Abstract
Objectives
The aim of this study is to determine the use of platelet-rich fibrin (PRF) in the management of soft tissue donor site healing after harvesting connective tissue graft (CTG) from the palate and evaluate the postoperative discomfort (pain, bleeding, analgesic consumption, tissue color match) of patients.
Materials and methods
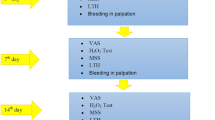
Forty patients were randomly assigned to PRF or control group. In the PRF group, PRF membrane was placed into CTG donor site. After surgery, delayed bleeding, early healing index (EHI), tissue color match, and analgesic consumption were recorded. The visual analog scale (VAS) was used to observe the postoperative pain and tissue color match. Data were analyzed using the independent sample t test and the repeated measure ANOVA test.
Results
The patients in the PRF group reported significantly lower pain scores at all-time points. Postoperative 3rd and 7th day, EHI scores were lower in the favor of the PRF group. VAS score values of tissue color match were lower in the control group at 7th and 14th day, compared with the PRF group. Analgesic intake was significantly lower in the PRF group postoperatively at 1st and 3rd day that of control group.
Conclusion
PRF application at the palatal donor site demonstrates promising results in terms of better wound healing and reduced postoperative discomfort in the patients after harvesting CTG.
Clinical relevance
Patients may avoid surgical operations because of the discomfort or pain feeling. Reducing postoperative pain and discomfort and accelerating recovery meet the wishes of every patient and physician. PRF can provide these requirements as an easy method to obtain and implement.








Similar content being viewed by others
References
Chambrone L, Sukekava F, Araujo MG, Pustiglioni FE, Chambrone LA, Lima LA (2010) Root-coverage procedures for the treatment of localized recession-type defects: a Cochrane systematic review. J Periodontol 81:452–478. https://doi.org/10.1902/jop.2010.090540
Zuhr O, Baumer D, Hurzeler M (2014) The addition of soft tissue replacement grafts in plastic periodontal and implant surgery: critical elements in design and execution. J Clin Periodontol 41(Suppl 15):S123–S142. https://doi.org/10.1111/jcpe.12185
Karthikeyan BV, Khanna D, Chowdhary KY, Prabhuji ML (2016) The versatile subepithelial connective tissue graft: a literature update. Gen Dent 64:e28–e33
Del Pizzo M, Modica F, Bethaz N, Priotto P, Romagnoli R (2002) The connective tissue graft: a comparative clinical evaluation of wound healing at the palatal donor site. a preliminary study. J Clin Periodontol 29:848–854
Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJ, Mouhyi J, Dohan DM (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV: clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:e56–e60. https://doi.org/10.1016/j.tripleo.2005.07.011
Miron RJ, Zucchelli G, Pikos MA, Salama M, Lee S, Guillemette V, Fujioka-Kobayashi M, Bishara M, Zhang Y, Wang HL, Chandad F, Nacopoulos C, Simonpieri A, Aalam AA, Felice P, Sammartino G, Ghanaati S, Hernandez MA, Choukroun J (2017) Use of platelet-rich fibrin in regenerative dentistry: a systematic review. Clin Oral Investig 21:1913–1927. https://doi.org/10.1007/s00784-017-2133-z
Canellas J, Medeiros PJD, Figueredo C, Fischer RG, Ritto FG (2018) Platelet-rich fibrin in oral surgical procedures: a systematic review and meta-analysis. Int J Oral Maxillofac Surg 48:395–414. https://doi.org/10.1016/j.ijom.2018.07.007
Choukroun J, Adda F, Schoeffler C, Vervelle A (2000) Une opportunité en paro-implantologie: le PRF. Implantodontie 42:55–62
Rudagi KB, Rudagi B (2012) One-step apexification in immature tooth using grey mineral trioxide aggregate as an apical barrier and autologus platelet rich fibrin membrane as an internal matrix. J Conserv Dent 15:196–199. https://doi.org/10.4103/0972-0707.94582
Inchingolo F, Tatullo M, Marrelli M, Inchingolo AM, Scacco S, Inchingolo AD, Dipalma G, Vermesan D, Abbinante A, Cagiano R (2010) Trial with platelet-rich fibrin and bio-oss used as grafting materials in the treatment of the severe maxillar bone atrophy: clinical and radiological evaluations. Eur Rev Med Pharmacol Sci 14:1075–1084
Mazor Z, Horowitz RA, Del Corso M, Prasad HS, Rohrer MD, Dohan Ehrenfest DM (2009) Sinus floor augmentation with simultaneous implant placement using Choukroun’s platelet-rich fibrin as the sole grafting material: a radiologic and histologic study at 6 months. J Periodontol 80:2056–2064. https://doi.org/10.1902/jop.2009.090252
Lekovic V, Milinkovic I, Aleksic Z, Jankovic S, Stankovic P, Kenney EB, Camargo PM (2012) Platelet-rich fibrin and bovine porous bone mineral vs. platelet-rich fibrin in the treatment of intrabony periodontal defects. J Periodontal Res 47:409–417. https://doi.org/10.1111/j.1600-0765.2011.01446.x
Bansal C, Bharti V (2013) Evaluation of efficacy of autologous platelet-rich fibrin with demineralized-freeze dried bone allograft in the treatment of periodontal intrabony defects. J Indian Soc Periodontol 17:361–366. https://doi.org/10.4103/0972-124X.115663
Del Corso M, Mazor Z, Rutkowski JL, Dohan Ehrenfest DM (2012) The use of leukocyte- and platelet-rich fibrin during immediate postextractive implantation and loading for the esthetic replacement of a fractured maxillary central incisor. J Oral Implantol 38:181–187. https://doi.org/10.1563/AAID-JOI-D-12-CL.3802
Aroca S, Keglevich T, Nikolidakis D, Gera I, Nagy K, Azzi R, Etienne D (2010) Treatment of class III multiple gingival recessions: a randomized-clinical trial. J Clin Periodontol 37:88–97. https://doi.org/10.1111/j.1600-051X.2009.01492.x
Jankovic S, Aleksic Z, Milinkovic I, Dimitrijevic B (2010) The coronally advanced flap in combination with platelet-rich fibrin (PRF) and enamel matrix derivative in the treatment of gingival recession: a comparative study. Eur J Esthet Dent 5:260–273
Femminella B, Iaconi MC, Di Tullio M, Romano L, Sinjari B, D'Arcangelo C, De Ninis P, Paolantonio M (2016) Clinical comparison of platelet-rich fibrin and a gelatin sponge in the management of palatal wounds after epithelialized free gingival graft harvest: a randomized clinical trial. J Periodontol 87:103–113. https://doi.org/10.1902/jop.2015.150198
Bahammam MA (2018) Effect of platelet-rich fibrin palatal bandage on pain scores and wound healing after free gingival graft: a randomized controlled clinical trial. Clin Oral Investig 22:3179–3188. https://doi.org/10.1007/s00784-018-2397-y
Eren G, Kantarci A, Sculean A, Atilla G (2016) Vascularization after treatment of gingival recession defects with platelet-rich fibrin or connective tissue graft. Clin Oral Investig 20:2045–2053. https://doi.org/10.1007/s00784-015-1697-8
He Y, Chen J, Huang Y, Pan Q, Nie M (2017) Local application of platelet-rich fibrin during lower third molar extraction improves treatment outcomes. J Oral Maxillofac Surg 75:2497–2506. https://doi.org/10.1016/j.joms.2017.05.034
Ustaoglu G, Ercan E, Tunali M (2016) The role of titanium-prepared platelet-rich fibrin in palatal mucosal wound healing and histoconduction. Acta Odontol Scand 74:558–564. https://doi.org/10.1080/00016357.2016.1219045
Fickl S, Fischer KR, Jockel-Schneider Y, Stappert CF, Schlagenhauf U, Kebschull M (2014) Early wound healing and patient morbidity after single-incision vs. trap-door graft harvesting from the palate--a clinical study. Clin Oral Investig 18:2213–2219. https://doi.org/10.1007/s00784-014-1204-7
Akpinar A, Toker H, Lektemur Alpan A, Calisir M (2016) Postoperative discomfort after Nd:YAG laser and conventional frenectomy: comparison of both genders. Aust Dent J 61:71–75. https://doi.org/10.1111/adj.12333
Dohan Ehrenfest DM, Del Corso M, Diss A, Mouhyi J, Charrier JB (2010) Three-dimensional architecture and cell composition of a Choukroun’s platelet-rich fibrin clot and membrane. J Periodontol 81:546–555. https://doi.org/10.1902/jop.2009.090531
Dohan Ehrenfest DM, Bielecki T, Jimbo R, Barbe G, Del Corso M, Inchingolo F, Sammartino G (2012) Do the fibrin architecture and leukocyte content influence the growth factor release of platelet concentrates? An evidence-based answer comparing a pure platelet-rich plasma (P-PRP) gel and a leukocyte- and platelet-rich fibrin (L-PRF). Curr Pharm Biotechnol 13:1145–1152
Thibault MM, Hoemann CD, Buschmann MD (2007) Fibronectin, vitronectin, and collagen I induce chemotaxis and haptotaxis of human and rabbit mesenchymal stem cells in a standardized transmembrane assay. Stem Cells Dev 16:489–502. https://doi.org/10.1089/scd.2006.0100
Jain V, Triveni MG, Kumar AB, Mehta DS (2012) Role of platelet-rich-fibrin in enhancing palatal wound healing after free graft. Contemp Clin Dent 3:S240–S243. https://doi.org/10.4103/0976-237X.101105
Yen CA, Griffin TJ, Cheung WS, Chen J (2007) Effects of platelet concentrate on palatal wound healing after connective tissue graft harvesting. J Periodontol 78:601–610. https://doi.org/10.1902/jop.2007.060275
Nawshad A, LaGamba D, Hay ED (2004) Transforming growth factor beta (TGFbeta) signalling in palatal growth, apoptosis and epithelial mesenchymal transformation (EMT). Arch Oral Biol 49:675–689. https://doi.org/10.1016/j.archoralbio.2004.05.007
Dohan Ehrenfest DM, Pinto NR, Pereda A, Jimenez P, Corso MD, Kang BS, Nally M, Lanata N, Wang HL, Quirynen M (2018) The impact of the centrifuge characteristics and centrifugation protocols on the cells, growth factors, and fibrin architecture of a leukocyte- and platelet-rich fibrin (L-PRF) clot and membrane. Platelets 29:171–184. https://doi.org/10.1080/09537104.2017.1293812
Sharma A, Aggarwal N, Rastogi S, Choudhury R, Tripathi S (2017) Effectiveness of platelet-rich fibrin in the management of pain and delayed wound healing associated with established alveolar osteitis (dry socket). Eur J Dent 11:508–513. https://doi.org/10.4103/ejd.ejd_346_16
Mosesson MW, Siebenlist KR, Meh DA (2001) The structure and biological features of fibrinogen and fibrin. Ann N Y Acad Sci 936:11–30
Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:e37–e44. https://doi.org/10.1016/j.tripleo.2005.07.008
Daugela P, Grimuta V, Sakavicius D, Jonaitis J, Juodzbalys G (2018) Influence of leukocyte- and platelet-rich fibrin (L-PRF) on the outcomes of impacted mandibular third molar removal surgery: a split-mouth randomized clinical trial. Quintessence Int 49:377–388. https://doi.org/10.3290/j.qi.a40113
Al-Hamed FS, Tawfik MA, Abdelfadil E, Al-Saleh MAQ (2017) Efficacy of platelet-rich fibrin after mandibular third molar extraction: a systematic review and meta-analysis. J Oral Maxillofac Surg 75:1124–1135. https://doi.org/10.1016/j.joms.2017.01.022
Ozcan M, Ucak O, Alkaya B, Keceli S, Seydaoglu G, Haytac MC (2017) Effects of platelet-rich fibrin on palatal wound healing after free gingival graft harvesting: a comparative randomized controlled clinical trial. Int J Periodontics Restorative Dent 37:e270–e278. https://doi.org/10.11607/prd.3226
Ozgul O, Senses F, Er N, Tekin U, Tuz HH, Alkan A, Kocyigit ID, Atil F (2015) Efficacy of platelet rich fibrin in the reduction of the pain and swelling after impacted third molar surgery: randomized multicenter split-mouth clinical trial. Head Face Med 11:37. https://doi.org/10.1186/s13005-015-0094-5
Dohan Ehrenfest DM, Andia I, Zumstein MA, Zhang CQ, Pinto NR, Bielecki T (2014) Classification of platelet concentrates (platelet-rich plasma-PRP, platelet-rich fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J 4:3–9
Shimokado K, Raines EW, Madtes DK, Barrett TB, Benditt EP, Ross R (1985) A significant part of macrophage-derived growth factor consists of at least two forms of PDGF. Cell 43:277–286
Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:e45–e50. https://doi.org/10.1016/j.tripleo.2005.07.009
Acknowledgments
We would like to thank to Prof. Dr. Hülya TOKER (Health Sciences University Gülhane Faculty of Dentistry Department of Periodontology) and PhD DDS Mustafa TUNALI (Bezmialem University Faculty of Dentistry Department of Periodontology) for contributions to the manuscript.
Funding
This study is a self-funded study, not supported by an institution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Pamukkale University Ethical Committee with 60116787-020/44407 protocol number and number 13.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lektemur Alpan, A., Torumtay Cin, G. PRF improves wound healing and postoperative discomfort after harvesting subepithelial connective tissue graft from palate: a randomized controlled trial. Clin Oral Invest 24, 425–436 (2020). https://doi.org/10.1007/s00784-019-02934-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02934-9