Abstract
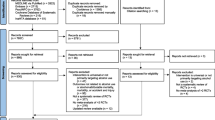
This study aims to synthesise the available evidence on psychological interventions to reduce alcohol consumption among pregnant and postpartum women. Six electronic databases were searched to identify controlled studies targeting pregnant and postpartum women who drink or are at risk of drinking due to previous patterns of alcohol use. Controlled quantitative studies such as randomised controlled trials and quasi-experimental studies were included. The search was limited to peer-reviewed articles in English. The methodological quality of studies was assessed using the Cochrane risk of bias tool. A narrative synthesis of the findings was conducted. In total, 12,610 records were screened, and 11 studies were eligible for inclusion (9 with pregnant women, 2 with postpartum women). All studies were randomised controlled trials. Five studies had positive or partially positive primary outcomes of reductions in drinking or abstinence, and their interventions ranged from multi-session brief interventions to self-help manuals based on cognitive behavioural components. All studies showed considerable methodological limitations. Psychological interventions may be effective in promoting abstinence or reducing alcohol consumption among pregnant and postpartum women. Interventions that demonstrated some efficacy showed higher level of engagement with pregnant women compared to studies which delivered interventions in a single session. Paucity of evidence, inconsistency of outcomes, large heterogeneity in the interventions and methodological weaknesses limit the ability to make final conclusions about the overall effectiveness of these interventions. Findings highlight the need for better quality research on this topic.

Similar content being viewed by others
Data availability
Data and materials of this systematic review can be obtained from the corresponding author.
References
Bailey BA, Sokol RJ (2011) Prenatal alcohol exposure and miscarriage, stillbirth, preterm delivery, and sudden infant death syndrome. Alcohol Res Health 34:86–91
Bertrand J, Floyd R, Weber M et al (2004) Fetal alcohol syndrome: guidelines for referral and diagnosis. Atlanta, GA
Center for Substance Abuse Treatment (1999) Brief interventions and brief therapies for substance abuse. Substance Abuse and Mental Health Services Administration (US), Rockville, MD
Chang G, McNamara TK, Orav EJ et al (2005) Brief intervention for prenatal alcohol use: a randomized trial. Obstet Gynecol 105:991–998
Chang G, Wilkins-Haug L, Berman S, Goetz MA (1999) Brief intervention for alcohol use in pregnancy: a randomized trial. Addiction 94:1499–1508
Choi KW, Abler LA, Watt MH, Eaton LA, Kalichman SC, Skinner D, Pieterse D, Sikkema KJ (2014) Drinking before and after pregnancy recognition among South African women: the moderating role of traumatic experiences. BMC Pregnancy Childbirth 14:97. https://doi.org/10.1186/1471-2393-14-97
Ernhart CB, Morrow-Tlucak M, Sokol RJ, Martier S (1988) Underreporting of alcohol use in pregnancy. Alcohol Clin Exp Res 12:506–511. https://doi.org/10.1111/j.1530-0277.1988.tb00233.x
Fergie L, Campbell KA, Coleman-Haynes T, Ussher M, Cooper S, Coleman T (2018) Identifying effective behavior change techniques for alcohol and illicit substance use during pregnancy: a systematic review. Ann Behav Med 53:769–781. https://doi.org/10.1093/abm/kay085
Fleming MF, Lund MR, Wilton G, Landry M, Scheets D (2008) The Healthy Moms Study: the efficacy of brief alcohol intervention in postpartum women. Alcohol Clin Exp Res 32:1600–1606
Gebara CF d P, Bhona FM d C, Ronzani TM et al (2013) Brief intervention and decrease of alcohol consumption among women: a systematic review. Subst Abuse Treat Prev Policy 8:31. https://doi.org/10.1186/1747-597X-8-31
Gilinsky A, Swanson V, Power K (2011) Interventions delivered during antenatal care to reduce alcohol consumption during pregnancy: a systematic review. Addict Res Theory 19:235–250. https://doi.org/10.3109/16066359.2010.507894
Handmaker NS, Miller WR, Manicke M (1999) Findings of a pilot study of motivational interviewing with pregnant drinkers. J Stud Alcohol 60:285–287
Henderson J, Gray R, Brocklehurst P (2007) Systematic review of effects of low–moderate prenatal alcohol exposure on pregnancy outcome. BJOG An Int J Obstet Gynaecol 114:243–252. https://doi.org/10.1111/j.1471-0528.2006.01163.x
Institute of Medicine; Committee to Study Fetal Alcohol Syndrome (1996) Fetal alcohol syndrome: diagnosis, epidemiology, prevention, and treatment, 1st edn. National Academies Press, Washington, D.C.
Kaner EFS, Beyer FR, Muirhead C, Campbell F, Pienaar ED, Bertholet N, Daeppen JB, Saunders JB, Burnand B, Cochrane Drugs and Alcohol Group (2018) Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004148.pub4
Lange S, Shield K, Koren G, Rehm J, Popova S (2014) A comparison of the prevalence of prenatal alcohol exposure obtained via maternal self-reports versus meconium testing: a systematic literature review and meta-analysis. BMC Pregnancy Childbirth 14:127. https://doi.org/10.1186/1471-2393-14-127
Mamluk L, Edwards HB, Savović J, Leach V, Jones T, Moore THM, Ijaz S, Lewis SJ, Donovan JL, Lawlor D, Smith GD, Fraser A, Zuccolo L (2017) Low alcohol consumption and pregnancy and childhood outcomes: time to change guidelines indicating apparently ‘safe’ levels of alcohol during pregnancy? A systematic review and meta-analyses. BMJ Open 7:e015410. https://doi.org/10.1136/bmjopen-2016-015410
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
NICE (2014) Antenatal and postnatal mental health: clinical management and service clinical management and service guidance
O’connor MJ, Whaley SE (2007) Brief intervention for alcohol use by pregnant women. Am J Public Health 97:252–258
Ondersma SJ, Beatty JR, Svikis DS, Strickler RC, Tzilos GK, Chang G, Divine GW, Taylor AR, Sokol RJ (2015) Computer-delivered screening and brief intervention for alcohol use in pregnancy: a pilot randomized trial. Alcohol Clin Exp Res 39:1219–1226
Ondersma SJ, Svikis DS, Thacker LR, Beatty JR, Lockhart N (2016) A randomised trial of a computer-delivered screening and brief intervention for postpartum alcohol use. Drug Alcohol Rev 35:710–718
Oni HT, Buultjens M, Abdel-Latif ME, Islam MM (2018) Barriers to screening pregnant women for alcohol or other drugs: a narrative synthesis. Women and Birth 32:479–486. https://doi.org/10.1016/j.wombi.2018.11.009
Patra J, Bakker R, Irving H, Jaddoe VWV, Malini S, Rehm J (2011) Dose–response relationship between alcohol consumption before and during pregnancy and the risks of low birthweight, preterm birth and small for gestational age (SGA)—a systematic review and meta-analyses. BJOG An Int J Obstet Gynaecol 118:1411–1421. https://doi.org/10.1111/j.1471-0528.2011.03050.x
Popay J, Roberts H, Sowden A et al (2006) Guidance on the conduct of narrative synthesis in systematic reviews. ESRC Methods Program 1:b92
Popova S, Lange S, Probst C, Gmel G, Rehm J (2017) Estimation of national, regional, and global prevalence of alcohol use during pregnancy and fetal alcohol syndrome: a systematic review and meta-analysis. Lancet Glob Heal 5:e290–e299. https://doi.org/10.1016/S2214-109X(17)30021-9
Reynolds KD, Coombs DW, Lowe JB, Peterson PL, Gayoso E (1995) Evaluation of a self-help program to reduce alcohol consumption among pregnant women. Int J Addict 30:427–443
Romano M, Cacciatore A, Giordano R, La Rosa B (2010) Postpartum period: three distinct but continuous phases. J Prenat Med 4:22–25
Royal College of Obstetricians and Gynaecologists (2018) Alcohol and pregnancy
Rubio DM, Day NL, Conigliaro J et al (2014) Brief motivational enhancement intervention to prevent or reduce postpartum alcohol use: a single-blinded, randomized controlled effectiveness trial. J Subst Abus Treat 46:382–389
Sokol RJ, Martier SS, Ager JW (1989) The T-ACE questions: practical prenatal detection of risk-drinking. Am J Obstet Gynecol 160:863–870. https://doi.org/10.1016/0002-9378(89)90302-5
Stade BC, Bailey C, Dzendoletas D, Sgro M, Dowswell T, Bennett D, Cochrane Pregnancy and Childbirth Group (2009) Psychological and/or educational interventions for reducing alcohol consumption in pregnant women and women planning pregnancy. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004228.pub2
Sterne JAC, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JPT (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
Sterne JAC, Savović J, Page MJ, et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:. https://doi.org/10.1136/bmj.l4898
Tzilos GK, Sokol RJ, Ondersma SJ (2011) A randomized phase I trial of a brief computer-delivered intervention for alcohol use during pregnancy. J Women’s Heal 20:1517–1524
van der Wulp NY, Hoving C, Eijmael K, Candel MJJM, van Dalen W, de Vries H (2014) Reducing alcohol use during pregnancy via health counseling by midwives and internet-based computer-tailored feedback: a cluster randomized trial. J Med Internet Res 16:e274
WHO (2014) Guidelines for the identification and management of substance use and substance use disorders in pregnancy. World Health Organization, Geneva
WHO (2003) Global strategy for infant and young child feeding. World Health Organization, Geneva
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the London School of Hygiene and Tropical Medicine.
Consent to participate
NA
Consent for publication
NA
Code availability
NA
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 52 kb)
Rights and permissions
About this article
Cite this article
Samawi, L., Williams, P.P., Myers, B. et al. Effectiveness of psychological interventions to reduce alcohol consumption among pregnant and postpartum women: a systematic review. Arch Womens Ment Health 24, 557–568 (2021). https://doi.org/10.1007/s00737-020-01100-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-020-01100-5