Abstract
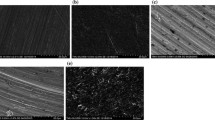
Dental implants are prone to bacterial colonization which may result in bone destruction and implant loss. Treatments of peri-implant disease aim to reduce bacterial adherence while leaving the implant surface intact for attachment of bone-regenerating host cells. The aims of this study were to investigate the antimicrobial efficacy of gaseous ozone on bacteria adhered to various titanium and zirconia surfaces and to evaluate adhesion of osteoblast-like MG-63 cells to ozone-treated surfaces. Saliva-coated titanium (SLA and polished) and zirconia (acid etched and polished) disks served as substrates for the adherence of Streptococcus sanguinis DSM20068 and Porphyromonas gingivalis ATCC33277. The test specimens were treated with gaseous ozone (140 ppm; 33 mL/s) for 6 and 24 s. Bacteria were resuspended using ultrasonication, serially diluted and cultured. MG-63 cell adhesion was analyzed with reference to cell attachment, morphology, spreading, and proliferation. Surface topography as well as cell morphology of the test specimens were inspected by SEM. The highest bacterial adherence was found on titanium SLA whereas the other surfaces revealed 50–75% less adherent bacteria. P. gingivalis was eliminated by ozone from all surfaces within 24 s to below the detection limit (≥99.94% reduction). S. sanguinis was more resistant and showed the highest reduction on zirconia substrates (>90% reduction). Ozone treatment did not affect the surface structures of the test specimens and did not influence osteoblastic cell adhesion and proliferation negatively. Titanium (polished) and zirconia (acid etched and polished) had a lower colonization potential and may be suitable material for implant abutments. Gaseous ozone showed selective efficacy to reduce adherent bacteria on titanium and zirconia without affecting adhesion and proliferation of osteoblastic cells. This in vitro study may provide a solid basis for clinical studies on gaseous ozone treatment of peri-implantitis and revealed an essential base for sufficient tissue regeneration.






Similar content being viewed by others
References
Al-Nawas B, Kämmerer PW, Morbach T, Ladwein C, Wegener J, Wagner W (2010) Ten-year retrospective follow-up study of the TiOblast dental implant. Clin Implant Dent Relat Res. doi:10.1111/j.1708-8208.2009.00237.x
Jemt T (2008) Single implants in the anterior maxilla after 15 years of follow-up: comparison with central implants in the edentulous maxilla. Int J Prosthodont 21:400–408
Buddula A, Assad DA, Salinas TJ, Garces YI, Volz JE, Weaver AL (2010) Survival of dental implants in irradiated head and neck cancer patients: a retrospective analysis. Clin Implant Dent Relat Res. doi:10.1111/j.1708-8208.2010.00307.x
Karoussis IK, Muller S, Salvi GE, Heitz-Mayfield LJ, Bragger U, Lang NP (2004) Association between periodontal and peri-implant conditions: a 10-year prospective study. Clin Oral Implants Res 15:1–7
Berglundh T, Gislason O, Lekholm U, Sennerby L, Lindhe J (2004) Histopathological observations of human peri-implantitis lesions. J Clin Periodontol 31:341–347
Albrektsson T, Isidor F (1994) Consensus report: implant therapy. In: Lang NP, Karring T (eds) Proceedings of the 1st European Workshop on Periodontology. Quintessence Publishing Co Ltd, London, pp 365–369
Quirynen M, De Soete M, van Steenberghe D (2002) Infectious risks for oral implants: a review of the literature. Clin Oral Implants Res 13:1–19
Costerton JW, Montanaro L, Arciola CR (2005) Biofilm in implant infections: its production and regulation. Int J Artif Organs 28:1062–1068
Teughels W, Van Assche N, Sliepen I, Quirynen M (2006) Effect of material characteristics and/or surface topography on biofilm development. Clin Oral Implant Res 17:68–81
Norowski PA, Bumgardner JD (2009) Biomaterial and antibiotic strategies for peri-implantitis: a review. J Biomed Mater Res B Appl Biomater 88:530–543
Schwarz F, Bieling K, Sculean A, Herten M, Becker J (2004) Treatment of periimplantitis with laser or ultrasound. A review of the literature (Article in German). Schweiz Monatsschr Zahnmed 114:1228–1235
Renvert S, Roos-Jansåker AM, Claffey N (2008) Non-surgical treatment of peri-implant mucositis and peri-implantitis: a literature review. J Clin Periodontol 35(8 Suppl):305–315
Roos-Jansåker AM, Renvert S, Egelberg J (2003) Treatment of peri-implant infections: a literature review. J Clin Periodontol 30:467–485
Persson GR, Samuelsson E, Lindahl C, Renvert S (2010) Mechanical non-surgical treatment of peri-implantitis: a single-blinded randomized longitudinal clinical study. II. Microbiological results. J Clin Periodontol 37:563–573
Mouhyi J, Sennerby L, Pireaux JJ, Dourov N, Nammour S, Van Reck J (1998) An XPS and SEM evaluation of six chemical and physical techniques for cleaning of contaminated titanium implants. Clin Oral Implants Res 9:185–194
Mouhyi J, Sennerby L, Wennerberg A, Louette P, Dourov N, van Reck J (2000) Re-establishment of the atomic composition and the oxide structure of contaminated titanium surfaces by means of carbon dioxide laser and hydrogen peroxide: an in vitro study. Clin Implant Dent Relat Res 2:190–202
Deppe H, Horch HH (2007) Laser applications in oral surgery and implant dentistry. Lasers Med Sci 22:217–221
Stübinger S, Sader R, Filippi A (2006) The use of ozone in dentistry and maxillofacial surgery: a review. Quintessence Int 37:353–359
Azarpazhooh A, Limeback H (2008) The application of ozone in dentistry: a systematic review of literature. J Dent 36:104–116
Emerson M, Sprone OJ, Buck CE (1982) Ozone inactivation of cell-associated viruses. Appl Environ Microbiol 43:603–608
Dyas A, Boughton BJ, Das BC (1983) Ozone killing action against bacterial and fungal species; microbiological testing of a domestic ozone generator. J Clin Pathol 36:1102–1104
Persson LG, Berglundh T, Lindhe J, Sennerby L (2001) Re-osseointegration after treatment of peri-implantitis at different implant surfaces. An experimental study in the dog. Clin Oral Implants Res 12:595–603
Ivanoff CJ, Sennerby L, Lekholm U (1996) Influence of soft tissue contamination on the integration of titanium implants. An experimental study in rabbits. Clin Oral Implant Res 7:128–132
Bowers KT, Keller JC, Randolph BA, Wick DC, Michaels CM (1992) Optimization of surface micromorphology for enhanced osteoblast responses in vitro. Int J Oral Maxillofac Implants 73:302–310
Filippi A (2001) Der Einfluss von ozoniertem Wasser auf die epitheliale Wundheilung. Dtsch Zahnärztl Z 56:104–108
Hisbergues M, Vendeville S, Vendeville P (2008) Zirconia: established facts and perspectives for a biomaterial in dental implantology. J Biomed Mater Res B Appl Biomater 88:519–529
Hauser-Gerspach I, Kulik EM, Weiger R, Decker E-M, Von Ohle C, Meyer J (2007) Adhesion of Streptococcus sanguinis to dental implant and restorative materials. Dent Mater J 26:361–366
Hauser-Gerspach I, Stübinger S, Meyer J (2010) Bactericidal effects of different laser systems on bacteria adhered to dental implant surfaces. An in vitro study comparing zirconia to titanium. Clin Oral Implant Res 21:277–283
Sardin S, Morrier J-J, Benay G, Barsotti O (2004) In vitro streptococcal adherence on prosthetic and implant materials. Interactions with physicochemical surface properties. J Oral Rehab 31:140–148
Mabboux F, Ponsonnet L, Morrier JJ, Jaffrezic N, Barsotti O (2004) Surface free energy and bacterial retention to saliva-coated dental implant materials–an in vitro study. Colloids Surf B Biointerfaces 39:199–205
Hems RS, Gulabivala K, Ng YL, Ready DR, Spratt DA (2005) An in vitro evaluation of the ability of ozone to kill a strain of Enterococcus faecalis. Int Endod J 38:22–29
Müller P, Guggenheim B, Schmidlin PR (2007) Efficacy of gasiform ozone and photodynamic therapy on a multispecies oral biofilm in vitro. Eur J Oral Sci 115:77–80
Hauser-Gerspach I, Pfäffli-Savtchenko V, Dähnhardt JE, Meyer J, Lussi A (2009) Comparison of the immediate effects of gaseous ozone and chlorhexidine gel on bacteria in cavitated carious lesions in children in vivo. Clin Oral Invest 13:287–291
Baysan A, Beighton D (2007) Assessment of the ozone-mediated killing of bacteria in infected dentine associated with non-cavitated occlusal carious lesions. Caries Res 41:337–341
Kuştarci A, Sümer Z, Altunbaş D, Koşum S (2009) Bactericidal effect of KTP laser irradiation against Enterococcus faecalis compared with gaseous ozone: an ex vivo study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107:e73–e79
Huth KC, Quirling M, Maier S, Kamereck K, Alkhaye M, Paschos E, Welsch U, Miethke T, Brand K, Hickel R (2009) Effectiveness of ozone against endodontopathogenic microorganisms in a root canal biofilm model. Int Endod J 42:3–13
Stoll R, Venne L, Jablonski-Momeni A, Mutters R, Stachniss V (2008) The disinfecting effect of ozonized oxygen in an infected root canal: an in vitro study. Quintessence Int 39:231–236
van Winkelhoff AJ, Goené RJ, Benschop C, Folmer T (2000) Early colonization of dental implants by putative periodontal pathogens in partially edentulous patients. Clin Oral Implants Res 11:511–521
Heuer W, Elter C, Demling A, Neumann A, Suerbaum S, Hannig M, Heidenblut T, Bach FW, Stiesch-Scholz M (2007) Analysis of early biofilm formation on oral implants in man. J Oral Rehabil 34:377–382
Millar BJ, Hodson N (2007) Assessment of the safety of two ozone delivery devices. J Dent 35:195–200
Deligianni DD, Katsala ND, Ladas S, Sotiropoulou D, Amedee J, Missirlis YF (2001) Effect of surface roughness of the titanium alloy Ti-6Al-4 V on human bone marrow cell response and on protein adsorption. Biomaterials 22:1241–1251
Zhao G, Raines AL, Wieland M, Schwartz Z, Boyan BD (2007) Requirement for both micron- and submicron scale structure for synergistic responses of osteoblasts to substrate surface energy and topography. Biomaterials 28:2821–2829
Boyan BD, Lossdörfer S, Wang L, Zhao G, Lohmann CH, Cochran DL, Schwartz Z (2003) Osteoblasts generate an osteogenic microenvironment when grown on surfaces with rough microtopographies. Eur Cell Mater 24:22–27
Rausch-Fan X, Qu Z, Wieland M, Matejka M, Schedle A (2008) Differentiation and cytokine synthesis of human alveolar osteoblasts compared to osteoblast-like cells (MG63) in response to titanium surfaces. Dent Mater 24:102–110
Setzer B, Bächle M, Metzger MC, Kohal RJ (2009) The gene-expression and phenotypic response of hFOB 1.19 osteoblasts to surface-modified titanium and zirconia. Biomaterials 30:979–990
Martin JY, Schwartz Z, Hummert TW, Schraub DM, Simpson J, Lankford JJ, Dean DD, Cochran DL, Boyan BD (1995) Effect of titanium surface roughness on proliferation, differentiation, and protein synthesis of human osteoblast-like cells (MG63). J Biomed Mater Res 29:389–401
Acknowledgements
We thank the ITI Foundation, Switzerland, (Grant No.: 518/2007) and the SSO Fonds (grant no.: 248–09) for financial support and TIP TOP TIPS Sàrl, Rolle, Switzerland, for supplying the ozone equipment.
Conflict of interests
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hauser-Gerspach, I., Vadaszan, J., Deronjic, I. et al. Influence of gaseous ozone in peri-implantitis: bactericidal efficacy and cellular response. An in vitro study using titanium and zirconia. Clin Oral Invest 16, 1049–1059 (2012). https://doi.org/10.1007/s00784-011-0603-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-011-0603-2