Abstract
Background
The aim of the present study was to evaluate whether different Nd:YAG laser applications as an adjunct to scaling and root planning (SRP) improve the healing response to periodontal therapy in smokers with periodontitis.
Methods
This clinical trial included eighty systemically healthy smokers with periodontitis. Patients were randomly allocated to a treatment group: SRP alone (group 1), SRP+low-level laser therapy (LLLT) with Nd:YAG laser (group 2), SRP+pocket debridement with ND:YAG laser (group 3), and SRP+combined pocket debridement and LLLT with Nd:YAG laser (group 4). Gingival index (GI), plaque index (PI), bleeding on probing (%), probing depth (PD), and clinical attachment level (CAL) were recorded, and gingival crevicular fluid (GCF) samples for metalloproteinase-8 (MMP-8) levels were collected at baseline, 1 month and 3 months after treatment.
Results
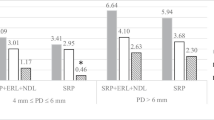
There were no significant differences between the treatment groups for the GI, PI, and BOP (%) parameters and MMP-8 levels at any time points (p > 0.05). For moderately deep pockets, PD and CAL reductions were significantly greater in all test groups compared to group 1 (p ˂ 0.05). For deep pockets, these reductions were significantly greater in group 2 and group 4 compared to group 1 (p ˂ 0.05). PD and CAL reductions were generally similar between test groups (p > 0.05) except PD reduction between baseline and 3 months in deep pockets (p ˂ 0.05).
Conclusions
The findings of this clinical trial suggest that Nd:YAG laser applications may be beneficial on the healing response of smokers to non-surgical therapy compared to SRP alone.

Similar content being viewed by others
References
Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F, Greenwell H, Herrera D, Kao RT, Kebschull M, Kinane DF, Kirkwood KL, Kocher T, Kornman KS, Kumar PS, Loos BG, Machtei E, Meng H, Mombelli A, Needleman I, Offenbacher S, Seymour GJ, Teles R, Tonetti MS (2018) Periodontitis: consensus report of workgroup 2 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J Periodontol 89(Suppl 1):S173–S182. https://doi.org/10.1002/JPER.17-0721
Bergstrom J, Preber H (1994) Tobacco use as a risk factor. J Periodontol 65(5):545–550. https://doi.org/10.1902/jop.1994.65.5.545
Grossi SG, Zambon JJ, Ho AW, Koch G, Dunford RG, Machtei EE, Norderyd OM, Genco RJ (1994) Assessment of risk for periodontal disease. I. Risk indicators for attachment loss. J Periodontol 65(3):260–267. https://doi.org/10.1902/jop.1994.65.3.260
Preber H, Bergstrom J (1986) Cigarette smoking in patients referred for periodontal treatment. Scand J Dent Res 94(2):102–108. https://doi.org/10.1111/j.1600-0722.1986.tb01372.x
Bergstrom J (1989) Cigarette smoking as risk factor in chronic periodontal disease. Community Dent Oral Epidemiol 17(5):245–247. https://doi.org/10.1111/j.1600-0528.1989.tb00626.x
Bergstrom J, Eliasson S (1987) Cigarette smoking and alveolar bone height in subjects with a high standard of oral hygiene. J Clin Periodontol 14(8):466–469. https://doi.org/10.1111/j.1600-051x.1987.tb02253.x
Grossi SG, Genco RJ, Machtei EE, Ho AW, Koch G, Dunford R, Zambon JJ, Hausmann E (1995) Assessment of risk for periodontal disease. II. Risk indicators for alveolar bone loss. J Periodontol 66(1):23–29. https://doi.org/10.1902/jop.1995.66.1.23
Holm G (1994) Smoking as an additional risk for tooth loss. J Periodontol 65(11):996–1001. https://doi.org/10.1902/jop.1994.65.11.996
Albandar JM, Streckfus CF, Adesanya MR, Winn DM (2000) Cigar, pipe, and cigarette smoking as risk factors for periodontal disease and tooth loss. J Periodontol 71(12):1874–1881. https://doi.org/10.1902/jop.2000.71.12.1874
Mullally BH, Linden GJ (1996) Molar furcation involvement associated with cigarette smoking in periodontal referrals. J Clin Periodontol 23(7):658–661. https://doi.org/10.1111/j.1600-051x.1996.tb00590.x
Axelsson P, Paulander J, Lindhe J (1998) Relationship between smoking and dental status in 35-, 50-, 65-, and 75-year-old individuals. J Clin Periodontol 25(4):297–305. https://doi.org/10.1111/j.1600-051x.1998.tb02444.x
Heitz-Mayfield LJ (2005) Disease progression: identification of high-risk groups and individuals for periodontitis. J Clin Periodontol 32(Suppl 6):196–209. https://doi.org/10.1111/j.1600-051X.2005.00803.x
Kibayashi M, Tanaka M, Nishida N, Kuboniwa M, Kataoka K, Nagata H, Nakayama K, Morimoto K, Shizukuishi S (2007) Longitudinal study of the association between smoking as a periodontitis risk and salivary biomarkers related to periodontitis. J Periodontol 78(5):859–867. https://doi.org/10.1902/jop.2007.060292
Mantyla P, Stenman M, Kinane D, Salo T, Suomalainen K, Tikanoja S, Sorsa T (2006) Monitoring periodontal disease status in smokers and nonsmokers using a gingival crevicular fluid matrix metalloproteinase-8-specific chair-side test. J Periodontal Res 41(6):503–512. https://doi.org/10.1111/j.1600-0765.2006.00897.x
Ogawa H, Yoshihara A, Hirotomi T, Ando Y, Miyazaki H (2002) Risk factors for periodontal disease progression among elderly people. J Clin Periodontol 29(7):592–597. https://doi.org/10.1034/j.1600-051x.2002.290702.x
Bergstrom J, Eliasson S, Dock J (2000) A 10-year prospective study of tobacco smoking and periodontal health. J Periodontol 71(8):1338–1347. https://doi.org/10.1902/jop.2000.71.8.1338
Norderyd O, Hugoson A, Grusovin G (1999) Risk of severe periodontal disease in a Swedish adult population. A longitudinal study. J Clin Periodontol 26(9):608–615. https://doi.org/10.1034/j.1600-051x.1999.260908.x
Preber H, Bergstrom J (1986) The effect of non-surgical treatment on periodontal pockets in smokers and non-smokers. J Clin Periodontol 13(4):319–323. https://doi.org/10.1111/j.1600-051x.1986.tb02229.x
Preber H, Linder L, Bergstrom J (1995) Periodontal healing and periopathogenic microflora in smokers and non-smokers. J Clin Periodontol 22(12):946–952. https://doi.org/10.1111/j.1600-051x.1995.tb01800.x
Preber H, Bergstrom J (1986) Effect of non-surgical treatment on gingival bleeding in smokers and non-smokers. Acta Odontol Scand 44(2):85–89. https://doi.org/10.3109/00016358609041312
Drisko CH (2001) Nonsurgical periodontal therapy. Periodontology 2000(25):77–88
Aoki A, Sasaki KM, Watanabe H, Ishikawa I (2004) Lasers in nonsurgical periodontal therapy. Periodontology 2000(36):59–97. https://doi.org/10.1111/j.1600-0757.2004.03679.x
Ishikawa I, Aoki A, Takasaki AA, Mizutani K, Sasaki KM (2000) Izumi Y (2009) Application of lasers in periodontics: true innovation or myth?. Periodontology 50:90–126. https://doi.org/10.1111/j.1600-0757.2008.00283.x
Cobb CM, Low SB, Coluzzi DJ (2010) Lasers and the treatment of chronic periodontitis. Dent Clin N Am 54(1):35–53. https://doi.org/10.1016/j.cden.2009.08.007
Parker S (2007) Lasers and soft tissue: periodontal therapy. Br Dent J 202(6):309–315. https://doi.org/10.1038/bdj.2007.224
White JM, Goodis HE, Rose CL (1991) Use of the pulsed Nd:YAG laser for intraoral soft tissue surgery. Lasers Surg Med 11(5):455–461. https://doi.org/10.1002/lsm.1900110511
White JM, Goodis HE, Cohen JN (1991) Bacterial reduction of contaminated dentin by Nd:YAG laser. J Dent Res 70:412
Ben Hatit Y, Blum R, Severin C, Maquin M, Jabro MH (1996) The effects of a pulsed Nd:YAG laser on subgingival bacterial flora and on cementum: an in vivo study. J Clin Laser Med Surg 14(3):137–143. https://doi.org/10.1089/clm.1996.14.137
Giannelli M, Bani D, Viti C, Tani A, Lorenzini L, Zecchi-Orlandini S, Formigli L (2012) Comparative evaluation of the effects of different photoablative laser irradiation protocols on the gingiva of periodontopathic patients. Photomed Laser Surg 30(4):222–230. https://doi.org/10.1089/pho.2011.3172
Qadri T, Poddani P, Javed F, Tuner J, Gustafsson A (2010) A short-term evaluation of Nd:YAG laser as an adjunct to scaling and root planing in the treatment of periodontal inflammation. J Periodontol 81(8):1161–1166. https://doi.org/10.1902/jop.2010.090700
Eltas A, Orbak R (2012) Effect of 1,064-nm Nd:YAG laser therapy on GCF IL-1beta and MMP-8 levels in patients with chronic periodontitis. Lasers Med Sci 27(3):543–550. https://doi.org/10.1007/s10103-011-0939-5
Qadri T, Tuner J, Gustafsson A (2015) Significance of scaling and root planing with and without adjunctive use of a water-cooled pulsed Nd:YAG laser for the treatment of periodontal inflammation. Lasers Med Sci 30(2):797–800. https://doi.org/10.1007/s10103-013-1432-0
Martelli FS, Fanti E, Rosati C, Martelli M, Bacci G, Martelli ML, Medico E (2016) Long-term efficacy of microbiology-driven periodontal laser-assisted therapy. European journal of clinical microbiology & infectious diseases : official publication of the European Society of Clinical Microbiology 35(3):423–431. https://doi.org/10.1007/s10096-015-2555-y
Eltas A, Orbak R (2012) Clinical effects of Nd:YAG laser applications during nonsurgical periodontal treatment in smoking and nonsmoking patients with chronic periodontitis. Photomed Laser Surg 30(7):360–366. https://doi.org/10.1089/pho.2011.3184
Gkogkos AS, Karoussis IK, Prevezanos ID, Marcopoulou KE, Kyriakidou K, Vrotsos IA (2015) Effect of Nd:YAG low level laser therapy on human gingival fibroblasts. Int J Dent 2015:258941. https://doi.org/10.1155/2015/258941
Prevezanos ID, Karoussis IK, Gkogkos AS, Marcopoulou KE, Kyriakidou K, Chernysheva A, Vrotsos IA (2018) Effect of Nd: YAG Low Level Laser Therapy on human periodontal ligament cells: A preliminary in-vitro study. Biomed J Sci Tech Res 2(4):2797–2802
Arisu HD, Turkoz E, Bala O (2006) Effects of Nd: Yag laser irradiation on osteoblast cell cultures. Lasers Med Sci 21(3):175–180. https://doi.org/10.1007/s10103-006-0398-6
Usumez A, Cengiz B, Oztuzcu S, Demir T, Aras MH, Gutknecht N (2014) Effects of laser irradiation at different wavelengths (660, 810, 980, and 1,064 nm) on mucositis in an animal model of wound healing. Lasers Med Sci 29(6):1807–1813. https://doi.org/10.1007/s10103-013-1336-z
Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F, Greenwell H, Herrera D, Kao RT, Kebschull M, Kinane DF, Kirkwood KL, Kocher T, Kornman KS, Kumar PS, Loos BG, Machtei E, Meng H, Mombelli A, Needleman I, Offenbacher S, Seymour GJ, Teles R, Tonetti MS (2018) Periodontitis: consensus report of workgroup 2 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. Journal Clin Periodontol 45(Suppl 20):S162–S170. https://doi.org/10.1111/jcpe.12946
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Periodontol 89(Suppl 1):S159–S172. https://doi.org/10.1002/JPER.18-0006
Kornman KS, Papapanou PN (2020) Clinical application of the new classification of periodontal diseases: Ground rules, clarifications and “gray zones.” J Periodontol 91(3):352–360. https://doi.org/10.1002/JPER.19-0557
Loe H (1967) The gingival index, the plaque index and the retention index systems. J Periodontol 38(6):610–616. https://doi.org/10.1902/jop.1967.38.6.610
Silness J, Loe H (1964) Periodontal disease in pregnancy. Ii. Correlation between Oral Hygiene and Periodontal Condtion. Acta Odontol Scand 22:121–135. https://doi.org/10.3109/00016356408993968
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25(4):229–235
Chellini F, Sassoli C, Nosi D, Deledda C, Tonelli P, Zecchi-Orlandini S, Formigli L, Giannelli M (2010) Low pulse energy Nd:YAG laser irradiation exerts a biostimulative effect on different cells of the oral microenvironment: an in vitro study. Lasers Surg Med 42(6):527–539. https://doi.org/10.1002/lsm.20861
Wang L, Wu F, Liu C, Song Y, Guo J, Yang Y, Qiu Y (2019) Low-level laser irradiation modulates the proliferation and the osteogenic differentiation of bone marrow mesenchymal stem cells under healthy and inflammatory condition. Lasers Med Sci 34(1):169–178. https://doi.org/10.1007/s10103-018-2673-8
Qadri T, Miranda L, Tuner J, Gustafsson A (2005) The short-term effects of low-level lasers as adjunct therapy in the treatment of periodontal inflammation. J Clin Periodontol 32(7):714–719. https://doi.org/10.1111/j.1600-051X.2005.00749.x
Aykol G, Baser U, Maden I, Kazak Z, Onan U, Tanrikulu-Kucuk S, Ademoglu E, Issever H, Yalcin F (2011) The effect of low-level laser therapy as an adjunct to non-surgical periodontal treatment. J Periodontol 82(3):481–488. https://doi.org/10.1902/jop.2010.100195
Saafan A, El-Nahass H, Nasr AS, Radwan R (2013) Effect of low power diode laser 810 nm on TGF-β1 level in GCF in aggressive periodontitis. J Dent Lasers 7(2):59–65
Ting CC, Fukuda M, Watanabe T, Sanaoka A, Mitani A, Noguchi T (2014) Morphological alterations of periodontal pocket epithelium following Nd:YAG laser irradiation. Photomed Laser Surg 32(12):649–657. https://doi.org/10.1089/pho.2014.3793
Yukna RA, Carr RL, Evans GH (2007) Histologic evaluation of an Nd:YAG laser-assisted new attachment procedure in humans. Int J Periodontics Restorative Dent 27(6):577–587
Fukuda M, Minoura S, Ishikawa K, Ogura N, Ueda N, Murase M, Sugihara N, Kato K, Nakagaki H, Noguchi T (1994) Effects of Nd:YAG laser irradiation on endotoxin in exposed cementum [in Japanese, English abstract]. Jpn J Conserv Dent 37:711–716
Abduljabbar T, Vohra F, Kellesarian SV, Javed F (2017) Efficacy of scaling and root planning with and without adjunct Nd:YAG laser therapy on clinical periodontal parameters and gingival crevicular fluid interleukin 1-beta and tumor necrosis factor-alpha levels among patients with periodontal disease: a prospective randomized split-mouth clinical study. J Photochem Photobiol B Biol 169:70–74. https://doi.org/10.1016/j.jphotobiol.2017.03.001
Gomez C, Dominguez A, Garcia-Kass AI, Garcia-Nunez JA (2011) Adjunctive Nd:YAG laser application in chronic periodontitis: clinical, immunological, and microbiological aspects. Lasers Med Sci 26(4):453–463. https://doi.org/10.1007/s10103-010-0795-8
Slot DE, Kranendonk AA, Van der Reijden WA, Van Winkelhoff AJ, Rosema NA, Schulein WH, Van der Velden U, Van der Weijden FA (2011) Adjunctive effect of a water-cooled Nd:YAG laser in the treatment of chronic periodontitis. J Clin Periodontol 38(5):470–478. https://doi.org/10.1111/j.1600-051X.2010.01695.x
Radvar M, MacFarlane TW, MacKenzie D, Whitters CJ, Payne AP, Kinane DF (1996) An evaluation of the Nd:YAG laser in periodontal pocket therapy. Br Dent J 180(2):57–62. https://doi.org/10.1038/sj.bdj.4808976
Maden I (2009) Effects of Nd:YAG laser treatment as an adjunct to conventional periodontal therapy [PhD Thesis]. Istanbul: Istanbul University;:113p
Cobb CM (2006) Lasers in periodontics: a review of the literature. J Periodontol 77(4):545–564. https://doi.org/10.1902/jop.2006.050417
Petrovic MS, Kannosh IY, Milasin JM, Mihailovic DS, Obradovic RR, Bubanj SR, Kesic LG (2018) Clinical, microbiological and cytomorphometric evaluation of low-level laser therapy as an adjunct to periodontal therapy in patients with chronic periodontitis. Int J Dent Hyg 16(2):e120–e127. https://doi.org/10.1111/idh.12328
Morlock BJ, Pippin DJ, Cobb CM, Killoy WJ, Rapley JW (1992) The effect of Nd:YAG laser exposure on root surfaces when used as an adjunct to root planing: an in vitro study. J Periodontol 63(7):637–641. https://doi.org/10.1902/jop.1992.63.7.637
Acknowledgements
We would like to thank Assoc. Prof. Ferhan Elmalı for his statistical assistance.
Funding
This study was funded by The Scientific Research Coordination Office of Izmir Katip Çelebi University (2017-TDU-DİŞF-0034).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures in this study were approved by the Ethics Committee of Izmir Katip Celebi University for human subjects (2017/106) and also the Republic of Turkey Ministry of Health, Turkey Pharmaceuticals and Medical Devices Agency (No: 71146310-511.06-E.213417 Subject: 2017-102). Clinical trial serial number: TCTR20190926001.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ezber, A., Taşdemir, İ., Yılmaz, H.E. et al. Different application procedures of Nd:YAG laser as an adjunct to scaling and root planning in smokers with stage III grade C periodontitis: a single-blind, randomized controlled trial. Ir J Med Sci 192, 457–466 (2023). https://doi.org/10.1007/s11845-022-02940-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-022-02940-z