Abstract
Introduction
The aim of this study was to evaluate the in vitro osteogenic potential of osteoblasts from neural crest-derived frontal bone (OB-NC) and mesoderm-derived parietal bone (OB-MS) and the bone formation induced by them when injected into calvarial defects.
Materials and methods
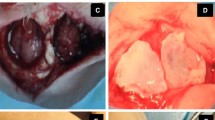
Calvarial bones were collected from newborn Wistar rats (3-day old) and characterized as frontal and parietal prior to OB-NC and OB-MS harvesting. The cells were cultured, and several parameters of osteoblast differentiation were evaluated. These cells, or PBS without cells (control), were locally injected into 5-mm rat calvarial defects (5 × 106 cells/defect) and after 4 weeks bone formation was evaluated by morphometric and histological analyses.
Results
The characterization of frontal and parietal bones assured the different embryonic origin of both cell populations, OB-NC and OB-MS. The OB-NC presented higher proliferation while the OB-MS presented higher alkaline phosphatase (ALP) activity, extracellular matrix mineralization and gene expression of runt-related transcription factor 2, Alp, bone sialoprotein and osteocalcin revealing their high osteogenic potential. µCT analysis indicated that there was higher amount of bone formation in defects injected with both OB-NC and OB-MS compared to the control. Moreover, the bone tissue formed by both cells displayed the same histological characteristics.
Conclusions
Despite the distinct in vitro osteogenic potential, OB-NC and OB-MS induced similar bone repair in a rat calvarial defect model. Thus, osteoblasts, irrespective of their in vitro osteogenic potential linked to embryonic origins, seem to be suitable for cell-based therapies aiming to repair bone defects.






Similar content being viewed by others
References
Khan SN, Cammisa FPJ, Sandhu HS, Diwan AD, Girardi FP, Lane JM (2005) The biology of bone grafting. J Am Acad Orthop Surg 13:77–86
Rosa AL, de Oliveira PT, Beloti MM (2008) Macroporous scaffolds associated with cells to construct a hybrid biomaterial for bone tissue engineering. Expert Rev Med Devices 5:719–728
Brydone AS, Meek D, Maclaine S (2010) Bone grafting, orthopaedic biomaterials, and the clinical need for bone engineering. Proc Inst Mech Eng H 224:1329–1343
Zheng GS, Su YX, Liao GQ, Chen ZF, Wang L, Jiao PF, Liu HC, Zhong YQ, Zhang TH, Liang YJ (2012) Mandible reconstruction assisted by preoperative virtual surgical simulation. Oral Surg Oral Med Oral Pathol Oral Radiol 113:604–611
Younger EM, Chapman MW (1989) Morbidity at bone graft donor sites. J Orthop Trauma 3:192–195
Kappe T, Cakir B, Mattes T, Reichel H, Flören M (2010) Infections after bone allograft surgery: a prospective study by a hospital bone bank using frozen femoral heads from living donors. Cell Tissue Bank 11:253–259
Zwingenberger S, Nich C, Valladares RD, Yao Z, Stiehler M, Goodman SB (2012) Recommendations and considerations for the use of biologics in orthopedic surgery. BioDrugs 26:245–256
Lichte P, Pape H, Pufe T, Kobbe P, Fischer H (2011) Scaffolds for bone healing: concepts, materials and evidence. Injury 42:569–573
Marx RE (2007) Bone and bone graft healing. Oral Maxillofac Surg Clin N Am 19:455–466
Walmsley GG, Ransom RC, Zielins ER, Leavitt T, Flacco JS, Hu MS, Lee AS, Longaker MT, Wan DC (2016) Stem cells in bone regeneration. Stem Cell Rev 12:524–529
Dimitriou R, Jones E, McGonagle D, Giannoudis PV (2011) Bone regeneration: current concepts and future directions. BMC Med 9:66
Sadri-Ardekani H, Atala A (2016) Regenerative medicine. Methods 99:1–2
Buzhor E, Leshansky L, Blumenthal J, Barash H, Warshawsky D, Mazor Y, Shtrichman R (2014) Cell-based therapy approaches: the hope for incurable diseases. Regen Med 9:649–672
Salgado AJ, Oliveira JM, Martins A, Teixeira FG, Silva NA, Neves NM, Souza N, Reis RL (2013) Tissue engineering and regenerative medicine: past, present, and future. Int Rev Neurobiol 108:1–33
Roddy E, DeBaun MR, Daoud-Gray A, Yang YP, Gardner MJ (2018) Treatment of critical-sized bone defects: clinical and tissue engineering perspectives. Eur J Orthop Surg Traumatol 28:351–362
Toogood P, Miclau T (2017) Critical-sized bone defects: sequence and planning. J Orthop Trauma 31:S23–S26
Keating JF, Simpson AH, Robinson CM (2005) The management of fractures with bone loss. J Bone Jt Surg Br 87:142–150
Fu Y, Karbaat L, Wu L, Leijten J, Both SK, Karperien M (2017) Trophic effects of mesenchymal stem cells in tissue regeneration. Tissue Eng Part B Rev 23:515–528
Ding DC, Chang YH, Shyu WC, Lin SZ (2015) Human umbilical cord mesenchymal stem cells: a new era for stem cell therapy. Cell Transpl 24:339–347
Bianco P, Robey PG, Simmons PJ (2008) Mesenchymal stem cells: revisiting history, concepts, and assays. Cell Stem Cell 2:313–319
Freitas GP, Lopes HB, Almeida ALG, Abuna RPF, Gimenes R, Souza LEB, Covas DT, Beloti MM, Rosa AL (2017) Potential of osteoblastic cells derived from bone marrow and adipose tissue associated with a polymer/ceramic composite to repair bone tissue. Calcif Tissue Int 101:312–320
De Santana ST, Abuna RP, Bacha Lopes H, Goncalves de Almeida AL, Beloti MM, Luiz Rosa A (2015) Association of mesenchymal stem cells and osteoblasts for bone repair. Regen Med 10:127–133
Beloti MM, Sicchieri LG, de Oliveira PT, Rosa AL (2012) The influence of osteoblast differentiation stage on bone formation in autogenously implanted cell-based poly(lactide-co-glycolide) and calcium phosphate constructs. Tissue Eng Part A 18:999–1005
Souza ATP, Freitas GP, Lopes HB, Ferraz EP, Oliveira FS, Beloti MM, Rosa AL (2018) Effect of cell therapy with allogeneic osteoblasts on bone repair of rat calvaria defects. Cytotherapy 20:1267–1277
Freitas GP, Lopes HB, Souza ATP, Oliveira PGFP, Almeida ALG, Souza LEB, Coelho PG, Beloti MM, Rosa AL (2019) Cell therapy: effect of locally injected mesenchymal stromal cells derived from bone marrow or adipose tissue on bone regeneration of rat calvarial defects. Sci Rep 9:13476
Chai Y, Jiang X, Ito Y, Bringas P Jr, Han J, Rowitch DH, Soriano P, McMahon AP, Sucov HM (2000) Fate of the mammalian cranial neural crest during tooth and mandibular morphogenesis. Development 127:1671–1679
Jiang X, Iseki S, Maxson RE, Sucov HM, Morriss-Kay GM (2002) Tissue origins and interactions in the mammalian skull vault. Dev Biol 24:106–116
Li S, Quarto N, Senarath-Yapa K, Grey N, Bai X, Longaker MT (2015) Enhanced activation of canonical Wnt signalling confers mesoderm-derived parietal bone with similar osteogenic and skeletal healing capacity to neural crest-derived frontal bone. PLoS ONE 10:e0138059. https://doi.org/10.1371/journal.pone.0138059
Quarto N, Wan DC, Kwan MD, Panetta NJ, Li S, Longaker MT (2010) Origin matters: differences in embryonic tissue origin and Wnt signalling determine the osteogenic potential and healing capacity of frontal and parietal calvarial bones. J Bone Miner Res 25:1680–1694
Hu B, Wu T, Zhao Y, Xu G, Shen R, Chen G (2017) Physiological signatures of dual embryonic origins in mouse skull vault. Cell Physiol Biochem 43:2525–2534
Li S, Quarto N, Longaker MT (2010) Activation of FGF signalling mediates proliferative and osteogenic differences between neural crest derived frontal and mesoderm parietal derived bone. PLoS ONE 5:e14033. https://doi.org/10.1371/journal.pone.0014033
Orimo H (2010) The mechanism of mineralization and the role of alkaline phosphatase in health and disease. J Nippon Med Sch 77:4–12
Li S, Meyer NP, Quarto N, Longaker MT (2013) Integration of multiple signalling regulates through apoptosis the differential osteogenic potential of neural crest-derived and mesoderm-derived osteoblasts. PLoS ONE 8:e58610. https://doi.org/10.1371/journal.pone.0058610
Bonilla-Claudio M, Wang J, Bai Y, Klysik E, Selever J, Martin JF (2012) BMP signaling regulates a dose-dependent transcriptional program to control facial skeletal development. Development 139:709–719
Haversath M, Catelas I, Li X, Tassemeier T, Jäger M (2012) PGE2 and BMP-2 in bone and cartilage metabolism: 2 intertwining pathways. Can J Physiol Pharmacol 90:1434–1445
Lee MH, Kim YJ, Kim HJ, Park HD, Kang AR, Kyung HM, Sung JH, Wozney JM, Kim HJ, Ryoo HM (2003) BMP-2-induced Runx2 expression is mediated by Dlx5, and TGF-beta 1 opposes the BMP-2-induced osteoblast differentiation by suppression of Dlx5 expression. J Biol Chem 278:34387–34394
Tadic T, Dodig M, Erceg I, Marijanovic I, Mina M, Kalajzic Z, Velonis D, Kronenberg MS, Kosher RA, Ferrari D, Lichtler AC (2002) Overexpression of Dlx5 in chicken calvarial cells accelerates osteoblastic differentiation. J Bone Miner Res 17:1008–1014
Miyama K, Yamada G, Yamamoto TS, Takagi C, Miyado K, Sakai M, Ueno N, Shibuya H (1999) A BMP-inducible gene, dlx5, regulates osteoblast differentiation and mesoderm induction. Dev Biol 208:123–133
Ryoo HM, Hoffmann HM, Beumer T, Frenkel B, Towler DA, Stein GS, Stein JL, van Wijnen AJ, Lian JB (1997) Stage-specific expression of Dlx-5 during osteoblast differentiation: involvement in regulation of osteocalcin gene expression. Mol Endocrinol 11:1681–1694
Mokhtari R, Lachman HM (2016) The major histocompatibility complex (MHC) in schizophrenia: a review. J Clin Cell Immunol 7:479. https://doi.org/10.4172/2155-9899.1000479
Doherty PC, Topham DJ, Tripp RA, Cardin RD, Brooks JW, Stevenson PG (1997) Effector CD4 and CD8 T-cell mechanisms in the control of respiratory virus infections. Immunol Rev 159:105–117
Schrum LW, Bost KL, Hudson MC, Marriott I (2003) Bacterial infection induces expression of functional MHC class II molecules in murine and human osteoblasts. Bone 33:812–882
Reyes-Botella C, Montes MJ, Vallecillo-Capilla MF, Olivares EG, Ruiz C (2002) Antigenic phenotype of cultured human osteoblast-like cells. Cell Physiol Biochem 12:359–364
Heinemann DE, Lohmann C, Siggelkow H, Alves F, Engel I, Koster G (2000) Human osteoblast-like cells phagocytose metal particles and express the macrophage marker CD68 in vitro. J Bone Jt Sur Br 82:283–289
Khoury EL, Arnaud CD (1993) Alkaline phosphatase-positive human osteoblasts do not normally express MHC class II antigens in vivo. Bone 14:289–295
Skjodt H, Moller T, Freiesleben SF (1989) Human osteoblast-like cells expressing MHC class II determinants stimulate allogeneic and autologous peripheral blood mononuclear cells and function as antigen presenting cells. Immunology 68:416–420
Zhou Y, Huang R, Fan W, Prasadam I, Crawford R, Xiao Y (2018) Mesenchymal stromal cells regulate the cell mobility and the immune response during osteogenesis through secretion of vascular endothelial growth factor A. J Tissue Eng Regen Med 12:e566–e578
Acknowledgements
Fabiana Rossetto de Moraes and Roger Rodrigo Fernandes are acknowledged for technical assistance during the experiments. This research was supported by the Coordination for the Improvement of Higher Education Personnel (CAPES, Grant # 00.889.834/0001-08), National Council for Scientific and Technological Development (CNPq, Grant # 404318/2016-9) and São Paulo Research Foundation (FAPESP, Grants # 2009/54142-5 and 2015/21439-6).
Author information
Authors and Affiliations
Contributions
ATPS undertook the experiments, analysed the data and drafted the manuscript. HBL and GPF worked with animal experiments, analysed the data and revised the manuscript. EPF, FSO and DW worked with in vitro experiments and revised the manuscript. ALGA performed the histological and microtomographic analysis and revised the manuscript. MMB and ALR designed the study, analysed the data and drafted the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
Animal rights
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. The Committee of Ethics in Animal Research of the School of Dentistry of Ribeirão Preto, University of São Paulo approved all animal procedures performed during the experiments (Protocol # 2016.668.58.0, approved on September 21th, 2016).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
774_2020_1090_MOESM3_ESM.tif
Fig. S1 Gene expression of the bone morphogenetic proteins 2 (Bmp2, a) and 4 (Bmp4, b), and distal-less homeobox 5 (Dlx5, c) in osteoblasts derived from neural crest (frontal bone, OB-NC) and mesoderm (parietal bone, OB-MS) of newborn rats, grown under osteogenic conditions, on 3, 7 and 10 days. Asterisks (*) indicate statistically significant differences (ANOVA, p≤0.05). Data are presented as mean ± standard deviation (n=3) (TIF 2026 kb)
About this article
Cite this article
Souza, A.T.P., Lopes, H.B., Freitas, G.P. et al. Role of embryonic origin on osteogenic potential and bone repair capacity of rat calvarial osteoblasts. J Bone Miner Metab 38, 481–490 (2020). https://doi.org/10.1007/s00774-020-01090-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-020-01090-5