Abstract
Objectives
With the higher risk of dental implant failure with type 2 diabetes mellitus (T2DM), there is a need to characterize the jaw bones in those individuals. The aim of this post mortem study was to compare jaw bone quality of individuals with T2DM to healthy controls.
Material and methods
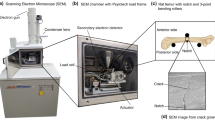
Bone cores from the edentulous lower first molar region and the region of mandibular angle were collected from male individuals with T2DM (n = 10, 70.6 ± 4.5 years) and healthy controls (n = 11, 71.5 ± 3.8 years) during autopsy. Within the T2DM, a subgroup treated with oral antidiabetics (OAD) and one on insulin were identified. Bone quality assessment encompassed evaluation of bone microstructure, matrix composition, and cellular activity, using microcomputed tomography (micro-CT), quantitative backscattered electron imaging (qBEI), Raman spectroscopy, and bone histomorphometry.
Results
In the mandibular angle, T2DM showed 51% lower porosity of the lingual cortex (p = 0.004) and 21% higher trabecular thickness (p = 0.008) compared to control. More highly mineralized bone packets were found in the buccal cortex of the mandibular angle in insulin-treated compared to OAD-treated T2DM group (p = 0.034). In the molar region, we found higher heterogeneity of trabecular calcium content in T2DM insulin compared to controls (p = 0.015) and T2DM OAD (p = 0.019). T2DM was associated with lower osteocyte lacunar size in the trabecular bone of the molar region (vs. control p = 0.03).
Conclusions
Alterations in microstructure, mineralization, and osteocyte morphology were determined in jaw bone of individuals with T2DM compared to controls.
Clinical relevance
Future studies will have to verify if the mild changes determined in this study will translate to potential contraindications for dental implant placements.











Similar content being viewed by others
References
WHO: Global Report on Diabetes 2017; NCD-RisC https://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf;jsessionid=A3890983DA4DA8727ABC73AD6167E736?sequence=1. Accessed Nov 2019
NCD Risk Factor Collaboration (NCD-RisC) (2016) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 387(10027):1513–1530. https://doi.org/10.1016/S0140-6736(16)00618-8
Naujokat H, Kunzendorf B, Wiltfang J (2016) Dental implants and diabetes mellitus-a systematic review. Int J Implant Dent 2(1):5. https://doi.org/10.1186/s40729-016-0038-2
Ward NH III, Wainwright DJ (2015) Outcomes research: mandibular fractures in the diabetic population. J Cranio-Maxillofac Surg 44:763–769. https://doi.org/10.1016/j.jcms.2015.09.001
Chrcanovic BR (2014) Fixation of mandibular angle fractures: Clinical studies. Oral Maxillofac Surg 18(2):123–152. https://doi.org/10.1007/s10006-012-0374-1
Kudiyirickal MG, Pappachan JM (2015) Diabetes mellitus and oral health. Endocrine. 49(1):27–34. https://doi.org/10.1007/s12020-014-0496-3
Singh R, Parihar AS, Vaibhav V, Kumar K, Singh R, Jerry JJ (2020) A 10 years retrospective study of assessment of prevalence and risk factors of dental implants failures. J Family Med Prim Care 9:1617–1619
Chrcanovic BR, Albrektsson T, Wennerberg A (2014) Diabetes and oral implant failure: a systematic review. J Dent Res 93(9):859–867. https://doi.org/10.1177/0022034514538820
Castellanos-Cosano L, Rodriguez-Perez A, Spinato S, Wainwright M, Machuca-Portillo G, Serrera-Figallo MA, Torres-Lagares D (2019) Descriptive retrospective study analyzing relevant factors related to dental implant failure. Med Oral Patol Oral Cir Bucal 24(6):e726–e738. https://doi.org/10.4317/medoral.23082
Marchand F, Raskin A, Dionnes-Hornes A, Barry T, Dubois N, Valéro R, Vialettes B (2012) Dental implants and diabetes: conditions for success. Diabetes Metab 38(1):14–19. https://doi.org/10.1016/j.diabet.2011.10.002
Aguilar-Salvatierra A, Calvo-Guirado JL, González-Jaranay M, Moreu G, Delgado-Ruiz RA, Gómez-Moreno G (2016) Peri-implant evaluation of immediately loaded implants placed in esthetic zone in patients with diabetes mellitus type 2: a two-year study. Clin Oral Implants Res 27(2):156–161. https://doi.org/10.1111/clr.12552
Eskow CC, Oates TW (2017) Dental implant survival and complication rate over 2 years for individuals with poorly controlled type 2 diabetes mellitus. Clin Implant Dent Relat Res 19(3):423–431. https://doi.org/10.1111/cid.12465
Oates TW Jr, Galloway P, Alexander P, Vargas Green A, Huynh-Ba G, Feine J, McMahan CA (2014) The effects of elevated hemoglobin A(1c) in patients with type 2 diabetes mellitus on dental implants: survival and stability at one year. J Am Dent Assoc 145(12):1218–1226. https://doi.org/10.14219/jada.2014.93
Alsaadi G, Quirynen M, Komárek A, van Steenberghe D (2008) Impact of local and systemic factors on the incidence of late oral implant loss. Clin Oral Implants Res 19(7):670–676. https://doi.org/10.1111/j.1600-0501.2008.01534.x
Peled M, Ardekian L, Tagger-Green N, Gutmacher Z, Machtei EE (2003) Dental implants in patients with type 2 diabetes mellitus: a clinical study. Implant Dent 12(2):116–122. https://doi.org/10.1097/01.id.0000058307.79029.b1
Parihar AS, Madhuri S, Devanna R, Sharma G, Singh R, Shetty K (2020) Assessment of failure rate of dental implants in medically compromised patients. J Family Med Prim Care 9:883–885. https://doi.org/10.4103/jfmpc.jfmpc_989_19
Smeets R, Henningsen A, Jung O, Heiland M, Hammächer C, Stein JM (2014) Definition, etiology, prevention and treatment of peri-implantitis--a review. Head Face Med 10:34. https://doi.org/10.1186/1746-160X-10-34
Oates TW, Huynh-Ba G, Vargas A, Alexander P, Feine J (2013) A critical review of diabetes, glycemic control, and dental implant therapy. Clin Oral Implants Res 24(2):117–127. https://doi.org/10.1111/j.1600-0501.2011.02374.x
Saito M, Kida Y, Kato S, Marumo K (2014) Diabetes, collagen, and bone quality. Curr Osteoporos Rep 12(2):181–188. https://doi.org/10.1007/s11914-014-0202-7
Palermo A, D'Onofrio L, Buzzetti R, Manfrini S, Napoli N (2017) Pathophysiology of bone fragility in patients with diabetes. Calcif Tissue Int 100(2):122–132. https://doi.org/10.1007/s00223-016-0226-3
Napoli N, Chandran M, Pierroz DD, Abrahamsen B, Schwartz AV, Ferrari SL (2017) IOF bone and diabetes working group. Mechanisms of diabetes mellitus-induced bone fragility. Nat Rev Endocrinol 13(4):208–219. https://doi.org/10.1038/nrendo.2016.153
Picke AK, Campbell G, Napoli N, Hofbauer LC, Rauner M (2019) Update on the impact of type 2 diabetes mellitus on bone metabolism and material properties. Endocr Connect 8(3):R55–R70. https://doi.org/10.1530/EC-18-0456
Wu YY, Xiao E, Graves DT (2015) Diabetes mellitus related bone metabolism and periodontal disease. Int J Oral Sci 7(2):63–72. https://doi.org/10.1038/ijos.2015.2
Milovanovic P, Zimmermann EA, Riedel C, vom Scheidt A, Herzog L, Krause M, Djonic D, Djuric M, Püschel K, Amling M, Ritchie RO, Busse B (2015) Multi-level characterization of human femoral cortices and their underlying osteocyte network reveal trends in quality of young, aged, osteoporotic and antiresorptive-treated bone. Biomaterials. 45:46–55. https://doi.org/10.1016/j.biomaterials.2014.12.024
Ferrato G, Falisi G, Ierardo G, Polimeni A, Di Paolo C (2017) Digital evaluation of occlusal forces: comparison between healthy subjects and TMD patients. Ann Stomatol (Roma) 8(2):79–88. https://doi.org/10.11138/ads/2017.8.2.089
Alrabiah M, Al-Aali KA, Al-Sowygh ZH, Binmahfooz AM, Mokeem SA, Abduljabbar T (2018) Association of advanced glycation end products with peri-implant inflammation in prediabetes and type 2 diabetes mellitus patients. Clin Implant Dent Relat Res 20(4):535–540. https://doi.org/10.1111/cid.12607
Javid AZ, Hormoznejad R, Yousefimanesh HA, Haghighi-Zadeh MH, Zakerkish M (2019) Impact of resveratrol supplementation on inflammatory, antioxidant, and periodontal markers in type 2 diabetic patients with chronic periodontitis. Diabetes Metab Syndr 13(4):2769–2774. https://doi.org/10.1016/j.dsx.2019.07.042
Mauri-Obradors E, Merlos A, Estrugo-Devesa A, Jané-Salas E, López-López J, Viñas M (2018) Benefits of non-surgical periodontal treatment in patients with type 2 diabetes mellitus and chronic periodontitis: a randomized controlled trial. J Clin Periodontol 45(3):345–353. https://doi.org/10.1111/jcpe.12858
Kurşun-Çakmak EŞ, Bayrak S (2018) Comparison of fractal dimension analysis and panoramic-based radiomorphometric indices in the assessment of mandibular bone changes in patients with type 1 and type 2 diabetes mellitus. Oral Surg Oral Med Oral Pathol Oral Radiol 126(2):184–191. https://doi.org/10.1016/j.oooo.2018.04.010
Nemtoi A, Ladunca O, Dragan E, Budacu C, Mihai C, Haba D (2013) Quantitative and qualitative bone assessment of the posterior mandible in patients with diabetes mellitus: a cone beam computed tomography study. Rev Med Chir Soc Med Nat Iasi 117(4):1002–1008
Bulut E, Baş B, Altunkaynak BZ, Bekçioğlu B, Erdem Koç G, Gönülol E, Önger ME, Kaplan S (2014) Efficacy of Ankaferd Blood Stopper on bone healing in diabetic rats: a stereological and histopathological study. Biotech Histochem 89(7):535–543. https://doi.org/10.3109/10520295.2014.906657
Akyol UK, Güngörmüş M (2010) Effect of biostimulation on healing of bone defects in diabetic rats. Photomed Laser Surg 28(3):411–416. https://doi.org/10.1089/pho.2008.2478
von Wilmowsky C, Schlegel KA, Baran C, Nkenke E, Neukam FW, Moest T (2016) Peri-implant defect regeneration in the diabetic pig: a preclinical study. J Craniomaxillofac Surg 44(7):827–834. https://doi.org/10.1016/j.jcms.2016.04.002
Goss AN, Sambrook PJ (2013) Diabetes, wound healing and complications: authors’ reply. Aust Dent J 58(4):536–537. https://doi.org/10.1111/adj.12117_2
Guja C, Guja L, Miulescu RD (2019) Effect of type 2 diabetes medications on fracture risk. Ann Transl Med 7(20):580. https://doi.org/10.21037/atm.2019.09.51
Huang S, Dang H, Huynh W, Sambrook PJ, Goss AN (2013) The healing of dental extraction sockets in patients with type 2 diabetes on oral hypoglycaemics: a prospective cohort. Aust Dent J 58(1):89–93. https://doi.org/10.1111/adj.12029
Power DJ, Sambrook PJ, Goss AN (2019) The healing of dental extraction sockets in insulin-dependent diabetic patients: a prospective controlled observational study. Aust Dent J 64(1):111–116. https://doi.org/10.1111/adj.12669
Pietschmann P, Patsch JM, Schernthaner G (2010) Diabetes and bone. Horm Metab Res 42(11):763–768. https://doi.org/10.1055/s-0030-1262825
Murray CE, Coleman CM (2019) Impact of diabetes mellitus on bone health. Int J Mol Sci 20(19):4873. Published 2019 Sep 30. https://doi.org/10.3390/ijms20194873
Achemlal L, Tellal S, Rkiouak F, Nouijai A, Bezza A, Derouiche EM, Ghafir D, el Maghraoui A (2005) Bone metabolism in male patients with type 2 diabetes. Clin Rheumatol 24(5):493–496. https://doi.org/10.1007/s10067-004-1070-9
Pacios S, Andriankaja O, Kang J, Alnammary M, Bae J, de Brito Bezerra B, Schreiner H, Fine DH, Graves DT (2013) Bacterial infection increases periodontal bone loss in diabetic rats through enhanced apoptosis. Am J Pathol 183(6):1928–1935. https://doi.org/10.1016/j.ajpath.2013.08.017
Yamagishi S (2012) Potential clinical utility of advanced glycation end product cross-link breakers in age- and diabetes-associated disorders. Rejuvenation Res 15(6):564–572. https://doi.org/10.1089/rej.2012.1335
Kasahara T, Imai S, Kojima H, Katagi M, Kimura H, Chan L, Matsusue Y (2010) Malfunction of bone marrow-derived osteoclasts and the delay of bone fracture healing in diabetic mice. Bone. 47(3):617–625. https://doi.org/10.1016/j.bone.2010.06.014
Wittrant Y, Gorin Y, Woodruff K, Horn D, Abboud HE, Mohan S, Abboud-Werner SL (2008) High d(+)glucose concentration inhibits RANKL-induced osteoclastogenesis. Bone. 42(6):1122–1130. https://doi.org/10.1016/j.bone.2008.02.006
He B, Li SQ, Wang W, Han P (2004) [Maternal serum lipid at 36-42 weeks’ gestation and their relationship to newborn weight in pregnant women with gestational diabetes mellitus and type 1 and type 2 diabetes mellitus]. Zhonghua Fu Chan Ke Za Zhi 39(10):675–677 (Chinese)
Thrailkill KM, Lumpkin CK Jr, Bunn RC, Kemp SF, Fowlkes JL (2005) Is insulin an anabolic agent in bone? Dissecting the diabetic bone for clues. Am J Physiol Endocrinol Metab 289(5):E735–E745. https://doi.org/10.1152/ajpendo.00159.2005
Tomczyk S, Whitten T, Holzbauer SM, Lynfield R (2018) Combating antibiotic resistance: a survey on the antibiotic-prescribing habits of dentists. Gen Dent 66(5):61–68
Sella-Tunis T, Pokhojaev A, Sarig R, O'Higgins P, May H (2018) Human mandibular shape is associated with masticatory muscle force. Sci Rep 8(1):6042. https://doi.org/10.1038/s41598-018-24293-3
Roschger P, Paschalis EP, Fratzl P, Klaushofer K (2008) Bone mineralization density distribution in health and disease. Bone. 42(3):456–466. https://doi.org/10.1016/j.bone.2007.10.021
Image J referenceSchneider CA, Rasband WS, Eliceiri KW (2012) NIH image to ImageJ: 25 years of image analysis. Nat Methods 9:671–675. https://doi.org/10.1038/nmeth.2089
Dempster DW, Compston JE, Drezner MK, Glorieux FH, Kanis JA, Malluche H, Meunier PJ, Ott SM, Recker RR, Parfitt AM (2013) Standardized nomenclature, symbols, and units for bone histomorphometry: a 2012 update of the report of the ASBMR Histomorphometry nomenclature committee. J Bone Miner Res 28(1):2–17. https://doi.org/10.1002/jbmr.1805
Bernhard A, Milovanovic P, Zimmermann EA, Hahn M, Djonic D, Krause M, Breer S, Püschel K, Djuric M, Amling M, Busse B (2013) Micro-morphological properties of osteons reveal changes in cortical bone stability during aging, osteoporosis, and bisphosphonate treatment in women. Osteoporos Int 24(10):2671–2680. https://doi.org/10.1007/s00198-013-2374-x
Shah FA, Sayardoust S, Thomsen P, Palmquist A (2019) Extracellular matrix composition during bone regeneration in the human dental alveolar socket. Bone. 127:244–249. https://doi.org/10.1016/j.bone.2019.06.003
Marin S, Popovic-Pejicic S, Radosevic-Caric B, Trtić N, Tatic Z, Selakovic S (2020) Hyaluronic acid treatment outcome on the post-extraction wound healing in patients with poorly controlled type 2 diabetes: a randomized controlled split-mouth study. Med Oral Patol Oral Cir Bucal 25(2):e154–e160. https://doi.org/10.4317/medoral.23061
Liu R, Bal HS, Desta T, Krothapalli N, Alyassi M, Luan Q, Graves DT (2006) Diabetes enhances periodontal bone loss through enhanced resorption and diminished bone formation. J Dent Res 85:510–514. https://doi.org/10.1177/154405910608500606
Pacios S, Kang J, Galicia J, Gluck K, Patel H, Ovaydi-Mandel A, Petrov S, Alawi F, Graves DT (2012) Diabetes aggravates periodontitis by limiting repair through enhanced inflammation. FASEB J 26:1423–1430. https://doi.org/10.1096/fj.11-196279
Xiao E, Mattos M, Vieira GHA, Chen S, Correa JD, Wu Y, Albiero ML, Bittinger K, Graves DT (2017) Diabetes enhances IL-17 expression and alters the oral microbiome to increase its pathogenicity. Cell Host Microbe 22:120–128. https://doi.org/10.1016/j.chom.2017.06.014
Yamamoto M, Yamaguchi T, Nawata K, Yamauchi M, Sugimoto T (2012) Decreased PTH levels accompanied by low bone formation are associated with vertebral fractures in postmenopausal women with type 2 diabetes. J Clin Endocrinol Metab 97(4):1277–1284. https://doi.org/10.1210/jc.2011-2537
Jiajue R, Jiang Y, Wang O, Li M, Xing X, Cui L, Yin J, Xu L, Xia W (2014) Suppressed bone turnover was associated with increased osteoporotic fracture risks in non-obese postmenopausal Chinese women with type 2 diabetes mellitus. Osteoporos Int 25(8):1999–2005. https://doi.org/10.1007/s00198-014-2714-5
Busse B, Djonic D, Milovanovic P, Hahn M, Püschel K, Ritchie RO, Djuric M, Amling M (2010) Decrease in the osteocyte lacunar density accompanied by hypermineralized lacunar occlusion reveals failure and delay of remodeling in aged human bone. Aging Cell 9(6):1065–1075. https://doi.org/10.1111/j.1474-9726.2010.00633.x
Weinkamer R, Kollmannsberger P, Fratzl P (2019) Towards a connectomic description of the osteocyte lacunocanalicular network in bone. Curr Osteoporos Rep 17(4):186–194. https://doi.org/10.1007/s11914-019-00515-z
Paschalis EP, Gamsjaeger S, Klaushofer K (2017) Vibrational spectroscopic techniques to assess bone quality. Osteoporos Int 28(8):2275–2291. https://doi.org/10.1007/s00198-017-4019-y
Creecy A, Uppuganti S, Merkel AR, O'Neal D, Makowski AJ, Granke M, Voziyan P, Nyman JS (2016) Changes in the fracture resistance of bone with the progression of type 2 diabetes in the ZDSD rat. Calcif Tissue Int 99(3):289–301. https://doi.org/10.1007/s00223-016-0149-z
Mansur SA, Mieczkowska A, Flatt PR, Chappard D, Irwin N, Mabilleau G (2019) The GLP-1 receptor agonist exenatide ameliorates bone composition and tissue material properties in high fat fed diabetic mice. Front Endocrinol (Lausanne) 10:51. https://doi.org/10.3389/fendo.2019.00051
Pascart T, Falgayrac G, Migaud H, Quinchon J, Norberciak L, Budzik JF, Paccou J, Cotten A, Penel G, Cortet B (2017) Region specific Raman spectroscopy analysis of the femoral head reveals that trabecular bone is unlikely to contribute to non-traumatic osteonecrosis. Sci Rep 7(1):97. https://doi.org/10.1038/s41598-017-00162-3
Fiedler IAK, Schmidt FN, Wölfel EM, Plumeyer C, Milovanovic P, Gioia R, Tonelli F, Bale HA, Jähn K, Besio R, Forlino A, Busse B (2018) Severely impaired bone material quality in Chihuahua Zebrafish resembles classical dominant human Osteogenesis Imperfecta. J Bone Miner Res 33(8):1489–1499. https://doi.org/10.1002/jbmr.3445
Paschalis EP, Gamsjaeger S, Tatakis DN, Hassler N, Robins SP, Klaushofer K (2015) Fourier transform infrared spectroscopic characterization of mineralizing type I collagen enzymatic trivalent cross-links. Calcif Tissue Int 96(1):18–29. https://doi.org/10.1007/s00223-014-9933-9
Creecy A, Uppuganti S, Unal M, Clay Bunn R, Voziyan P, Nyman JS (2018) Low bone toughness in the TallyHO model of juvenile type 2 diabetes does not worsen with age. Bone. 110:204–214. https://doi.org/10.1016/j.bone.2018.02.005
Hammond MA, Gallant MA, Burr DB, Wallace JM (2014) Nanoscale changes in collagen are reflected in physical and mechanical properties of bone at the microscale in diabetic rats. Bone. 60:26–32. https://doi.org/10.1016/j.bone.2013.11.015
Mandair GS, Morris MD (2015) Contributions of Raman spectroscopy to the understanding of bone strength. Bonekey Rep 4:620. https://doi.org/10.1038/bonekey.2014.115
Kanazawa I, Sugimoto T (2018) Diabetes mellitus-induced bone fragility. Intern Med 57(19):2773–2785. https://doi.org/10.2169/internalmedicine.0905-18
Ogata N, Chikazu D, Kubota N, Terauchi Y, Tobe K, Azuma Y, Ohta T, Kadowaki T, Nakamura K, Kawaguchi H (2000) Insulin receptor substrate-1 in osteoblast is indispensable for maintaining bone turnover. J Clin Invest 105(7):935–943. https://doi.org/10.1172/JCI9017
Milovanovic P, Vom Scheidt A, Mletzko K, Sarau G, Püschel K, Djuric M, Amling M, Christiansen S, Busse B (2018) Bone tissue aging affects mineralization of cement lines. Bone. 110:187–193. https://doi.org/10.1016/j.bone.2018.02.004
Rolvien T, Vom Scheidt A, Stockhausen KE, Milovanovic P, Djonic D, Hubert J, Hawellek T, Wacker A, Jebens V, Püschel K, Zimmermann EA, Djuric M, Amling M, Busse B (2018) Inter-site variability of the osteocyte lacunar network in the cortical bone underpins fracture susceptibility of the superolateral femoral neck. Bone. 112:187–193. https://doi.org/10.1016/j.bone.2018.04.018
Acknowledgments
Authors thank medical technicians who assisted during sample collection: Branislav Milivojevic, Bojan Kacarevic, and Milos Knezevic (Institute for Pathology, University of Belgrade, Serbia).
Funding
This work was supported by institutional partnership grant of Alexander von Humboldt Foundation, South-East-Europe Cooperation of the University Medical Center Hamburg-Eppendorf under direction of Prof. H.J. Seitz, German Research Foundation (DFG, BU 2562/3-1), German Academic Exchange Service (DAAD), Ministry of Education and Science of the Republic of Serbia (III 45005), and Science Fund of the Republic of Serbia (PROMIS, #6064549, DiaBoNet). This project has received funding from the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie grant agreement no. 860898.
Author information
Authors and Affiliations
Contributions
Conceptualization: Marija Djuric; methodology: Marija Djuric, Björn Busse, and Petar Milovanovic; formal analysis and investigation: Teodora Rodic, Eva Maria Wölfel, Petar Milovanovic, Imke A.K. Fiedler, Katharina Jähn-Rickert, and Danica Cvetkovic; writing—original draft preparation: Teodora Rodic; writing—review and editing: Teodora Rodic, Petar Milovanovic, Marija Djuric, Eva Maria Wölfel, Imke A.K. Fiedler, Katharina Jähn-Rickert, Björn Busse; supervision: Marija Djuric, Björn Busse, Katharina Jähn, Michael Amling, Jelena Sopta, Slobodan Nikolic, and Vladimir Zivkovic; All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee of the Faculty of Medicine, University of Belgrade, Serbia, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the families of all individual participants included in the study. The aspect of confidentiality was respected.
Consent to publish
Not applicable.
Code availability
Available upon request.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Rodic, T., Wölfel, E.M., Milovanovic, P. et al. Bone quality analysis of jaw bones in individuals with type 2 diabetes mellitus—post mortem anatomical and microstructural evaluation. Clin Oral Invest 25, 4377–4400 (2021). https://doi.org/10.1007/s00784-020-03751-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03751-1