Abstract
Objectives
To evaluate the medium-term clinical performance of direct composite build-ups for diastema closures and teeth recontouring using a nano and a nanohybrid composite in combination with three- or two-step etch-and-rinse adhesives following treatment with fixed orthodontic appliances.
Materials and methods
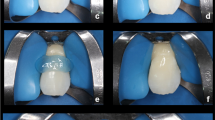
A total of 30 patients (mean age, 19.5 years) received 147 direct composite additions for teeth recontouring and diastema closures. A nano and a nanohybrid composite (Filtek Supreme XT and CeramX Duo) were bonded to tooth structure by using a three-step (Scotchbond Multipurpose) or a two-step (XP Bond) etch and rinse adhesive. Ten out of 147 composite build-ups (composite addition) constituted tooth recontouring cases, and the remaining 137 constituted diastema closure cases. The restorations were evaluated by two experienced, calibrated examiners according to modified Ryge criteria at the following time intervals: baseline, 1, 2, 3, and 4 years.
Results
The 4-year survival rates were 92.8 % for Filtek Supreme XT/Scotchbond Multi-Purpose Plus and 93 % for CeramX Duo/XP Bond. Only ten restorations failed (5 Filtek Supreme XT and 5 CeramX Duo). Statistical analysis revealed no significant differences between the two composite–adhesive combinations with respect to color match, marginal discoloration, wear/loss of anatomical form, caries formation, marginal adaptation, and surface texture on comparing the five time periods (baseline, 1, 2, 3, and 4 years)
Conclusions
The 4-year survival rates in the present study were favorable. The restorations exhibited excellent scores with regard to color match, marginal adaptation, surface texture, marginal discoloration, wear/loss of anatomical form, and caries formation, after 4 years of clinical evaluation.
Clinical relevance
An alternative clinical approach for correcting discrepancies in tooth size and form, such as performing direct composite restorations following fixed orthodontic treatment, may be an excellent and minimally invasive treatment.







Similar content being viewed by others
References
Wolff D, Kraus T, Schach C, Pritsch M, Mente J, Staehle HJ, Ding P (2010) Recontouring teeth and closing diastemas with direct composite buildups: a clinical evaluation of survival and quality parameters. J Dent 38:1001–1009
Staehle HJ (1999) Minimally invasive restorative treatment. J Adhes Dent 1:267–284
Frese C, Schiller P, Staehle HJ, Wolff D (2013) Recontouring teeth and closing diastemas with direct composite buildups: a 5-year follow-up. J Dent 41:979–985
Buonocore MG (1955) A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res 34:849–853
Peumans M, Van Meerbeek B, Lambrechts P, Vanherle G (1997) The 5-year clinical performance of direct composite additions to correct tooth form and position. II. Marginal qualities. Clin Oral Investig 1:19–26
Peumans M, Van Meerbeek B, Lambrechts P, Vanherle G (1997) The 5-year clinical performance of direct composite additions to correct tooth form and position. I. Esthetic qualities. Clin Oral Investig 1:12–18
Heymann HO, Hershey HG (1985) Use of composite resin for restorative and orthodontic correction of anterior interdental spacing. J Prosthet Dent 53:766–771
Peumans M, Van Meerbeek B, Lambrechts P, Vanherle G, Quirynen M (1998) The influence of direct composite additions for the correction of tooth form and/or position on periodontal health. A retrospective study. J Periodontol 69:422–427
Peumans M, Kanumilli P, De Munck J, Van Landuyt K, Lambrechts P, Van Meerbeek B (2005) Clinical effectiveness of contemporary adhesives: a systematic review of current clinical trials. Dent Mater 21:864–881
Van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P, Van Landuyt K, Lambrechts P, Vanherle G (2003) Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper Dent 28:215–235
de Andrade AK, Duarte RM, Medeiros e Silva FD, Batista AU, Lima KC, Pontual ML, Montes MA (2011) 30-Month randomised clinical trial to evaluate the clinical performance of a nanofill and a nanohybrid composite. J Dent 39:8–15
van Dijken JW, Pallesen U (2011) Four-year clinical evaluation of class II nano-hybrid resin composite restorations bonded with a one-step self-etch and a two-step etch-and-rinse adhesive. J Dent 39:16–25
Schirrmeister JF, Huber K, Hellwig E, Hahn P (2006) Two-year evaluation of a new nano-ceramic restorative material. Clin Oral Investig 10:181–186
Filtek™ Supreme XT Universal Restorative (2005) Technical product profile, USA
Gresnigt MM, Kalk W, Ozcan M (2012) Randomized controlled split-mouth clinical trial of direct laminate veneers with two micro-hybrid resin composites. J Dent 40:766–775
Heymann HO (2002) Additional conservative esthetic procedures. In: Sturdevant CM (ed) The art and science of operative dentistry, 4th edn. C.V. Mosby Co., St. Louis, pp 591–650
Ryge G (1980) Clinical criteria. Int Dent J 30:347–358
Barnes DM, Blank LW, Gingell JC, Gilner PP (1995) A clinical evaluation of a resin-modified glass ionomer restorative material. J Am Dent Assoc 126:1245–1253
Demirci M, Uysal O (2006) Clinical evaluation of a polyacid-modified resin composite (Dyract AP) in class I cavities: 3-year results. Am J Dent 19:376–381
Cvar JF, Ryge G (2005) Reprint of criteria for the clinical evaluation of dental restorative materials. Clin Oral Investig 9:215–232
Roulet JF (1997) Longevity of glass ceramic inlays and amalgam—results up to 6 years. Clin Oral Investig 1:40–46
Fields HW Jr (1981) Orthodontic restorative treatment for relative mandibular anterior excess tooth-size problems. Am J Orthod 79:176–183
Müssig E, Lux CJ, Staehle HJ, Stellzig-Eisenhauer A, Komposch G (2004) Applications for direct composite restorations in orthodontics. J Orofac Orthop 65:164–179
Wise RJ, Nevins M (1988) Anterior tooth site analysis (Bolton Index): how to determine anterior diastema closure. Int J Periodontics Restorative Dent 8:8–23
Sakaguchi RL, Powers JM (2012) Craig’s restorative dental materials, 13th edn. Elsevier Mosby, Philadelphia
Mitra SB, Wu D, Holmes BN (2003) An application of nanotechnology in advanced dental materials. J Am Dent Assoc 134:1382–1390
Chen MH (2010) Update on dental nanocomposites. J Dent Res 89:549–560
Cetin AR, Unlu N (2009) One-year clinical evaluation of direct nanofilled and indirect composite restorations in posterior teeth. Dent Mater J 28:620–626
Stefanski S, van Dijken JW (2012) Clinical performance of a nanofilled resin composite with and without an intermediary layer of flowable composite: a 2-year evaluation. Clin Oral Investig 16:147–53
Østervemb N, Jørgensen JN, Hørsted-Bindslev P (2011) A new approach to compare the esthetic properties of different composite materials. J Esthet Restor Dent 23:238–246
Beier US, Kapferer I, Burtscher D, Dumfahrt H (2012) Clinical performance of porcelain laminate veneers for up to 20 years. Int J Prosthodont 25:79–85
Peumans M, De Munck J, Fieuws S, Lambrechts P, Vanherle G, Van Meerbeek B (2004) A prospective ten-year clinical trial of porcelain veneers. J Adhes Dent 6:65–76
D’Arcangelo C, De Angelis F, Vadini M, D’Amario M (2012) Clinical evaluation on porcelain laminate veneers bonded with light-cured composite: results up to 7 years. Clin Oral Investig 16:1071–1079
Layton D, Walton T (2007) An up to 16-year prospective study of 304 porcelain veneers. The Int J Prosthodont 20:389–396
Fradeani M, Redemagni M, Corrado M (2005) Porcelain laminate veneers: 6- to 12-year clinical evaluation—a retrospective study. Int J Periodontics Restorative Dent 25:9–17
De Munck J, Van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Braem M, Van Meerbeek B (2005) A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res 84:118–132
Loguercio AD, Moura SK, Pellizzaro A, Dal-Bianco K, Patzlaff RT, Grande RH, Reis A (2008) Durability of enamel bonding using two-step self-etch systems on ground and unground enamel. Oper Dent 33:79–88
Hickel R, Roulet JF, Bayne S, Heintze SD, Mjör IA, Peters M, Rousson V, Randall R, Schmalz G, Tyas M, Vanherle G (2007) Recommendations for conducting controlled clinical studies of dental restorative materials. Clin Oral Investig 11:5–33
Beun S, Glorieux T, Devaux J, Vreven J, Leloup G (2007) Characterization of nanofilled compared to universal and microfilled composites. Dent Mater 23:51–59
Condon JR, Ferracane JL (2002) Reduced polymerization stress through non-bonded nanofiller particles. Biomaterials 23:3807–3815
Yap AUJ, Yap SH, Teo CK, Ng JJ (2004) Comparison of surface finish of new aesthetic restorative materials. Oper Dent 29:100–104
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Demirci, M., Tuncer, S., Öztaş, E. et al. A 4-year clinical evaluation of direct composite build-ups for space closure after orthodontic treatment. Clin Oral Invest 19, 2187–2199 (2015). https://doi.org/10.1007/s00784-015-1458-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1458-8