Abstract
Objectives
To compare the treatment response and prognosis of oral cavity cancer between non-smoking and non-alcohol-drinking (NSND) patients and smoking and alcohol-drinking (SD) patients.
Methods
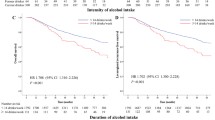
A total of 313 consecutively treated patients from 2000 to 2019 were included. Demographic, clinicopathologic, treatment, and prognosis information were obtained. Relapse-free survival (RFS), disease-specific survival (DSS), and overall survival (OS) were compared between NSND and SD groups using Kaplan-Meier plots, log-rank test, and multivariate Cox regression analysis.
Results
Sample prevalence of NSND patients was 54.6%. These patients were predominantly females in their eighth decade with lower prevalence of floor of the mouth cancers compared to SD patients (1.8% vs 14.8%). No difference in the RFS and DSS between both groups was found following multivariable analysis; however, NSND patients had better OS (HR (95% CI) − 0.47 (0.29–0.75); p = 0.002). Extracapsular extension was associated with significantly poorer OS, DSS, and RFS in this oral cavity cancer cohort.
Conclusion
Treatment response and disease-specific prognosis are comparable between NSND and SD patients with oral cavity cancer. However, NSND patients have better OS.
Clinical relevance
This study shows that oral cavity cancer in NSND is not less or more aggressive compared to SD patients. Although better survival is expected for NSND than SD patients, this is likely due to the reduced incidence of other chronic diseases in the NSND group.

Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Warnakulasuriya S (2009) Global epidemiology of oral and oropharyngeal cancer. Oral Oncol 45(4-5):309–316
Adeoye J, Thomson P (2020) Strategies to improve diagnosis and risk assessment for oral cancer patients. Fac Dent J 11(3):122–127
Dahlstrom KR, Little JA, Zafereo ME, Lung M, Wei Q, Sturgis EM (2008) Squamous cell carcinoma of the head and neck in never smoker-never drinkers: a descriptive epidemiologic study. Head Neck 30(1):75–84
DeAngelis A, Breik O, Koo K, Iseli T, Nastri A, Fua T, Rischin D, McCullough M, Wiesenfeld D (2018) Non-smoking, non-drinking elderly females, a 5 year follow-up of a clinically distinct cohort of oral squamous cell carcinoma patients. Oral Oncol 86:113–120
Harris SL, Kimple RJ, Hayes DN, Couch ME, Rosenman JG (2010) Never-smokers, never-drinkers: unique clinical subgroup of young patients with head and neck squamous cell cancers. Head Neck 32(4):499–503
Koo K, Barrowman R, McCullough M, Iseli T, Wiesenfeld D (2013) Non-smoking non-drinking elderly females: a clinically distinct subgroup of oral squamous cell carcinoma patients. Int J Oral Maxillofac Surg 42(8):929–933
Moyses RA, Lopez RVM, Cury PM, Siqueira SA, Curioni OA, Gois Filho JF, Figueiredo DL, GENCAPO, Tajara EH, Michaluart Jr P (2013) Significant differences in demographic, clinical, and pathological features in relation to smoking and alcohol consumption among 1,633 head and neck cancer patients. Clinics. 68(6):738–744
Montero PH, Patel PD, Palmer FL, Patel SG, Shah JP, Hayes RB, Ganly I (2012) Changing trends in smoking and alcohol consumption in patients with oral cancer treated at Memorial Sloan-Kettering Cancer Center from 1985 to 2009. Arch Otolaryngol Head Neck Surg 138(9):817–822
Kruse AL, Bredell M, Luebbers HT, Grätz KW (2010) Head and neck cancer in the elderly: a retrospective study over 10 years (1999 - 2008). Head Neck Oncol 2:25
Brennan K, Koenig JL, Gentles AJ, Sunwoo JB, Gevaert O (2017) Identification of an atypical etiological head and neck squamous carcinoma subtype featuring the CpG island methylator phenotype. EBioMedicine. 17:223–236
Dediol E, Sabol I, Virag M, Grce M, Muller D, Manojlović S (2016) HPV prevalence and p16INKa overexpression in non-smoking non-drinking oral cavity cancer patients. Oral Dis 22(6):517–522
Rikardsen OG, Bjerkli IH, Uhlin-Hansen L, Hadler-Olsen E, Steigen SE (2014) Clinicopathological characteristics of oral squamous cell carcinoma in Northern Norway: a retrospective study. BMC Oral Health 14:103
Koo K, Mouradov D, Angel CM, Iseli TA, Wiesenfeld D, McCullough MJ, Burgess AW, Sieber OM (2021) Genomic signature of oral squamous cell carcinomas from non-smoking non-drinking patients. Cancers. 13(5):1029
Foy JP, Bertolus C, Michallet MC, Deneuve S, Incitti R, Bendriss-Vermare N, Albaret MA, Ortiz-Cuaran S, Thomas E, Colombe A, Py C, Gadot N, Michot JP, Fayette J, Viari A, van den Eynde B, Goudot P, Devouassoux-Shisheboran M, Puisieux A, Caux C, Zrounba P, Lantuejoul S, Saintigny P (2017) The immune microenvironment of HPV-negative oral squamous cell carcinoma from never-smokers and never-drinkers patients suggests higher clinical benefit of IDO1 and PD1/PD-L1 blockade. Ann Oncol 28(8):1934–1941
Lenouvel D, González-Moles MÁ, Ruiz-Ávila I, Chamorro-Santos C, González-Ruiz L, González-Ruiz I, Ramos-García P (2021) Clinicopathological and prognostic significance of PD-L1 in oral cancer: a preliminary retrospective immunohistochemistry study. Oral Dis 27(2):173–182
Bachar G, Hod R, Goldstein DP, Irish JC, Gullane PJ, Brown D, Gilbert RW, Hadar T, Feinmesser R, Shpitzer T (2011) Outcome of oral tongue squamous cell carcinoma in patients with and without known risk factors. Oral Oncol 47(1):45–50
Lee SU, Moon SH, Choi SW, Cho KH, Park JY, Jung YS, Ryu J, Ryu CH, Yun T, Kim TH, Youn SH, Oh ES (2020) Prognostic significance of smoking and alcohol history in young age oral cavity cancer. Oral Dis 26(7):1440–1448
Bao X, Liu F, Chen Q, Chen L, Lin J, Chen F, Wang J, Qiu Y, Shi B, Pan L, Lin L, He B (2020) Propensity score analysis exploring the impact of smoking and drinking on the prognosis of patients with oral cancer. Head Neck 42(8):1837–1847
Adelstein D, Gillison ML, Pfister DG, Spencer S, Adkins D, Brizel DM, Burtness B, Busse PM, Caudell JJ, Cmelak AJ, Colevas AD, Eisele DW, Fenton M, Foote RL, Gilbert J, Haddad RI, Hicks WL Jr, Hitchcock YJ, Jimeno A, Leizman D, Lydiatt WM, Maghami E, Mell LK, Mittal BB, Pinto HA, Ridge JA, Rocco J, Rodriguez CP, Shah JP, Weber RS, Witek M, Worden F, Yom SS, Zhen W, Burns JL, Darlow SD (2017) NCCN guidelines insights: head and neck cancers, version 2.2017. J Natl Compr Cancer Netw 15(6):761–770
Almangush A, Mäkitie AA, Triantafyllou A, de Bree R, Strojan P, Rinaldo A, Hernandez-Prera JC, Suárez C, Kowalski LP, Ferlito A, Leivo I (2020) Staging and grading of oral squamous cell carcinoma: An update. Oral Oncol 107:104799
Fan Y, Zheng L, Mao MH, Huang MW, Liu SM, Zhang J, Li SL, Zheng L, Zhang JG (2014) Survival analysis of oral squamous cell carcinoma in a subgroup of young patients. Asian Pac J Cancer Prev 15(20):8887–8891
Farshadpour F, Roepman P, Hordijk GJ, Koole R, Slootweg PJ (2012) A gene expression profile for non-smoking and non-drinking patients with head and neck cancer. Oral Dis 18(2):178–183
Wiseman SM, Swede H, Stoler DL, Anderson GR, Rigual NR, Hicks WL Jr, Douglas WG, Tan D, Loree TR (2003) Squamous cell carcinoma of the head and neck in nonsmokers and nondrinkers: an analysis of clinicopathologic characteristics and treatment outcomes. Ann Surg Oncol 10(5):551–557
Albuquerque R, López-López J, Marí-Roig A, Jané-Salas E, Roselló-Llabrés X, Santos JR (2011) Oral tongue squamous cell carcinoma (OTSCC): alcohol and tobacco consumption versus non-consumption. A study in a Portuguese population. Braz Dent J 22(6):517–521
Farshadpour F, Hordijk GJ, Koole R, Slootweg PJ (2007) Non-smoking and non-drinking patients with head and neck squamous cell carcinoma: a distinct population. Oral Dis 13(2):239–243
Adeoye J, Thomson P, Choi S-W (2020) Prognostic significance of multi-positive invasive histopathology in oral cancer. J Oral Pathol Med 49(10):1004–1010
Choi S-W, Thomson P (2019) Increasing incidence of oral cancer in Hong Kong—Who, where…and why? J Oral Pathol Med 48(6):483–490
Thomson PJ (2002) Field change and oral cancer: new evidence for widespread carcinogenesis? Int J Oral Maxillofac Surg 31(3):262–266
Shah JP, Batsakis JG, Johnson NW (2003) Oral cancer. London, Martin Dunitz
Lin CS, Jen YM, Cheng MF, Lin YS, Su WF, Hwang JM, Chang LP, Chao HL, Liu DW, Lin HY, Shum WY (2006) Squamous cell carcinoma of the buccal mucosa: an aggressive cancer requiring multimodality treatment. Head Neck 28(2):150–157
Wang W, Adeoye J, Thomson P, Choi SW (2021) Statistical profiling of oral cancer and the prediction of outcome. J Oral Pathol Med 50(1):39–46
Lubek JE, Dyalram D, Perera EH et al (2013) A retrospective analysis of squamous carcinoma of the buccal mucosa: an aggressive subsite within the oral cavity. J Oral Maxillofac Surg 71(6):1126–1131
Zhang Y, He J, He B et al (2019) Effect of tobacco on periodontal disease and oral cancer. Tob Induc Dis 17:40
Foy JP, Bertolus C, Boutolleau D, Agut H, Gessain A, Herceg Z, Saintigny P (2020) Arguments to support a viral origin of oral squamous cell carcinoma in non-smoker and non-drinker patients. Front Oncol 10:822
Campisi G, Calvino F, Carinci F, Matranga D, Carella M, Mazzotta M, Rubini C, Panzarella V, Santarelli A, Fedele S, Lo Muzio L (2011) Peri-tumoral inflammatory cell infiltration in OSCC: a reliable marker of local recurrence and prognosis? An investigation using artificial neural networks. Int J Immunopathol Pharmacol 24(2 Suppl):113–120
Hongli Z, Bi X, Zheng N, Li C, Yan K (2021) Joint effect of alcohol drinking and tobacco smoking on all-cause mortality and premature death in China: a cohort study. PLoS One 16(1):e0245670
Alkhadar H, Macluskey M, White S, Ellis I, Gardner A (2021) Comparison of machine learning algorithms for the prediction of five-year survival in oral squamous cell carcinoma. J Oral Pathol Med 50(4):378–384
Department of Health HKSAR Government (2008) Promoting health in Hong Kong: a strategic framework for prevention and control of non-communicable diseases. Available from: https://www.dh.gov.hk/english/pub_rec/pub_rec_ar/pdf/ncd/ENGwholeDOC16-10-08.pdf. Accessed 5 Feb 2021
Warnakulasuriya S, Greenspan JS (2020) Textbook of oral cancer: prevention, diagnosis and management. Springer, Cham
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Approval to conduct this study was granted by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (Reference number UW-19-704). All clinical data were anonymized by the researchers, and all potential patient identifiers were removed before data analysis.
Informed consent
For this type of study, formal consent is not required.
Conflict of interest
JA declares that he has no conflict of interest. LH declares that she has no conflict of interest. JYT declares that she has no conflict of interest. MK-M declares that he has no conflict of interest. S-WC declares that she has no conflict of interest. PT declares that he has no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 2484 kb)
Rights and permissions
About this article
Cite this article
Adeoye, J., Hui, L., Tan, J.Y. et al. Prognostic value of non-smoking, non-alcohol drinking status in oral cavity cancer. Clin Oral Invest 25, 6909–6918 (2021). https://doi.org/10.1007/s00784-021-03981-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03981-x



