniorrhaphy using standardized dissection technique of the preperitoneal space: long-term operative outcome in consecutive 340 patients with inguinal hernia. Hernia 17, 699–707 (2013). https://doi.org/10.1007/s10029-013-1132-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-013-1132-5