Abstract
Non-motor symptoms (NMS) occur in patients with cervical dystonia (CD) but with variable frequencies and impact on health-related quality of life (HRQoL). To define non-motor and motor profiles and their respective impact on HRQoL in CD patients using the newly validated Dystonia Non-Motor Symptoms Questionnaire (DNMSQuest). In an observational prospective multicentre case–control study, we enrolled 61 patients with CD and 61 age- and sex-matched healthy controls (HC) comparing demographic data, motor and non-motor symptoms and HRQoL measurements. 95% CD patients reported at least one NMS. Mean total NMS score was significantly higher in CD patients (5.62 ± 3.33) than in HC (1.74 ± 1.52; p < 0.001). Pain, insomnia and stigma were the most prevalent NMS and HRQoL was significantly impaired in CD patients compared to HC. There was strong correlation of NMS burden with HRQoL (CDQ-24: r = 0.72, EQ-5D: r = − 0.59; p < 0.001) in CD patients. Regression analysis between HRQoL and NMS suggested that emotional well-being (standardized beta = − 0.352) and pain (standardized beta = − 0.291) had a major impact on HRQoL while, in contrast motor severity had no significant impact in this model. Most NMS with the exception of pain, stigma and ADL did not correlate with motor severity. NMS are highly prevalent in CD patients and occur independent of age, sex, disease duration, duration of botulinum neurotoxin therapy and socio-economic status. Specific NMS such as emotional well-being and pain have a major impact on HRQoL and are more relevant than motor severity.
Similar content being viewed by others
Introduction
Cervical dystonia (CD) is the commonest idiopathic focal dystonia (Albanese et al. 2013; LeDoux et al. 2016) and is one of the most frequently treated movement disorders (Defazio et al. 2013b; Group 2000). Non-motor symptoms (NMS) are common in CD and can range from pain perception, sleep dysfunction to neuropsychiatric symptoms such as depression and are considered as a research priority (Jinnah et al. 2013). However, the results from these studies vary in relation to the reported frequencies of various NMS and in their impact on health-related quality of life (HRQoL). One explanation for the reported variabilities could be related to diverse and non-standard methodologies of assessment of NMS. The Dystonia Non-Motor Symptoms Questionnaire (DNMSQuest (Klingelhoefer et al. 2019, 2020)) is a newly described 14-item self-completed questionnaire listing the presence of a range of NMS in patients with craniocervical dystonia during the past month. The overall load of the seven different relevant non-motor domains of the DNMSQuest can be calculated as an estimation of the symptoms burden [similar to NMS questionnaire for Parkinson’s disease (PD) (Chaudhuri et al. 2006)] (Klingelhoefer et al. 2019).
In this case–control study we report on the association and the impact of non-motor burden and motor symptoms on HRQoL in CD patients using the DNMSQuest.
Methods
Patients and healthy controls (HC)
Consecutive patients with a diagnosis of adult-onset idiopathic CD according to the definition by Albanese et al. (2013) were included in this study. To minimize the potential effect of botulinum neurotoxin (BoNT) therapy on CD and study assessments, subjects were included at the end of a BoNT therapy cycle (≥ 3 months after the last BoNT treatment). Age- and sex-matched HC were selected from unrelated companions and carers.
Inclusion and exclusion criteria
All patients with CD and HC were included after exclusion of alternative movement disorders other than idiopathic dystonia and associated tremor. Patients with other forms of dystonia, with dementia or significant cognitive impairment [< 22 points on Montreal Cognitive Assessment (MoCA) (Dalrymple-Alford et al. 2010; Freitas et al. 2013)] and those undergoing deep brain stimulation were excluded.
Recruitment centres
Patients were recruited from two different specialist Movement Disorders Clinics in Germany: Department of Neurology, Technical University Dresden and Department of Neurology, Klinikum Chemnitz. HC were recruited at the Department of Neurology, Technical University Dresden, Germany and at the Parkinson’s Centre and Movement Disorders Clinic, King’s College London, UK. The project fell under the auspices of the Dresden-King’s-TransCampus research initiative.
Study assessments
The study protocol was approved by the ethics committee of the participant institutions (Dresden/Chemnitz: EK60022015, King’s College London: 15/EM/0106). All participants provided written informed consent before any study procedure was performed. The following variables were collected:
-
Demographic and disease-specific variables, general medical history, medication and BoNT dosage (calculated in Dysport mouse units).
-
Motor assessment: Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS) (Consky et al. 1990). Unified Dystonia Rating Scale (UDRS) (Comella et al. 2003), which includes ratings for 14 body areas of motor severity and duration of dystonia with a total score of 112. As only patients with focal CD affecting the neck and shoulder/proximal arm domain have been included, the maximal total score was 24.
-
Clinical Global Impression of severity (CGI-S) (Guy 1976) to assess severity of CD.
-
Non-motor assessment: Dystonia Non-Motor Symptoms Questionnaire (DNMSQuest) with seven different domains: sleep, autonomic symptoms, fatigue, emotional well-being, stigma, ADL, sensory symptoms [described in Klingelhoefer et al. (2019, 2020)]; additionally a question on memory and concentration, each formulated in the same style as the DNMSQuest and referred to as cognition domain of the DNMSQuest were added; MoCA (Nasreddine et al. 2005); Beck Depression Inventory (BDI) (Beck et al. 1996).
-
Quality of life questionnaires: Craniocervical dystonia questionnaire (CDQ-24) (Muller et al. 2004); EuroQol five dimensions questionnaire (EQ-5D) with index and visual analogue scale (VAS) (Group 1990).
Statistics
As data were not normally distributed, non-parametric statistics were applied, e.g. Mann–Whitney U Test. Analyses were performed with Chi-Square-Test and with Spearman rank correlation coefficient (r). The correlation was considered: “weak” if the r value was < 0.3, “moderate” if 0.3–0.5, “high” if > 0.5. A p value of less than 0.05 indicated statistical significance. Based on the approach of van den Dool et al. (2016) a principal component analysis and subsequently a multivariable linear regression analysis in backward elimination technique was also performed. Seven different symptom complexes were defined by generating congruent topics based on motor and non-motor domains of the different scales and questionnaires (TWSTRS, UDRS, CGI-S, DNMSQuest, MOCA, BDI, CDQ-24). For each symptom complex variables were transformed to normal distributions when appropriate and standardised into Z scores to enable direct comparison. Reliability analyses were performed to control the internal consistency of the variables within each symptom complex. A Cronbach’s alpha of ≥ 0.7 was evaluated as acceptable (Cronbach 1951).
Results
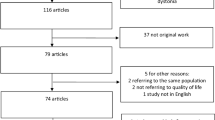
61 patients with CD and 61 HC were studied. Demographics, socio-economic status, general medical and family history are summarized in Table 1. Disease-specific characteristics of CD patients and therapy are summarized in Table 2. There was no missing data in the included study participants. Five HC and four CD patients were excluded due to neurological co-morbidities, MOCA < 22 points, segmental or multifocal dystonia.
Motor symptoms
CD patients had a mean TWSTRS sum score of 34.5 ± 12.94 (range 9.5–65.5) and a mean UDRS sum score of 9.5 ± 2.81 (range 1.5–14.0). CD patients ranged from CGI score 2–7 with 77% of patients presenting with “mildly ill” (score 3) to “markedly ill” (score 5) (median ± SE 4.00 ± 0.15, minimum 2, maximum 7). In contrast, 92% of HC reported to be “normal, not at all ill” in the CGI score (median ± SE 1.00 ± 0.06, IQR 1–1, minimum 1, maximum 3). Based on the Col-Cap concept (Reichel 2013), only 6.6% of the CD patients had a malposition in one whereas 47.5% in two and 45.9% in three anatomical planes. We found no significant correlation of motor severity (assessed by TWSTRS, UDRS, CGI) with age, sex, disease duration, duration of BoNT therapy, concomitant diseases as well as operations or traumata and socio-economic status in the investigated CD patients (p < 0.05).
Non-motor symptoms
NMS were significantly more common in CD patients compared to HC with pain, insomnia and stigma being the most prevalent symptoms. Mean total NMS score was significantly higher in CD patients (5.62 ± 3.33; range 0–14) in comparison to HC (1.74 ± 1.52; range 0–6) (p < 0.001). 95.1% CD patients reported at least one NMS and therefore only 4.9% did not suffer from any of the assessed NMS. About 29.5% CD patients presented with at least eight NMS. Additionally, all DNMSQuest domains were significantly more prevalent in CD patients than in HC (Fig. 1). There was no impact of age, sex, disease duration, duration of BoNT therapy and socio-economic status on the assessed NMS by DNMSQuest in the investigated CD patients (r = − 0.14 to 0.08, p > 0.05). In contrast, we found a significant correlation of NMS burden in HC with age (r = 0.35) and concomitant diseases (r = 0.36) on a moderate level (p < 0.01).
Association of motor and non-motor symptoms
The DNMSQuest score did not correlate with the TWSTRS I and UDRS but correlated significantly on a moderate to high level with its NMS parts (TWSTRS II: r = 0.43, III: r = 0.54, p < 0.001) as did the CDQ-24 (TWSTRS II: r = 0.54, III: r = 0.51, p < 0.001).
Sensory symptoms/pain
There was a linear correlation of the sensory symptoms domain of the DNMSQuest and the pain domain of the CDQ-24 and TWSTRS. The disability score (TWSTRS II) significantly correlated with pain [corresponding domains of DNMSQuest (r = 0.27, p < 0.05) and CDQ-24 (r = 0.62, p < 0.01)]. Further, pain assessed by TWSTRS III significantly correlated on a moderate level with emotional well-being (corresponding domains of DNMSQuest and CDQ-24: r = 0.30–0.36, p < 0.05) and with BDI (r = 0.39, p < 0.05). In contrast, there were only few significant correlations on a weak to moderate level of pain domains (TWSTRS III: r = 0.28, CDQ-24: r = 0.3–0.37, p < 0.05; DNMSQuest p > 0.05) with pure motor severity assessed by TWSTRS I and UDRS. In relation to motor severity, most relevant seemed to be the duration of head deviation (TWSTRS IB, UDRS I: r = 0.26–0.39) and the duration of BoNT effectiveness as a higher duration of head deviation and a shorter time of BoNT effectiveness were associated with more pain.
Emotional well-being
CD patients reported symptoms of depression, anxiety or flat moods twice as frequently as HC (Fig. 1). The mean BDI score was 8.6 ± 6.7 (range 0–24) and revealed a mild depression in 37% of CD patients. The BDI correlated on a moderate to high level with the DNMSQuest (r = 0.51, p < 0.01), the CDQ-24 (r = 0.67, p < 0.001) and the CDQ-24 emotional well-being domain (r = 0.4, p < 0.05). There was no association of the emotional well-being domain of the DNMSQuest and of the CDQ-24 with motor severity of CD (TWSTRS I, UDRS). In contrast, the emotional well-being domain of the DNMSQuest and of the CDQ-24 correlated significantly with various NMS (e.g. stigma, ADL, sleep/fatigue, pain, cognition) on a moderate to high level (r = 0.34–0.58, p < 0.05). CD patients reported a reduced HrQoL in EQ-5D VAS associated with worse emotional well-being assessed by the DNMSQuest (p < 0.001, Fig. 2).
Worse emotional well-being in the Dystonia Non-Motor Symptoms Questionnaire (DNMSQuest) is associated with reduced health related quality of life (assessed by EuroQol five dimensions questionnaire visual analogue scale (EQ-5D VAS)) in patients with cervical dystonia. Boxes: 25 and 75 percentiles. Whiskers: minimum and maximum values
Stigma
51% of CD patients declared the feeling of stigmatisation (Fig. 1). CD patients younger than 60 years of age suffered more often from stigmatisation than those older than 60 years (60% vs. 38.5%). The general impression of the CD assessed by CGI correlated on a high level with the stigma domain of the DNMSQuest (r = 0.57, p < 0.001) and on a moderate level with the one of the CDQ-24 (r = 0.3, p < 0.05). Stigmatisation as declared in DNMSQuest was significantly associated with worse motor severity (TWSTRS I: r = 0.26, p < 0.05), general NMS burden (r = 0.56, p < 0.001) and HrQoL (EQ-5D VAS r = − 0.45, CDQ-24 r = 0.53, p < 0.001).
Sleep/fatigue
The sleep/fatigue domain of the DNMSQuest correlated on a moderate to high level with the pain (r = 0.51, p < 0.001), the ADL (r = 0.5, p < 0.001) and the emotional well-being (r = 0.44, p < 0.001) domain of the CDQ-24. Furthermore, CD patients with anxiolytic or antidepressant medication presented with significant higher values in the DNMSQuest sleep/fatigue domain.
Cognition
CD patients showed a significantly lower mean MoCA value in comparison to HC (CD: 27.8 ± 1.95, range 22-30; HC: 28.5 ± 1.41, range 25–30; p < 0.05). In any of the single MoCA domains, CD patients were slightly worse but without significant difference to HC. Additionally, significantly more CD patients than HC declared impaired cognition and attention in the cognition domain of the DNMSQuest (41% vs. 21%). The cognition domain of the DNMSQuest significantly correlated with the emotional well-being (r = 0.34, p < 0.01) and the ADL (r = 0.42, p < 0.001) domain of the CDQ-24 as well as with the cognition domain (r = − 0.36, p < 0.01) of the MoCA.
Activities of daily living
With increasing limitations in ADL as assessed by the DNMSQuest, CD patients reported reduced HRQoL (CDQ-24, CDQ-24 ADL domain, p < 0.001), higher disability (TWSTRS II, p < 0.001) and had worse motor symptoms (TWSTRS I, UDRS, p < 0.01).
Health-related quality of life
CD patients presented with a significantly reduced HRQoL compared to HC (EQ-5D index: CD 0.86 ± 0.18, HC 0.95 ± 0.06, p < 0.001; EQ-5D VAS: CD 64.2 ± 20.21, HC 73.8 ± 13.31, p < 0.05; CDQ-24: CD 29.11 ± 17.48). Both, the EQ-5D index and VAS correlated significantly on a high level with pure NMS assessment by DNMSQuest (index r = − 0.58, VAS: r = − 0.59, p < 0.001) (Fig. 3a). Further, all domains of the DNMSQuest, despite the cognition domain, correlated significantly with EQ-5D index and VAS (r = − 0.26 to − 0.56, p < 0.05). Interestingly, only the EQ-5D VAS correlated significantly on a moderate level with pure motor assessments (TWSTRS I: r = − 0.43, UDRS: r = − 0.31; p < 0.01) but not the EQ-5D index (Fig. 3b). Additionally, DNMSQuest total score correlated significantly on a high level with the CDQ-24 total score and its domains (r = 0.51–0.72, p < 0.001, except social/family life: r = 0.32, p < 0.05) (Fig. 3c). Also, TWSTRS I correlated significantly with CDQ-24 but on a moderate level (r = 0.38, p < 0.01, Fig. 3d).
Scatterplots with negative regression lines for relationship between non-motor symptoms assessed by Dystonia Non-Motor Symptoms Questionnaire (DNMSQuest; a, c) and motor symptoms assessed by TWSTRS I (b, d) with health related quality of life measures in patients with cervical dystonia. EQ-5D VAS EuroQol five dimensions questionnaire visual analogue scale, CDQ-24 craniocervical dystonia questionnaire
To evaluate the impact of the defined symptom complexes on HRQoL, multiple regression analysis was used with EQ-5D VAS as dependent variable (Table 3). All symptom complexes revealed an acceptable Cronbach’s alpha. The model revealed significance [adjusted R2 0.573, F (4–55) = 20.81, p < 0.001] and 57% of the variance of HRQoL assessed by EQ-5D VAS could be explained. Major impact on HRQoL had the symptom complexes emotional well-being followed by pain. Stigma and motor severity showed an impact but were not significant in this model.
Discussion
In this multicenter observational case–control study, we describe the non-motor and motor profiles as well as their impact on HRQoL in CD patients in comparison to age- and sex-matched HC using the newly validated DNMSQuest.
The majority of investigated CD patients has intermediate motor severity, a combination of different dystonic postures and dystonic head tremor as previously described (Chan et al. 1991; Defazio et al. 2013a; Jankovic et al. 1991; Jost et al. 2020; Tomic et al. 2016; van den Dool et al. 2016; Werle et al. 2014). Importantly, our study cohort consisted of mainly middle-aged females and thus is representative for the CD population (Defazio et al. 2013b; Group 2000). Furthermore, patients of all disease durations and in all CGI stages were included.
NMS were significantly more common in CD patients with 95% reporting at least one NMS; in line with other publications (Klingelhoefer et al. 2014; Smit et al. 2017a). While in HC the NMS burden only became relevant with increasing age and comorbidities, in CD patients, the investigated NMS were independent of age, sex, disease duration, duration of BoNT therapy and socio-economic status. Further, there was no association of general NMS burden and motor severity.
Pain is common in dystonia (57–89% of CD patients), mainly in the neck and shoulder area (Comella and Bhatia 2015; Klingelhoefer et al. 2019; Sheehy and Marsden 1980; Tinazzi et al. 2020; Werle et al. 2014). In our study pain was reported by 77% of CD patients and there was a strong correlation between pain and other NMS, especially emotional well-being and depression whereas the correlation between pain and motor severity was low. This observation is therefore of interest as we also report that pain is only partly related to motor severity with the duration of head deviation being the most relevant factor. Our overall results support observations in relation to lack of correlation between pain and motor severity (Kutvonen et al. 1997; Novaretti et al. 2019). Emotional well-being, comprising symptoms of depression and anxiety, was highly prevalent and reported by 59% of CD patients in DNMSQuest; in line with other observations (Comella and Bhatia 2015; Fabbrini et al. 2010; Smit et al. 2016). Even though 37% of CD patients fulfilled the DSM criteria of mild depression (Beck et al. 1996; Kühner et al. 2007) only half of the CD patients had a documented diagnosis of depression/anxiety disorder and only a quarter was treated with anxiolytics or antidepressants. Our results indicate a marked underreporting of psychiatric comorbidities in CD patients. This is of special interest as our study and other publications reported no association of emotional well-being and motor severity (Gundel et al. 2001; Skogseid et al. 2007; Slawek et al. 2007) emphasising the need of recognition and appropriate treatment of NMS. Perceived Stigma was prevalent in around half of the investigated CD patients, especially in younger adults. Stigmatisation was mainly related to worse motor severity but also to a higher NMS burden. In our study, CD patients reporting stigmatisation were more likely to present with depressive symptoms and be treated with antidepressants or anxiolytics as described previously (Lewis et al. 2008; Papathanasiou et al. 2001). Sleep dysfunction was the second most common NMS with various presentation (66% of CD patients reporting insomnia, 41% a feeling of impaired sleep quality, 49% daytime sleepiness/fatigue). These findings are in line with other studies reporting impaired sleep in 44–72% of CD patients (Avanzino et al. 2010; Klingelhoefer et al. 2014; Paus et al. 2011). Sleep impairment was associated with reduced emotional well-being and more often reported by CD patients treated with anxiolytics or antidepressants. Importantly, sleep problems were not related to motor severity. Furthermore, our study revealed for the first time that CD patients with sleep problems had a higher pain burden than those with regular sleep and pain symptoms were reported more often during the day. Overall, sleep dysfunction and pain seem to aggravate each other independent of motor severity of CD and point out the need of specific treatment.
CD patients were significantly more impaired in their ADLs than HC. Relevant influencing factors on ADL were mainly other NMS like pain, emotional well-being, sleep dysfunction and autonomic symptoms but also motor severity. Van den Dool et al. (2016) showed that psychiatric features and pain have the largest contribution to disability in CD patients. We confirm these findings with more than half of our CD patients reporting pain as a source of disability.
NMS have a relevant influence on HRQoL in movement disorders, especially in PD (Martinez-Martin et al. 2011). In dystonia, NMS and their impact on HRQoL is topical (Ben-Shlomo et al. 2002; Camfield et al. 2002; Paracka et al. 2020; Pekmezovic et al. 2009; Smit et al. 2017b). The present study reports the impact of NMS burden, assessed by DNMSQuest, on HRQoL in CD patients (Fig. 3). HRQoL was measured by CDQ-24, a specific validated self-reported questionnaire for the assessment of HRQoL in craniocervical dystonia (Fig. 3c) and by EQ-5D, a more general validated self-reported questionnaire for the assessment of HRQoL in any kind of disease (Fig. 3a).
Based on the defined symptom complexes, emotional well-being had the highest impact on HRQoL followed by pain. Emotional well-being was also found relevant for HRQoL in CD patients in other studies (Ben-Shlomo et al. 2002; Drexel et al. 2020; Muller et al. 2002; Skogseid et al. 2007; Slawek et al. 2007). Pain as the second most relevant factor for HRQoL in the investigated CD patients, explained 41% of reduced HRQoL in a study by Werle et al. (2014). Stigma and motor severity were closely linked and relevant for HRQoL but were not significant in this study. Stigma was reported as the most relevant factor for HRQoL when using the CDQ-24 (Muller et al. 2004; van den Dool et al. 2016). This is in line with the finding of Drexel et al. reporting reduced HRQoL even under BoNT treatment (Drexel et al. 2020). Further NMS such as sleep problems and impaired ADL were associated with reduced HRQoL in this and previous studies (Smit et al. 2016, 2017b; Soeder et al. 2009; Tomic et al. 2016; Wagle Shukla et al. 2016) but were not significant within our regression model.
The potential limitations of this study are
-
1.
The symptom complex “sleep/fatigue” covers the sleep and fatigue domain of the DNMSQuest even though fatigue is not a sleep-related problem. There are no disease-specific sleep/fatigue scales in dystonia but “sleep/fatigue” are clustered together in other NMS measures, e.g. the Non-Motor Symptom assessment scale for PD (Chaudhuri et al. 2007). Thus we used the combined symptom complex in our analysis.
-
2.
The symptom complex “cognition” should be evaluated with caution as participants with a history of dementia or evidence of significant cognitive impairment were excluded. Nevertheless, the greater impairment of cognition and attention in CD patients compared to HC, both in subjective and objective evaluation, is an interesting finding, supported by other investigations (Czekoova et al. 2017) and needs further investigation.
-
3.
The effect of BoNT therapy cannot be evaluated as study assessments were performed at the end of a BoNT treatment cycle (Table 2). However, we observed that a shorter positive BoNT effect is associated with a higher amount of NMS and a longer positive BoNT effect is associated with better HRQoL. This may provide a hint that BoNT has a positive effect on NMS, at least on those NMS secondary to motor symptoms. These observations need to be studied further, e.g. by re-assessment of NMS at the most effective time point after BoNT treatment. An assessment of de-novo patients would also be desirable to fully exclude any BoNT effects.
In summary, we report that NMS are highly prevalent in CD patients with 95% reporting at least one NMS. Pain, sleep problems, stigma, anxiety and depression being most common NMS. Furthermore, NMS are present throughout the whole course of dystonia and appear independent of age, sex, disease duration, duration of BoNT therapy and socio-economic status. In general, NMS burden and especially emotional well-being and pain have a major impact on HRQoL which may be a greater determinant of QoL compared to the motor symptoms in CD patients. Further, most NMS with the exception of pain, stigma and ADL occurred independent of motor severity of CD. Therefore, in line with previous publications, our data suggests that most NMS could be a primary phenomenon of dystonia. This is of major importance as a diagnostic consideration and for a holistic treatment approach of CD patients. In contrast to the diagnostic criteria for PD including NMS both as supportive and as exclusion criteria (Postuma et al. 2015), the current definition of dystonia does not consider any NMS (Albanese et al. 2013). The DNMSQuest therefore, could be an useful screening tool empowering CD patients to declare relevant NMS and thus personalise and improve holistic care.
References
Albanese A et al (2013) Phenomenology and classification of dystonia: a consensus update. Mov Disord 28:863–873. https://doi.org/10.1002/mds.25475
Avanzino L et al (2010) Quality of sleep in primary focal dystonia: a case-control study. Eur J Neurol 17:576–581. https://doi.org/10.1111/j.1468-1331.2009.02884.x
Beck AT, Steer RA, Brown GK (1996) Manual for the Beck depression inventory-II. Psychological Corporation, San Antonio
Ben-Shlomo Y, Camfield L, Warner T (2002) What are the determinants of quality of life in people with cervical dystonia? J Neurol Neurosurg Psychiatry 72:608–614
Camfield L, Ben-Shlomo Y, Warner TT (2002) Impact of cervical dystonia on quality of life. Mov Disord 17:838–841. https://doi.org/10.1002/mds.10127
Chan J, Brin MF, Fahn S (1991) Idiopathic cervical dystonia: clinical characteristics. Mov Disord 6:119–126. https://doi.org/10.1002/mds.870060206
Chaudhuri KR et al (2006) International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: the NMSQuest study. Mov Disord 21:916–923. https://doi.org/10.1002/mds.20844
Chaudhuri KR et al (2007) The metric properties of a novel non-motor symptoms scale for Parkinson’s disease: results from an international pilot study. Mov Disord 22:1901–1911. https://doi.org/10.1002/mds.21596
Comella C, Bhatia K (2015) An international survey of patients with cervical dystonia. J Neurol 262:837–848. https://doi.org/10.1007/s00415-014-7586-2
Comella CL, Leurgans S, Wuu J, Stebbins GT, Chmura T (2003) Rating scales for dystonia: a multicenter assessment. Mov Disord 18:303–312. https://doi.org/10.1002/mds.10377
Consky E, Basinski A, Belle L, Ranawaya R, Lang A (1990) Toronto western spasmodic torticollis rating scale (TWSTRS): assesment of validity and inter- rater reliability. Neurology 40(suppl):445
Cronbach LJ (1951) Coefficient alpha and the internal structure of tests. Psychometrika 16:297–334
Czekoova K, Zemankova P, Shaw DJ, Bares M (2017) Social cognition and idiopathic isolated cervical dystonia. J Neural Transm (Vienna) 124:1097–1104. https://doi.org/10.1007/s00702-017-1725-8
Dalrymple-Alford JC et al (2010) The MoCA: well-suited screen for cognitive impairment in Parkinson disease. Neurology 75:1717–1725. https://doi.org/10.1212/WNL.0b013e3181fc29c9
Defazio G et al (2013a) Tremor in primary adult-onset dystonia: prevalence and associated clinical features. J Neurol Neurosurg Psychiatry 84:404–408. https://doi.org/10.1136/jnnp-2012-303782
Defazio G, Jankovic J, Giel JL, Papapetropoulos S (2013b) Descriptive epidemiology of cervical dystonia. Tremor Other Hyperkinet Mov (N Y). https://doi.org/10.7916/d80c4tgj
Drexel SC et al (2020) Caregiver burden and health-related quality of life in idiopathic dystonia patients under botulinum toxin treatment: a cross-sectional study. J Neural Transm (Vienna) 127:61–70. https://doi.org/10.1007/s00702-019-02109-6
Fabbrini G et al (2010) Psychiatric disorders in adult-onset focal dystonia: a case-control study. Mov Disord 25:459–465. https://doi.org/10.1002/mds.22983
Freitas S, Simoes MR, Alves L, Santana I (2013) Montreal cognitive assessment: validation study for mild cognitive impairment and Alzheimer disease. Alzheimer Dis Assoc Disord 27:37–43. https://doi.org/10.1097/WAD.0b013e3182420bfe
Group ESoDiEEC (2000) A prevalence study of primary dystonia in eight European countries. J Neurol 247:787–792
Group TE (1990) EuroQol—a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Gundel H, Wolf A, Xidara V, Busch R, Ceballos-Baumann AO (2001) Social phobia in spasmodic torticollis. J Neurol Neurosurg Psychiatry 71:499–504
Guy W (1976) Clinical Global Impressions (028-CGI). ECDEU Assessment Manual for Psychopharmacology. In: US Department of Health EaW, Public Health Service Alcohol, Drug Abuse, and Mental Health Administration, Rockville pp 217–222
Jankovic J, Leder S, Warner D, Schwartz K (1991) Cervical dystonia: clinical findings and associated movement disorders. Neurology 41:1088–1091. https://doi.org/10.1212/wnl.41.7.1088
Jinnah HA et al (2013) The focal dystonias: current views and challenges for future research. Mov Disord 28:926–943. https://doi.org/10.1002/mds.25567
Jost WH et al (2020) Frequency of different subtypes of cervical dystonia: a prospective multicenter study according to Col-Cap concept. J Neural Transm (Vienna) 127:45–50. https://doi.org/10.1007/s00702-019-02116-7
Klingelhoefer L et al (2014) Nonmotor symptoms and focal cervical dystonia: observations from 102 patients. Basal Ganglia 4:117–120
Klingelhoefer L et al (2019) Validation of a self-completed Dystonia Non-Motor Symptoms Questionnaire. Ann Clin Transl Neurol 6:2054–2065. https://doi.org/10.1002/acn3.50900
Klingelhoefer L, Jost W, Odin P, Storch A, Ray Chaudhuri K, Reichmann H (2020) [Dystonia Non-Motor Symptoms Questionnaire (DNMSQuest) for assessment of non-motor symptoms in dystonia: intercultural adaptation in the German language]. Nervenarzt 91:337–342. https://doi.org/10.1007/s00115-020-00885-1
Kühner C, Bürger C, Keller F, Hautzinger M (2007) Reliabilität und Validität des revidierten Beck-Depressions-Inventars (BDI-II). Befunde aus deutschsprachigen Stichproben Nervenarzt, pp 651–656
Kutvonen O, Dastidar P, Nurmikko T (1997) Pain in spasmodic torticollis. Pain 69:279–286
LeDoux MS et al (2016) Clinical and genetic features of cervical dystonia in a large multicenter cohort. Neurol Genet 2:e69. https://doi.org/10.1212/NXG.0000000000000069
Lewis L, Butler A, Jahanshahi M (2008) Depression in focal, segmental and generalized dystonia. J Neurol 255:1750–1755. https://doi.org/10.1007/s00415-008-0020-x
Martinez-Martin P, Rodriguez-Blazquez C, Kurtis MM, Chaudhuri KR (2011) The impact of non-motor symptoms on health-related quality of life of patients with Parkinson’s disease. Mov Disord 26:399–406. https://doi.org/10.1002/mds.23462
Muller J et al (2002) The impact of blepharospasm and cervical dystonia on health-related quality of life and depression. J Neurol 249:842–846. https://doi.org/10.1007/s00415-002-0733-1
Muller J et al (2004) Craniocervical dystonia questionnaire (CDQ-24): development and validation of a disease-specific quality of life instrument. J Neurol Neurosurg Psychiatry 75:749–753
Nasreddine ZS et al (2005) The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriat Soc 53:695–699. https://doi.org/10.1111/j.1532-5415.2005.53221.x
Novaretti N et al (2019) The prevalence and correlation of non-motor symptoms in adult patients with idiopathic focal or segmental dystonia tremor other. Hyperkinet Mov (N Y) 9:596. https://doi.org/10.7916/fhnv-v355
Papathanasiou I, MacDonald L, Whurr R, Jahanshahi M (2001) Perceived stigma in spasmodic torticollis. Mov Disord 16:280–285
Paracka L et al (2020) Body concept and quality of life in patients with idiopathic dystonia. Brain Sci. https://doi.org/10.3390/brainsci10080488
Paus S et al (2011) Impaired sleep quality and restless legs syndrome in idiopathic focal dystonia: a controlled study. J Neurol 258:1835–1840. https://doi.org/10.1007/s00415-011-6029-6
Pekmezovic T, Svetel M, Ivanovic N, Dragasevic N, Petrovic I, Tepavcevic DK, Kostic VS (2009) Quality of life in patients with focal dystonia. Clin Neurol Neurosurg 111:161–164. https://doi.org/10.1016/j.clineuro.2008.09.023
Postuma RB et al (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30:1591–1601. https://doi.org/10.1002/mds.26424
Reichel G (2013) Therapieleitfaden Spastik-Dystonien, 5th edn. UNI-MED, Bremen
Sheehy MP, Marsden CD (1980) Trauma and pain in spasmodic torticollis. Lancet 1:777–778. https://doi.org/10.1016/s0140-6736(80)91281-7
Skogseid IM, Malt UF, Roislien J, Kerty E (2007) Determinants and status of quality of life after long-term botulinum toxin therapy for cervical dystonia. Eur J Neurol 14:1129–1137. https://doi.org/10.1111/j.1468-1331.2007.01922.x
Slawek J et al (2007) Factors affecting the health-related quality of life of patients with cervical dystonia and the impact of botulinum toxin type A injections. Funct Neurol 22:95–100
Smit M et al (2016) Psychiatric co-morbidity is highly prevalent in idiopathic cervical dystonia and significantly influences health-related quality of life: Results of a controlled study. Parkinsonism Relat Disord 30:7–12. https://doi.org/10.1016/j.parkreldis.2016.06.004
Smit M, Bartels AL, Kuiper A, Kamphuis ASJ, Han V, Tijssen MAJ (2017a) The frequency and self-perceived impact on daily life of motor and non-motor symptoms in cervical dystonia. Mov Disord Clin Pract 4:750–754. https://doi.org/10.1002/mdc3.12510
Smit M, Kamphuis ASJ, Bartels AL, Han V, Stewart RE, Zijdewind I, Tijssen MA (2017b) Fatigue, sleep disturbances, and their influence on quality of life in cervical dystonia patients. Mov Disord Clin Pract 4:517–523. https://doi.org/10.1002/mdc3.12459
Soeder A et al (2009) Mood and energy determinants of quality of life in dystonia. J Neurol 256:996–1001. https://doi.org/10.1007/s00415-009-5060-3
Tinazzi M et al (2020) Demographic and clinical determinants of neck pain in idiopathic cervical dystonia. J Neural Transm (Vienna). https://doi.org/10.1007/s00702-020-02245-4
Tomic S, Petkovic I, Pucic T, Resan B, Juric S, Rotim T (2016) Cervical dystonia and quality of life. Acta Neurol Belg 116:589–592. https://doi.org/10.1007/s13760-016-0634-1
van den Dool J, Tijssen MA, Koelman JH, Engelbert RH, Visser B (2016) Determinants of disability in cervical dystonia. Parkinsonism Relat Disord 32:48–53. https://doi.org/10.1016/j.parkreldis.2016.08.014
Wagle Shukla A et al (2016) High rates of fatigue and sleep disturbances in dystonia. Int J Neurosci 126:928–935. https://doi.org/10.3109/00207454.2015.1085035
Werle RW, Takeda SY, Zonta MB, Guimaraes AT, Teive HA (2014) The physical, social and emotional aspects are the most affected in the quality of life of the patients with cervical dystonia. Arq Neuropsiquiatr 72:405–410. https://doi.org/10.1590/0004-282x20140044
Acknowledgements
We would like to acknowledge and thank Lynsey J. Hall, Lauren Perkins and Dhaval Trivedi and London South Central Research Network (National Institute of Health Research UK) for data collection at King’s College Hospital London, support from the steering group of the original dystonia NMS project steering group, as well as all study participants for their contribution. We also thank the Dresden-King’s-TransCampus research initiative programme.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
LK: Research project: Conception, Organization, Execution, Statistical Analysis: Design, Execution, Review and Critique, Manuscript: Writing of the first draft, Review and Critique. MK: Research project: Organization, Execution, Statistical Analysis: Design, Execution, Review and Critique, Manuscript: Review and Critique. AS: Research project: Organization, Execution, Statistical Analysis: Review and Critique, Manuscript: Review and Critique. RU: Research project: Organization, Execution, Statistical Analysis: Review and Critique, Manuscript: Review and Critique. MW: Research project: Execution, Statistical Analysis: Review and Critique, Manuscript: Review and Critique. KM: Research project: Execution, Statistical Analysis: Review and Critique, Manuscript: Review and Critique. BF: Research project: Organization, Statistical Analysis: Design, Execution, Review and Critique, Manuscript: Review and Critique. OG: Research project: Organization, Execution, Statistical Analysis: Review and Critique, Manuscript: Review and Critique. KRC: Research project: Organization, Execution, Statistical Analysis: Design, Execution, Review and Critique, Manuscript: Review and Critique. HR: Research project: Organization, Execution, Statistical Analysis: Design, Execution, Review and Critique, Manuscript: Review and Critique.
Corresponding author
Ethics declarations
Conflict of interest
Information concerning all sources of financial support and funding, regardless of relationship to current manuscript: Lisa Klingelhoefer: reports academic grants from EU Horizon 2020 and habilitation funding for women from the Medical Faculty of the Technical University Dresden, Germany. Robert Untucht: reports a grant from the Stiftung Hochschulmedizin (medical university foundation) Dresden and travel costs to a conference by Merz Pharma (Frankfurt, Germany). Björn Falkenburger: received payment for consultations, talks or articles from Desitin, UCB, Thieme; research support from Deutsche Forschungsgemeinschaft and Merz. K. Ray Chaudhuri: Advisory board: AbbVie, UCB, GKC, Bial, Cynapsus, Novartis, Lobsor, Stada, Medtronic, Zambon, Profile, Sunovion, Roche, Therevance, Scion, Britannia. Honoraria for lectures: AbbVie, Britannia, UCB, Mundipharma, Zambon, Novartis, Boeringer Ingelheim. Grants (Investigator Initiated): Britania, AbbVie, UCB, GKC, Bial. Aacdemic grants: EU (Horizon 2020), IMI EU, Parkinson’s UK, NIHR, PDNMG, NPF, MRC, Kirby Laing Foundation, Wellcome Trust. Heinz Reichmann: was acting on Advisory Boards, gave lectures and received research grants from Abbott, Abbvie, Bayer Health Care, Bial, Boehringer/Ingelheim, Brittania, Cephalon, Desitin, GSK, Lundbeck, Medtronic, Merck-Serono, Novartis, Orion, Pfizer, TEVA, UCB Pharma, Valeant, Zambon, and Kyowa. Maximilian Kaiser, Anna Sauerbier, Miriam Wienecke, Könül Mammadova, Olaf Gregor: None.
Ethics approval
Obtained and described under methods.
Consent to participate
Obtained and described under methods.
Consent for publication
All authors have approved the publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Klingelhoefer, L., Kaiser, M., Sauerbier, A. et al. Emotional well-being and pain could be a greater determinant of quality of life compared to motor severity in cervical dystonia. J Neural Transm 128, 305–314 (2021). https://doi.org/10.1007/s00702-020-02274-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-020-02274-z