Abstract
Objectives
Osteoporosis is a disease characterized by a reduction in bone mass, poor bone strength, and microarchitectural deterioration primarily in postmenopausal women. With respect to periodontal disease, osteoporosis is thought to contribute to pre-existing alveolar degeneration although the association between both diseases is not fully characterized. The aim of the present study was to observe the initial changes in mandibular alveolar bone for sham-operated and ovariectomized (OVX) rats in ligature-induced experimental periodontitis.
Materials and methods
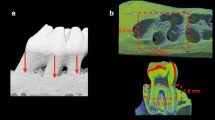
A total of 64 Wistar rats (7 weeks of age, 180–200 g) were used in this study (32 control sham-operated animals + ligature placement, 32 OVX animals + ligature placement). Following an 8-week period to induce an OVX model, micro-CT analysis was performed to calculate vertical and furcation bone loss of mandibular first molars at time points 0, 3, 7, and 11 days following ligature placement (six animals per group per time point). Furthermore, histological analysis was performed to calculate the loss of alveolar bone crest height from the cemento-enamel junction, and tartrate-resistant acid phosphatase (TRAP) staining was utilized to calculate the number of osteoclasts.
Results
The results from the present study demonstrate that OVX animals showed significant vertical bone loss at all time points when compared to control sham-operated animals. In the furcation area, no significant difference in bone loss was observed between sham-operated and OVX animals at 0, 3, and 7 days; however by 11 days, a significant decrease in bone volume/total volume and trabecular thickness was observed in the OVX group. The histological analysis also revealed that alveolar bone crest height was significantly reduced in OVX animals, and TRAP staining further revealed the greater number of multinucleated osteoclasts peaking at 3 days postligature placement.
Conclusion
The results from the present study demonstrate a direct correlation between the osteoporotic phenotype and the progression of periodontal breakdown in a diseased-induced animal model.
Clinical relevance
It may be suggested that an osteoporotic phenotype has the potential to speed periodontal breakdown and thus contributes to the overall degeneration of the periodontium in patients suffering from postmenopausal bone loss. Future research from human clinical studies are necessary to further understand the relationship between periodontal disease and osteoporosis.






Similar content being viewed by others
References
Tontonoz P, Pei LM (2004) Fat's loss is bone's gain. J Clin Invest 113:805–806. doi:10.1172/Jci200421311
Rodan GA, Martin TJ (2000) Therapeutic approaches to bone diseases. Science 289:1508–1514
Antonenko O, Bryk G, Brito G, Pellegrini G, Zeni SN (2014) Oral health in young women having a low calcium and vitamin D nutritional status. Clin Oral Investig. doi:10.1007/s00784-014-1343-x
Hansen PJ, Knitschke M, Draenert FG, Irle S, Neff A (2013) Incidence of bisphosphonate-related osteonecrosis of the jaws (BRONJ) in patients taking bisphosphonates for osteoporosis treatment—a grossly underestimated risk? Clin Oral Investig 17:1829–1837. doi:10.1007/s00784-012-0873-3
Marchand-Libouban H, Guillaume B, Bellaiche N, Chappard D (2013) Texture analysis of computed tomographic images in osteoporotic patients with sinus lift bone graft reconstruction. Clin Oral Investig 17:1267–1272. doi:10.1007/s00784-012-0808-z
Teitelbaum SL (2010) Stem cells and osteoporosis therapy. Cell Stem Cell 7:553–554. doi:10.1016/j.stem.2010.10.004
Silva BC, Bilezikian JP (2011) New approaches to the treatment of osteoporosis. Annu Rev Med 62:307–322. doi:10.1146/annurev-med-061709-145401
Passos Jde S, Gomes-Filho IS, Vianna MI, da Cruz SS, Barreto ML, Oliveira TJ, Borges LD, Monteiro FM (2010) Outcome measurements in studies on the association between osteoporosis and periodontal disease. J Periodontol 81:1773–1780. doi:10.1902/jop.2010.100143
Sultan N, Rao J (2011) Association between periodontal disease and bone mineral density in postmenopausal women: a cross sectional study. Med Oral Patol Oral Cir Bucal 16:e440–e447
von Wowern N, Klausen B, Kollerup G (1994) Osteoporosis: a risk factor in periodontal disease. J Periodontol 65:1134–1138
Brennan RM, Genco RJ, Hovey KM, Trevisan M, Wactawski-Wende J (2007) Clinical attachment loss, systemic bone density, and subgingival calculus in postmenopausal women. J Periodontol 78:2104–2111. doi:10.1902/jop.2007.070155
Al Habashneh R, Alchalabi H, Khader YS, Hazza'a AM, Odat Z, Johnson GK (2010) Association between periodontal disease and osteoporosis in postmenopausal women in jordan. J Periodontol 81:1613–1621. doi:10.1902/jop.2010.100190
Takahashi O, Yoshihara A, Nakamura K, Miyazaki H (2012) Association between periodontitis and systemic bone mineral density in Japanese community-dwelling postmenopausal women. J Dent 40:304–311. doi:10.1016/j.jdent.2012.01.005
Passos JS, Vianna MI, Gomes-Filho IS, Cruz SS, Barreto ML, Adan L, Rosing CK, Cerqueira EM, Trindade SC, Coelho JM (2013) Osteoporosis/osteopenia as an independent factor associated with periodontitis in postmenopausal women: a case-control study. Osteoporos Int J Established Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 24:1275–1283. doi:10.1007/s00198-012-2130-7
Marjanovic EJ, Southern HN, Coates P, Adams JE, Walsh T, Horner K, Devlin H (2013) Do patients with osteoporosis have an increased prevalence of periodontal disease? A cross-sectional study. Osteoporos Int J Established Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 24:1973–1979. doi:10.1007/s00198-012-2246-9
Darcey J, Devlin H, Lai D, Walsh T, Southern H, Marjanovic E, Horner K (2013) An observational study to assess the association between osteoporosis and periodontal disease. Br Dent J 215:617–621. doi:10.1038/sj.bdj.2013.1191
Miron RJ, Wei L, Bosshardt DD, Buser D, Sculean A, Zhang Y (2014) Effects of enamel matrix proteins in combination with a bovine-derived natural bone mineral for the repair of bone defects. Clin Oral Investig 18:471–478. doi:10.1007/s00784-013-0992-5
Miron RJ, Wei L, Yang S, Caluseru OM, Sculean A, Zhang Y (2014) Effect of an enamel matrix derivative on periodontal wound healing/regeneration in an osteoporotic model. J Periodontol 11:1603–1611. doi:10.1902/jop.2014.130745
Wei L, Ke J, Prasadam I, Miron RJ, Lin S, Xiao Y, Chang J, Wu C, Zhang Y (2014) A comparative study of Sr-incorporated mesoporous bioactive glass scaffolds for regeneration of osteopenic bone defects. Osteoporos Int J Established Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 25:2089–2096. doi:10.1007/s00198-014-2735-0
Zhang Y, Cheng N, Miron R, Shi B, Cheng X (2012) Delivery of PDGF-B and BMP-7 by mesoporous bioglass/silk fibrin scaffolds for the repair of osteoporotic defects. Biomaterials 33:6698–6708. doi:10.1016/j.biomaterials.2012.06.021
Yang S, Lan L, Miron RJ, Wei L, Zhang M, Zhang Y (2014) Variability in particle degradation of four commonly employed dental bone grafts. Clin Implant Dent Relat Res. doi:10.1111/cid.12196
Zhang Y, Wei L, Miron RJ, Shi B, Bian Z (2015) Anabolic bone formation via a site-specific bone-targeting delivery system by interfering with semaphorin 4D expression. J Bone Mineral Res Off J Am Soc Bone Mineral Res 30:286–296. doi:10.1002/jbmr.2322
Gyorfi A, Fazekas A, Suba Z, Ender F, Rosivall L (1994) Neurogenic component in ligature-induced periodontitis in the rat. J Clin Periodontol 21:601–605
Nociti FH Jr, Nogueira-Filho GR, Primo MT, Machado MA, Tramontina VA, Barros SP, Sallum EA (2000) The influence of nicotine on the bone loss rate in ligature-induced periodontitis. A histometric study in rats. J Periodontol 71:1460–1464. doi:10.1902/jop.2000.71.9.1460
Samejima Y, Ebisu S, Okada H (1990) Effect of infection with Eikenella corrodens on the progression of ligature-induced periodontitis in rats. J Periodontal Res 25:308–315
Jarry CR, Duarte PM, Freitas FF, de Macedo CG, Clemente-Napimoga JT, Saba-Chujfi E, Passador-Santos F, de Araujo VC, Napimoga MH (2013) Secreted osteoclastogenic factor of activated T cells (SOFAT), a novel osteoclast activator, in chronic periodontitis. Hum Immunol 74:861–866. doi:10.1016/j.humimm.2013.04.013
Niwa T, Mizukoshi K, Azuma Y, Kashimata M, Shibutani T (2013) Fundamental study of osteoclast chemotaxis toward chemoattractants expressed in periodontitis. J Periodontal Res 48:773–780. doi:10.1111/jre.12068
Vernal R, Diaz-Zuniga J, Melgar-Rodriguez S, Pujol M, Diaz-Guerra E, Silva A, Sanz M, Garcia-Sanz JA (2014) Activation of RANKL-induced osteoclasts and memory T lymphocytes by Porphyromonas gingivalis is serotype dependant. J Clin Periodontol 41:451–459. doi:10.1111/jcpe.12236
Casarin RC, Ribeiro Edel P, Nociti FH Jr, Sallum AW, Ambrosano GM, Sallum EA, Casati MZ (2010) Enamel matrix derivative proteins for the treatment of proximal class II furcation involvements: a prospective 24-month randomized clinical trial. J Clin Periodontol 37:1100–1109. doi:10.1111/j.1600-051X.2010.01614.x
Casarin RC, Ribeiro Edel P, Ribeiro FV, Nociti FH Jr, Sallum AW, Sallum EA, Casati MZ (2009) Influence of anatomic features on the effectiveness of enamel matrix derivative proteins in the treatment of proximal Class II furcation involvements. Quintessence Int 40:753–761
Gkranias ND, Graziani F, Sculean A, Donos N (2012) Wound healing following regenerative procedures in furcation degree III defects: histomorphometric outcomes. Clin Oral Investig 16:239–249. doi:10.1007/s00784-010-0478-7
Conflict of interest
Dai Jing, Yihui Ma, Miusi Shi, Zhengguo Cao, Richard J. Miron, and Yufeng Zhang declare that they have no conflict of interest. This project was supported by Program for New Century Excellent Talents in University (NCET-11-0414), Excellent Youth Foundation of Hubei, and the funds of the National Natural Science Foundation of China (81271108).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dai, J., Ma, Y., Shi, M. et al. Initial changes in alveolar bone volume for sham-operated and ovariectomized rats in ligature-induced experimental periodontitis. Clin Oral Invest 20, 581–588 (2016). https://doi.org/10.1007/s00784-015-1531-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1531-3