Abstract
Trial design
This is a randomized, controlled, superiority, double-blinded, parallel-group, two-arms trial with an allocation ratio of 1:1. The aim of this trial was to compare the two-year clinical performance of partial indirect restorations fabricated from CAD/CAM nano-hybrid composite and ceramic lithium disilicate blocks using the modified USPHS criteria.
Methods
In two parallel groups (n = 50 restorations), fifty participants having mutilated vital teeth with a minimum of two remaining walls were randomly enrolled in this trial and received indirect restorations of either nano-hybrid composite resin blocks (Brilliant, Coltene, Switzerland) or Lithium Disilicate (IPS Emax CAD). The restorations were assessed using modified USPHS criteria by two independent blinded assessors at baseline, six months, one-year and two years follow-up visits. Categorical and ordinal data were presented as frequencies and percentages. Categorical data were analyzed using the chi-square test. Ordinal data were analyzed using the Mann-Whitney U test for intergroup comparisons and Freidman’s test followed by the Nemenyi post hoc test for intragroup comparisons. Numerical data were presented as mean and standard deviation values. They were analyzed for normality using the Shapiro-Wilk test. Data were found to be normally distributed and were analyzed using the independent t-test. The significance level was set at p ≤ 0.05 within all tests.
Results
Forty-eight participants received the allocated intervention and completed the follow-up periods. There was a statistically significant difference between both tested materials for all USPHS criteria regarding Marginal integrity and Marginal discoloration at six-months Follow-up, but with no statistically significant difference at one- and two-year follow-up.
Conclusions
Both materials showed an acceptable, successful clinical performance along the two-years follow-up period.
Clinical relevance
The CAD/CAM nano-hybrid composite blocks are as reliable as Lithium disilicate for restoring mutilated vital teeth.
Similar content being viewed by others
Introduction
The choice of the most appropriate technique and material to restore large cavities with weakened cusps still creates doubts among clinicians [1]. To obtain an ideal anatomy, contour and contact, indirect partial coverage restorations are favored [2]. Although they offer adequate resistance to fracture and wear [3], clinical fracture is not uncommon [4].
Recently, there has been an increasing interest in fabricating such restorations using the CAD/CAM technology. This offers the opportunity to scan, design, and fabricate the restoration in a single appointment without making impressions, provisional restorations, or dental laboratory support. Moreover, industrially fabricated blocks are more homogeneous, and have higher intrinsic strength than the materials used for direct restorations [4].
Different ceramic systems are available for constructing restorations using CAD/CAM technology. This includes blocks made with glass ceramics, resin nano ceramics, zirconia, ceramic composites, ceramics and resin composites [5]. IPS e.max CAD (Ivoclar-Vivadent, Liechtenstein, Germany) is a milling lithium disilicate-reinforced ceramic with a high crystalline content of up to 70 vol% in a glass matrix. It comes as a pre-crystallized block, containing 32 vol% of metasilicate (Li2SiO3) crystals and 0.7 vol% lithium disilicate (Li2Si2O5) crystal nuclei, displaying a flexural strength of around 130 MPa, making the milling process easier. It is later crystallized in a ceramic oven at 850 °C in a vacuum for 20–25 min, where the metasilicate is dissolved and crystallizes as lithium disilicate changing from a bluish color to the chosen shade and translucency and increasing its flexural strength to around 360 MPa [6, 7].
CAD/CAM composites have superior mechanical properties to direct resin composites [8,9,10] due to the innovative composition and polymerisation modes under high temperature and pressure [11]. This category of materials merges the favourable properties of ceramics such as durability, enamel-like surface finish, good esthetics, and colour stability, with the favourable properties of composite resin, such as high flexural strength, low abrasiveness, and ease of polishing [12, 13]. Another possible advantage of resilient ceramic materials is that the adhesive resin cements may have a more similar wear rate than the restoration, leading to improved marginal integrity over time [14]. Brilliant Crios (Coltène Whaledent, Switzerland) is a nano-hybrid composite that contains barium glass (< 1.0 μm), amorphous silica (< 20 nm) with a filler wt of 70.7% in addition o resin matrix cross-linked methacrylates and inorganic pigments such as ferrous oxide or titanium dioxide.
Currently, scarce clinical data exists on the long-term outcomes of posterior partial indirect restorations fabricated from either CAD ceramic or composite blocks [15, 16]. Therefore, this study sought to evaluate the clinical performance of restorations fabricated from either IPS e.max CAD or Brilliant Crios nano-hybrid composite blocks regarding marginal integrity, marginal discoloration and restoration fracture using the modified USPHS criteria. The null hypothesis tested is that both materials will present a similar clinical performance after two years of clinical use.
Materials and methods
All materials and their description, composition, lot number and manufacturer are listed in Table 1.
Study setting
Approval of the study design was provided by the Research Ethics Committee at Cairo University, Egypt (CREC) (approval number: 16-09-2020, Date: 24-09-2020). Participants were recruited from the the Conservative Dentistry Department outpatient clinic, Faculty of Dentistry, Cairo University. All the patients were informed about the treatment’s indications, benefits, risks, and possible complications. All participants signed a written informed consent form. All procedures performed in this study were by with the Helsinki Declaration. The study protocol was registered in (www.clinicaltrials.gov) database, with unique identification number NCT04563624 on the date (24/09/2020).
Trial design
The study design for this randomized controlled clinical trial was a double-blinded, parallel-group, two-arms, superiority trial with an allocation ratio of 1:1.
Sample size calculation
A power analysis was designed to have adequate power to apply a statistical test of the null hypothesis that CAD/CAM indirect restorations fabricated from ceramic blocks are superior to those fabricated from composite blocks regarding their marginal adaptation after 24 months. According to the results of Fasbinder et al. [17] in which, the probability of score alpha-1 for marginal adaptation of CAD/CAM indirect ceramic restorations was (0.757), the probability of alpha-2 score was (0.243) with effect size w = 0.514 (n = 30). If the probability of score alpha-1 for marginal adaptation of indirect CAD/CAM composite restorations was (0.914), the probability of alpha-2 score was (0.086) with effect size w = 0.828 (n = 12), by adopting an alpha (α) level of 0.05 (5%), power = 80%. The predicted sample size was 42 (21 per group). The sample size was increased by (20%) to account for possible dropouts during follow-up intervals to be a total of [50] cases, i.e. [25]. for each group. Sample size calculation was performed using G*Power 3.1.9.2 using chi-square test with a superiority framework.
Eligibility criteria
Inclusion criteria
Patients included in the study were healthy males and females (Category: American Society of Anesthesiologists class 1, aged 16–45 years, presenting with good oral hygiene, healthy periodontium, a single badly broken down vital molar (caries reaching > 1/2 of the dentin thickness on periapical digital radiographic examination, with at least two missing cavity walls and the cavo-surface margins in enamel), and the antagonist teeth present in normal occlusion.
Exclusion criteria
Patients presenting one of the following situations were not included in the study: the presence of systemic disease (ASA 2–6), pregnancy or breastfeeding, hypersensitive, endodontically treated, non-vital or cracked teeth, multiple teeth that required treatment, patients with wear facets and parafunctional habits as clinching and bruxism, allergy to the composite resin and adhesive system, high caries risk index, or active periodontal disease.
Randomization and blinding
Using computer-generated randomization (www.randomization.com), the participants who fulfilled the eligibility criteria were allocated randomly into two groups with a 1:1 allocation ratio (25 participants in each group). The sequentially generated numbers were placed by MH in opaque envelopes until the time of intervention. Participants were enrolled by OH. Each participant was asked to select an envelope that determined his/her group for future intervention. HA assigned participants to interventions. The participants and the statistician were blinded, while the operator could not be blinded due to the nature of the intervention used.
Intervention
Demographic data were recorded, and each patient’s medical and dental status and history were collected in charts. Clinical and radiographic examinations were performed, and their findings were registered.
Restorative procedures
All operative procedures were performed with rubber dam isolation. All cavities were prepared according to the accepted principles for adhesive onlays [18]. A diamond stone # 245 (Komet, USA) and a straight fissure carbide bur number 57 size 010 (Komet, USA) were used to prepare the cavities. A new bur was used for every six preparations [19]. All carious dentin was excavated and removed by a hand excavator (#51/52, Maillefer Dentsply, Switzerland) according to the recent caries removal clinical recommendations [20]. Cuspal tipping for not less than 2 mm clearance, measured by a caliper (Diamonds Surgical Instruments, Pakistan), was done by a wheel stone (#909, Komet, USA) for weak cusps. Finishing was done using an extra-fine grit yellow-coded tapered with round-end diamond stones (#368EF, Komet, USA). The cavity walls were prepared with 12–15 degrees internal axial wall divergence using blue-coded diamond tapered with round end bur diameter 16, length 10 (MIDWEST Dentsply) held parallel to the long axis of the tooth.
During preparation, the following parameters checklist was followed for standardization [21]:
-
1.
The thickness of the remaining walls, in order to maintain them, had to be ≥ 2 mm measured by a dental caliper.
-
2.
The pulpal floor was prepared to provide a depth range of 3–4 mm measured by a periodontal probe.
-
3.
The width of the occlusal isthmus had to be at least 2–3 mm.
-
4.
Buccal and lingual walls of the proximal part of the cavity were prepared using the same diamond bur (Komet, USA) used for the occlusal part of the cavity to provide the same angle of divergence (12–15 degrees) as that of the occlusal walls.
-
5.
The internal line angles were rounded, and the cavo-surface angles were 90°.
-
6.
Regarding the cuspal coverage cases, the available inter-occlusal clearance was checked to be at least 2 mm in maximum intercuspation and during lateral movements.
Cavity design optimization (CDO)
The cavity was optimized, if needed, using the flowable resin (Brilliant EverGlow™ Flow, coltene), which was placed to block existing internal cavity undercuts; followed by light-curing for 20 s using a LED light-curing device (Elipar™ Deep Cure, 3 M ESPE) of 1470 mw/cm2 light intensity. Post-curing through clear glycerin gel was done for an additional 20 s to minimize the formation of an oxygen inhibition layer. Before intra-oral scanning, proper cavity evaluation was done regarding the sharp margins, absence of undercuts or any sharp irregularities [22].
Restoration construction
Each prepared tooth was scanned using the Omnicam intraoral camera of the CEREC system software version 4.60 (Sirona Dental Systems GmbH, D- 64,625 Benshein, Germany) for taking the optical impression [23]. Using the CEREC software version 4.60, the margin was drawn, and the final design was obtained and checked. The setting for the machining of composite restorations for occlusal and the lateral wall-thickness was entered to be 1.5 mm and with a 100 μm for the cement space. The MCXL milling machine (Sirona, USA) was used to mill the indirect restorations from nanohybrid CAD/CAM composite blocks (Brilliant blocs) size 14.
Cementation procedures
Before the cementation procedure, proper cleaning of the sealed cavity was achieved with soft-air abrasion airborne particle abrasion with aluminium oxide after try-in of the restoration and before cementation [24]. The restoration fitting surface was cleaned and roughened with 50 microns aluminium oxide using an intraoral sandblaster unit (Aquacare, Velopex, UK) [25]. The restoration was then placed in an ultrasonic cleaner filled with distilled water for 4 min [26]. After removal from the cleaner, the fitting surface was gently air-dried. The adhesive was actively rubbed for 20 s (One coat7), and solvent evaporation was allowed for 20 s before light-curing for 10 s, according to the manufacturer’s instruction [27]. The tooth surface was activated for bonding by air abrasion with 29 microns aluminium oxide. Then, 37% phosphoric acid gel (Gel S, coltene, Switzerland) was first applied to the enamel margins for 15 s and for an extra 10 s on the cavity interiors, rinsed for 30 s and gently air dried. The universal adhesive One coat7 (coltene,Switzerland) was actively applied for 20 s, gently air-dried for 5 s, and light cured for 10 s. A dual-cured adhesive resin cement (Duocem,Coltene) was injected into the cavity using the auto-mix tip supplied by the manufacturer. The restoration was then placed in the cavity and checked for complete seating with an ultrasonic seating tip (G22, NSK, Japan). The cement was tac light-cured for 2 s to facilitate removal of the interproximal and marginal excess with dental floss, and then light curing was done from all directions each for 40 s, to achieve the final set.
Contact, occlusal checking and finishing and polishing
The proximal contacts were checked with an unwaxed dental floss (Oral-B, USA). The occlusal contacts were adjusted using an articulating paper (Blue Red Combo 0.0028”/71 µm, Crosstex ® International, USA). Finally, finishing was done using fine grit yellow coded tapered with round and flame diamond stones (#368EF, #852EF, Komet, USA) while polishing was done by rubber points (Enhance kit, Dentsply Sirona) operated at low-speed contra-angle handpiece (NAC-EC, NSK, Japan) with a maximum speed 20,000 rpm under water coolant and minimal pressure.
Lithium disilicate indirect restorations
All the steps were repeated as discussed before, except for crystallization and cementation. After milling, the blue un-crystallized milled restorations were trimmed carefully using diamond abrasives at a very low speed to remove excess material at the connection site with the ceramic block, and was checked intra-orally to ensure complete seating of the restoration. The restoration margins were checked along with the proximal and occlusal contacts. The restorations were then introduced into the furnace (CEREC SpeedFire, Dentsply Sirona, Milford, USA). For the crystallization cycle according to the preset firing parameters. After adjustments and cooling of the restorations, they were checked intraorally. The glazing cycle was done according to the preset glazing parameters instructed by the manufacturer [23]. Before cementation, the restoration fitting surface was treated with 4% hydrofluoric acid for 60 s and rinsed with water according to the manufacturer’s instructions. The surface was cleaned with 37% phosphoric acid gel (Gel S)) for 60 s, rinsed and gently dried by the air stream. The Cleaned restoration was then placed in an ultrasonic cleaner filled with distilled water for 4 min [26]. Then it was silanated (Calibra silane) and heated using a furnace for 1 min [28], and universal adhesive was applied (One coat7) according to the manufacturer’s instructions as previously described.
Outcome assessment
The marginal integrity of both nano-hybrid composite blocks (Brilliant Crios) and ceramic blocks (IPS e.max CAD was evaluated by mirror and explorer by two trained calibrated examiners (HS and MF) with more than ten years of clinical experience using modified USPHS criteria [17]. This was performed post-cementation and after 6, 12 and 24 months.
Statistical analysis
Categorical and ordinal data were presented as frequencies and percentages. Categorical data were analyzed using the chi-square test. Ordinal data were analyzed using the Mann-Whitney U test for intergroup comparisons and Freidman’s test followed by the Nemenyi post hoc test for intragroup comparisons. Numerical data were presented as mean and standard deviation values. They were analyzed for normality using the Shapiro-Wilk test. Data were found to be normally distributed and were analyzed using the independent t-test. The significance level was set at p ≤ 0.05 within all tests. Statistical analysis was performed with R statistical analysis software version 4.1.3 for Windows (R Core Team (2022). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.)
Results
Intergroup comparisons for demographic data showed no significant differences between both groups regarding sex (p = 1) and age (p = 0.582). Recruitment started 1/1/2021 and stopped 31/3/2021 after enrollment of target population. Follow-up started 1/1/2023 and was extended till 31/3/2023. All assigned participants received the allocated intervention. 48 participants completed the analysis and were analyzed for the outcomes. Two participants, one from each group, did not show-up during the follow-up period. Participants flow diagram is presented in Fig. 1.
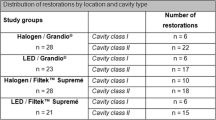
The inter-evaluator reliability had a kappa value 0.98. Frequencies and percentages of outcome scores in both groups are presented in Tables (2–4).
After six months, the inter-group comparison showed a significant difference in marginal integrity between both groups (p < 0.05), with all the cases (100%) in the nano-hybrid composite group having an alpha-1 score, while 80% (n = 20) of the cases in the Emax group had an alpha-1 score and 20% (n = 5) of them had an alpha-3 score. There was also a significant difference in marginal discolouration (p = 0.021), with all cases (100%) in the nano-hybrid composite group having an alpha-1 score. In comparison, in the Emax group, 80% (n=) of the cases (80%) had an alpha-1 score, while 8.0% (n = 2) of the cases had a bravo-1 score and 12.0% (n = 3) of them had a bravo-2 score.
At the 12- and 24-months observation points, there were no differences between the groups as regarding marginal integrity and discolouration (p > 0.05). Regarding the incidence of restoration fracture, there were no differences between either group at all observation points (p > 0.05).
The intra-group comparisons over time showed no differences in marginal integrity, marginal discolouration or incidence of fracture between nano-composite or Emax indirect restorations at all observation points (p = 1).
Discussion
The purpose of this randomized clinical trial was to evaluate the longitudinal clinical performance of ceramic and composite chairside CAD/CAM partial posterior restorations over two years of clinical service.
Several factors contribute to the longevity of indirect restorations, including caries activity, occlusal load, and the clinician’s experience. Therefore, patients with high caries risk index and unusual occlusal habits were excluded from the study [29]. For both types of restoration, the cement gap space was set to 100 μm using Exocad software according to Sokolowski et al. [30] who stated that utilizing a cement layer less than 25 μm, resulted in high hygroscopic expansion stresses, and that exceeding 200 μm generated significant contraction stresses, and that a cement gap of 100 μm appears clinically acceptable. A dual-cure resin cement was used for cementation of the indirect restorations because it can compensate for the limited light transmission, hence enables complete polymerization in areas that are difficult for light penetration [31].
Three important clinical features, marginal integrity, marginal discolouration, and fracture incidence were selected for comparison and monitored over the observation period using the USPHS criteria which was refined to create descriptors with potentially finer discrimination to detect minor changes over time [14]. The modified USPHS criteria have been widely regarded as reliable and standard methods for evaluating the clinical performance of ceramic restorations in various published literature.
[32, 33]. However, it is worth noting that several published studies have suggested that the modified USPHS criteria are less practical and less relevant, with limited sensitivity and categories that may not comprehensively reflect the clinical success of restorations compared to the FDI criteria [34, 35].
Regarding marginal integrity and marginal discoloration, the results of this study showed that initially, all the restorations in both groups had an alpha-1 score. This was predicted due to following all the common principles for indirect adhesive restorations regarding cavity preparation and restoration fabrication. Cavo-surface margin preparation and finishing into intact enamel, an important predictor of restoration survival [36], provided clear cavity margins for accurate scanning. Hence a precise design and fit of the final restoration were achieved, along with following all the literature recommendations regarding the bonding, cementation, finishing and polishing protocols for composite and ceramic restorations. All these factors collectively led to the perfect initial marginal integrity. After six months, a significant difference (p < 0.05) in marginal integrity and marginal discolouration existed between both groups in favour of the restorations milled from the nano-hybrid composite blocks. This is probably attributed to the nature of the materials used, where the ceramic blocks have a higher brittleness index (BI) in comparison to the nano-hybrid composite blocks, which renders them more susceptible to marginal chipping [37]. Also, a purported advantage of the nano-hybrid composites is that they wear at a similar rate to the resin cement, enabling them to maintain good marginal adaptation [14]. Moreover, degradation of the resin-based luting cement is more likely to occur under functional occlusal loading of the ceramic restorations, which have a lower modulus of elasticity than the tooth structure and the nano-hybrid composite material [38]. This agrees Archibald et al. [29] who reported cement wear with consequent marginal discoloration of ceramic indirect restorations at one-year follow-up. Conversely, in a laboratory study, Yildirim et al. [39] reported lower marginal adaptation for the indirect composite restoration (Lava Ultimate) and the hybrid ceramic restoration (Vita Enamic) than for the glass–ceramics (IPS e.max). Yildirim et al. [39] used a CEREC MC XL clinical-type milling unit with a 1.2-mm-diameter rotary instrument. However, smaller-diameter rotary instruments are recommended to capture finer curvature details and achieve more accurate results. Additionally, other variables, such as the virtual space configuration in the software, intrinsic properties of the CAD/CAM system, and speed of the rotary milling instruments, may also affect the outcomes [40].
After 12 and 24 months, there were no significant differences (p > 0.05) in the marginal integrity or marginal discolouration between both groups. This agrees Hassan et al. [40] who reported similar marginal adaptation for ceramic and composite indirect restorations after 2 years. Yet, disagrees Pallesen et al. [41] who reported a superiority for the indirect composite restorations after 11 years, attributed to the smooth interface between the indirect resin restoration and the resin cement, as they have similar mechanical properties.
Fracture of the restorative material has been reported as the main cause of failure in partial indirect restorations in posterior teeth and IPS e.max CAD [42, 43]. Regarding the incidence of restoration fracture in our study, there were no differences between either group at all observation points (p > 0.05). This can be attributed to the good mechanical properties of the used CAD/CAM blocks and the successful bonding of the restorations to the tooth structure. This improves stress distribution and response to the masticatory forces, preventing stress amplification in poorly bonded restorations [29]. Also, the use of the CAD/CAM technology enables control of the thickness of the luting resin cement, hence minimising the negative influence of polymerization shrinkage stresses [44, 45]. This agrees with previous published studies [46, 47]. However, it partially agrees Fasbinder et al. 2019 [14] who reported a higher fracture probability, yet not statistically significant, for Empress CAD onlays than the composite Lava Ultimate onlays after five years of clinical service, and Aslan et al. [48] who reported a minor fracture in a single case restored with a lithium disilicate restoration after one year of clinical follow-up, which also required a partial replacement.
Limitations of the present trial include a lack of standardization of the occlusal load as this is not a split-mouth design. However, patients with wear facets and parafunctional habits were excluded from participation. Also, a longer follow-up period is advised to evaluate the primary and secondary outcomes using modified USPHS criteria. Concerning the marginal integrity, it is recommended not to rely on clinical examination only, but also, it can be supported with the investigation of image analysis of scanned replicas.
In conclusion, the proposed null hypothesis should be accepted concerning the clinical performance after two years of recall as both CAD/CAM restorative materials evaluated exhibited a similar clinical performance after two years of service that need to be confirmed in long-term evaluations. This aligns with the results of previous studies [32, 46, 49, 50]. A recent systematic review also emphasized that indirect resin-based composite restorations are dependable materials for partial-coverage restorations, with clinical performance comparable to that of glass–ceramic restorations [15, 40].
Clinical relevance: The CAD/CAM nano-hybrid composite blocks are as reliable as Lithium disilicate for restoring mutilated vital teeth. However, clinicians must know the lack of knowledge regarding longer-term outcomes.
Data availability
Data are available from the corresponding author upon reasonable request and with permission of Cairo University - faculty of Dentistry.
References
Angeletaki F, Gkogkos A, Papazoglou E, Kloukos D. Direct versus indirect inlay/onlay composite restorations in posterior teeth. A systematic review and meta-analysis. J Dent. 2016;53:12.
Opdam NJM, Frankenberger R, Magne P. From ‘Direct Versus Indirect’’ toward an Integrated Restorative Concept in the posterior dentition’. Oper Dent. 2016;41(S7):27–S34.
Cetin AR, Unlu N, Cobanoglu N. A five-year clinical evaluation of direct Nanofilled and Indirect Composite Resin restorations in posterior teeth. Oper Dent. 2013;38:E31–41.
Abduo J, Sambrook RJ. Longevity of ceramic onlays: a systematic review. J Esthet Rest Dent. 2018;30:193.
Vichi A, Balestra D, Scotti N, Louca C, Paolone G. Translucency of CAD/CAM and 3D printable composite materials for Permanent Dental restorations. Polymers. 2023;15:1443.
Lubauer J, Belli R, Peterlik H, Hurle K, Lohbauer U. Grasping the Lithium hype: insights into modern dental Lithium Silicate glass-ceramics. Dent Mater. 2022;38:318.
Munoz A, Zhao Z, Paolone G, Louca C, Vichi A. Flexural strength of CAD/CAM Lithium-based Silicate Glass–Ceramics: a narrative review. Materials. 2023;16:4398.
Mangoush E, Lassila L, Vallittu PK, Garoushi S. Microstructure and surface characteristics of short-fiber reinforced CAD/CAM composite blocks. Eur J Prosthodont Restor Dent. 2021;29:166.
Maier E, Grottschreiber C, Knepper I, Opdam N, Petschelt A, Loomans B, Lohbauer U. Evaluation of wear behavior of dental restorative materials against zirconia in vitro. Dent Mater. 2022;38:778.
Elsahn NA, El-Damanhoury HM, Shirazi Z, Saleh ARM. Surface properties and wear resistance of Injectable and computer-aided Design/Computer aided Manufacturing-Milled Resin Composite Thin Occlusal Veneers. Eur J Dent. 2023;17:663.
Zhang Y, Kelly JR. Dental Ceramics for Restoration and Metal Veneering. Dent Clin North Am. 2017;61:797.
Ruse ND, Sadoun MJ. Resin-composite blocks for Dental CAD/CAM applications. J Dent Res. 2014;93:1232.
Moshaverinia A. Review of the Modern Dental Ceramic Restorative materials for Esthetic Dentistry in the minimally invasive age. Dent Clin North Am. 2020;64:621.
Fasbinder DJ, Neiva GF, Heys D, Heys R. Clinical evaluation of chairside computer assisted Design/Computer assisted Machining nano-ceramic restorations: five-year status. J Esthet Restor Dent. 2020;32:193–203.
Fathy H, Hamama HH, El-Wassefy N, Mahmoud SH. Clinical performance of resin-matrix ceramic partial coverage restorations: a systematic review. Clin Oral Investig. 2022;26:3807.
Bustamante-Hernández N, Montiel-Company JM, Bellot-Arcís C, Mañes-Ferrer JF, Solá-Ruíz MF, Agustín-Panadero R, Fernández-Estevan L. Clinical behavior of Ceramic, Hybrid and Composite Onlays. A systematic review and Meta-analysis. Int J Environ Res Public Health. 2020;17:7582.
Fasbinder DJ, Dennison JB, Heys DR, Lampe K. The clinical performance of CAD/CAM-generated composite inlays. J Am Dent Assoc. 2005;136:1714.
Krifka S, Anthofer T, Fritzsch M, Hiller KA, Schmalz G, Federlin M. Ceramic inlays and partial ceramic crowns: influence of remaining cusp wall thickness on the marginal integrity and enamel crack formation in vitro. Oper Dent. 2009;34:32.
El-Housseiny AA, Farsi N. Sealing ability of a single bond adhesive in primary teeth. An in vivo study. Int J Paediatr Dent. 2002;12:265.
Schwendicke F, Frencken J, Innes N. Current concepts in Carious tissue removal. Curr Oral Health Rep. 2018;5:154.
Veneziani M. Posterior indirect adhesive restorations: updated indications and the morphology Driven Preparation technique. Int J Esthet Dent. 2017;12:2014.
Rocca GT, Rizcalla N, Krejci I, Dietschi D. Clinical Research Clinical Research evidence-based concepts and procedures for bonded inlays and onlays. Part II. Updated guidelines for cavity preparation and restoration fabrication. Int J Esthet Dent. 2015;10:392.
Aboudorra HA, Amr H, El zohairy A, Hafez A, Hassan A. Internal fit evaluation of all ceramic restoration fabricated by two CAD/CAM milling systems using cone beam CT (CBCT). Egypt Dent J. 2019;65:2467.
Dillenburg ALK, Soares CG, Paranhos MPG, Spohr AM, Loguercio AD, Burnett LH. Microtensile bond strength of prehybridized dentin: storage time and surface treatment effects. J Adhes Dent. 2009;11:231.
Yoshihara K, Nagaoka N, Maruo Y, Nishigawa G, Irie M, Yoshida Y, et al. Sandblasting may damage the surface of composite CAD-CAM blocks. Dent Mater. 2017;33:e124–35.
Kim HJ, Kim S, You SH, Cho SG, Choi KK, Kim DS. Effects of silane treatment on salivary protein contamination during the bonding of lithium disilicate ceramic. J Adhes Sci Technol. 2020;34:1885.
Araoka D, Hosaka K, Nakajima M, Foxton R, Thanatvarakorn O, Prasansuttiporn T, et al. The strategies used for curing universal adhesives affect the micro-bond strength of resin cement used to lute indirect resin composites to human dentin. Dent Mater J. 2018;37:506.
Silva UPC, Maia AP, Silva ID, Miranda ME, Brandt WC. Influence of the multiple layers application and the heating of silane on the bond strength between Lithium Disilicate Ceramics and Resinous Cement. Eur J Dent. 2021;15:720.
Archibald JJ, Santos GC Jr, Moraes-Coelho-Santos MJ. Retrospective clinical evaluation of ceramic onlays placed by dental students. J Prosthet Dent. 2018;119:743–8e1.
Sokolowski G, Krasowski M, Szczesio-Wlodarczyk A. The influence of cement layer thickness on the stress state of metal inlay restorations-photoelastic analysis. Mater (Basel). 2021;14:599.
Al-Haj-Husain NzcanM, Molinero-Mourelle P, Joda T. Clinical performance of partial and full-coverage fixed dental restorations fabricated from hybrid polymer and ceramic CAD/CAM materials: a systematic review and meta-analysis. J Clin Med. 2020;9:2107.
Coşkun E, Aslan YU, zkan YK. Evaluation of two different CAD-CAM inlay-onlays in a split-mouth study: 2-year clinical follow-up. J Esthet Restor Dent. 2020;32:244.
Saavedra G, Tribst JPM. Feldspathic and lithium disilicate onlays with a 2-year follow-up: split-mouth randomized clinical trial. Braz Dent J. 2021;32:53.
Marquillier T, Dom.jean S, Le Clerc J, Chemla F, Gritsch K, Maurin JC, et al. The use of FDI criteria in clinical trials on direct dental restorations: a scoping review. J Dent. 2018;68:1.
Hickel R, Peschke A, Tyas M, Mj.r I, Bayne S, Peters M, et al. FDI World Dental Federation: clinical criteria for the evaluation of direct and indirect restorations-update and clinical examples. Clin Oral Investig. 2010;14:349.
Collares K, Corrêa MB, Laske M, Kramer E, Reiss B, Moraes RR, et al. A practice-based research network on the survival of ceramic inlay/onlay restorations. Dent Mater. 2016;32:687.
Tsitrou EA, Helvatjoglu-Antoniades M, van Noort R. A preliminary evaluation of the structural integrity and fracture mode of minimally prepared resin bonded CAD/CAM crowns. J Dent. 2010;38:16.
Ibrahim SH, Amr H, Hassan AA, Elzohairy A. Internal fit evaluation of indirect restorations fabricated from CAD/CAM composite blocks versus ceramic blocks in badly broken teeth using cone beam CT (CBCT): double-blinded randomized clinical trial. Heliyon. 2022;8:e09466.
Yildirim G, Uzun IH, Keles A. Evaluation of marginal and internal adaptation of hybrid and nanoceramic systems with microcomputed tomography: an in vitro study. J Prosthet Dent. 2017;118:200.
Hassan A, Hamdi K, Ali AI, et al. Clinical performance comparison between lithium disilicate and hybrid resin nano-ceramic CAD/CAM onlay restorations: a two-year randomized clinical split-mouth study. Odont. 2023. https://doi.org/10.1007/s10266-023-00841-w.
Pallesen U, Qvist V. Composite resin fillings and inlays. An 11-year evaluation. Clin Oral Investig. 2003;7:71.
Morimoto S, Rebello De Sampaio FBW, Braga MM, Sesma N, Özcan M. Survival rate of Resin and Ceramic Inlays, Onlays, and overlays: a systematic review and Meta-analysis. J Dent Res. 2016;95:985.
Alsaeed AY. Bonding CAD/CAM materials with current adhesive systems: an overview. Saudi Dent J. 2022;34:259.
Putzeys E, Vercruyssen C, Duca RC, Saha PS, Godderis L, Vanoirbeek J, et al. Monomer release from direct and indirect adhesive restorations: a comparative in vitro study. Dent Mater. 2020;36:1275.
Qanungo A, Aras MA, Chitre V, Mysore A, Amin B, Daswani SR. Immediate dentin sealing for indirect bonded restorations. J Prosth Res. 2016;60:240.
Souza J, Fuentes MV, Baena E, Ceballos L. One-year clinical performance of lithium disilicate versus resin composite CAD/CAM onlays. Odont. 2021;109:259.
Tunac AT, Celik EU. Two-year performance of CAD/CAM fabricated resin composite inlay restorations: a randomized controlled clinical trial. J Esthet Restor Dent. 2019;31:627.
Aslan YU, Coskun E, Ozkan Y, Dard M. Clinical evaluation of three types of CAD/CAM Inlay/ onlay materials after 1-Year clinical follow up. Eur J Prosth Restor Dent. 2019;27:131.
Edelhoff D, Güth JF, Erdelt K, Brix O, Liebermann A. Clinical performance of occlusal onlays made of lithium disilicate ceramic in patients with severe tooth wear up to 11 years. Dent Mater. 2019;35:1319.
Abdulrahman S, Von See MC, Talabani R, Abdulateef D. Evaluation of the clinical success of four different types of lithium disilicate ceramic restorations: a retrospective study. BMC Oral Health. 2021;21:625.
Acknowledgements
Not applicable.
Funding
Self-funded.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
All authors (HA, OH, MH and ME) contributed to the conception, design and execution of the study. HA, MH and SS drafted the work and substantively revised it. All authors have viewed and approved the initially submitted version and have agreed to be personally accountable to the submitted work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval of the study design was provided by the Research Ethics Committee at Cairo University, Egypt (CREC) (approval number: 16-9-20, Date: 29-09-2020).
Consent for publication
Not applicable.
Competing interests
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Elmoselhy, H.A.S., Hassanien, O.E.S., Haridy, M.F. et al. Two‑year clinical performance of indirect restorations fabricated from CAD/CAM nano hybrid composite versus lithium disilicate in mutilated vital teeth. A randomized controlled trial. BMC Oral Health 24, 101 (2024). https://doi.org/10.1186/s12903-023-03847-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03847-6