Abstract
Purpose
To develop a model to identify risk factors and predictors of acute pancreatitis in children with pancreaticobiliary maljunction (PBM).
Methods
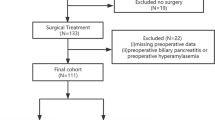
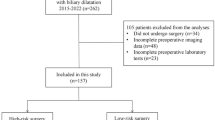
We screened consecutive PBM patients treated at two centers between January, 2015 and July, 2021. For machine learning, the cohort was divided randomly at a 6:4 ratio to a training dataset and a validation dataset. Three parallel models were developed using logistic regression (LR), a support vector machine (SVM), and extreme gradient boosting (XGBoost), respectively. Model performance was judged primarily based on the area under the receiver operating curves (AUC).
Results
A total of 99 patients were included in the analysis, 17 of whom suffered acute pancreatitis and 82 did not. The XGBoost (AUC = 0.814) and SVM (AUC = 0.813) models produced similar performance in the validation dataset; both outperformed the LR model (AUC = 0.805). Based on the SHapley Additive exPlanation values, the most important variable in both the XGBoost and SVM models were age, protein plugs, and white blood cell count.
Conclusions
Machine learning models, especially XGBoost and SVM, could be used to predict acute pancreatitis in children with PBM. The most important contributing factor to the models were age, protein plugs, and white blood cell count.





Similar content being viewed by others
References
Le Roy B, Gagnière J, Filaire L, Fontarensky M, Hordonneau C, Buc E. Pancreaticobiliary maljunction and choledochal cysts: from embryogenesis to therapeutics aspects. Surg Radiol Anat. 2016;38:1053–60.
Kamisawa T, Ando H, Suyama M, Shimada M, Morine Y, Shimada H. Japanese clinical practice guidelines for pancreaticobiliary maljunction. J Gastroenterol. 2012;47:731–59.
Hyvärinen I, Hukkinen M, Kivisaari R, Parviainen H, Nordin A, Pakarinen MP. Increased prevalence of pancreaticobiliary maljunction in biliary malignancies. Scand J Surg. 2019;108:285–90.
Yoshimoto K, Kamisawa T, Kikuyama M, Kuruma S, Chiba K, Igarashi Y. Classification of pancreaticobiliary maljunction and its clinical features in adults. J Hepatobil Pancreat Sci. 2019;26:541–7.
Kamisawa T, Honda G. Pancreaticobiliary maljunction: markedly high risk for biliary cancer. Digestion. 2019;99:123–5.
Kamisawa T, Takuma K, Anjiki H, Egawa N, Kurata M, Honda G, et al. Pancreaticobiliary maljunction. Clin Gastroenterol Hepatol. 2009;7:S84–8.
Fujishiro J, Masumoto K, Urita Y, Shinkai T, Gotoh C. Pancreatic complication in pediatric choledochal cysts. J Pediatr Surg. 2013;48:1897–902.
Urushihara N, Hamada Y, Kamisawa T, Fujii H, Koshinaga T, Morotomi Y, et al. Classification of pancreaticobiliary maljunction and clinical features in children. J Hepatobil Pancreat Sci. 2017;24(8):449–55.
Afzal S, Kleinhenz J. Acute pancreatitis in children. Pediatr Ann. 2021;50(8):e330–5.
Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma S, et al. Artificial intelligence in healthcare: past, present and future. Stroke VascNeurol. 2017;2(4):230–43.
Rajkomar A, Dean J, Kohane I. Machine learning in medicine. N Engl J Med. 2019;380(14):1347–58.
Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K, et al. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134(2):263–9.
Tseng PY, Chen YT, Wang CH, Chiu KM, Peng YS, Hsu SP, et al. Prediction of the development of acute kidney injury following cardiac surgery by machine learning. Crit Care. 2020;24(1):478.
Chen T, Guestrin C. XGBoost: a scalable tree boosting system. In: Proceedings of the 22nd ACM SIGKDD international conference on knowledge discovery and data mining-KDD 2016, San Francisco, CA, USA; 2016. p. 785–94.
Ogunleye A, Wang QG. XGBoost model for chronic kidney disease diagnosis. IEEE/ACM Trans Comput Biol Bioinform. 2020;17:2131–40.
Yuan KC, Tsai LW, Lee KH, Cheng YW, Hsu SC, Lo YS, et al. The development an artificial intelligence algorithm for early sepsis diagnosis in the intensive care unit. Int J Med Inform. 2020;141: 104176.
Xu L, Yang P, Liang W, Liu W, Wang W, Luo C, et al. A radiomics approach based on support vector machine using MR images for preoperative lymph node status evaluation in intrahepatic cholangiocarcinoma. Theranostics. 2019;9(18):5374–85.
Hui B, Qiu JJ, Liu JH, Ke NW. Identification of pancreaticoduodenectomy resection for pancreatic head adenocarcinoma: a preliminary study of radiomics. Comput Math Methods Med. 2020;2020:2761627.
Thapa R, Iqbal Z, Garikipati A, Siefkas A, Hoffman J, Mao Q, et al. Early prediction of severe acute pancreatitis using machine learning. Pancreatology. 2022;22(1):43–50.
Zhu M, Xu C, Yu J, Wu Y, Li C, Zhang M, et al. Differentiation of pancreatic cancer and chronic pancreatitis using computer-aided diagnosis of endoscopic ultrasound (EUS) images: a diagnostic test. PLoS ONE. 2013;8(5): e63820.
Panchoo AV, Infante JC, Rivera Rivera ED. Meandering main pancreatic duct in association with choledochal cysts and acute pancreatitis in pediatrics. Pediatr Ann. 2019;48(10):e412–6.
Artunduaga M, Grover AS, Callahan MJ. Acute pancreatitis in children: a review with clinical perspectives to enhance imaging interpretation. Pediatr Radiol. 2021;51(11):1970–82.
Burrowes DP, Choi HH, Rodgers SK, Fetzer DT, Kamaya A. Utility of ultrasound in acute pancreatitis. Abdom Radiol (NY). 2020;45:1253–64.
Qiu Q, Nian YJ, Guo Y, Tang L, Lu N, Wen LZ, et al. Development and validation of three machine learning models for predicting multiple organ failure in moderately severe and severe acute pancreatitis. BMC Gastroenterol. 2019;19(1):118.
Lan L, Guo Q, Zhang Z, Zhao W, Yang X, Lu H, et al. Classification of infected necrotizing pancreatitis for surgery within or beyond 4 weeks using machine learning. Front Bioeng Biotechnol. 2020;8:541.
Funding
This work was supported by the National Natural Science Foundation of China (#81971685).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to declare.
Ethical statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Ethics Committee of the Children’s Hospital of Soochow University and Xuzhou Children’s Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Han, X., Geng, J., Zhang, Xx. et al. Using machine learning models to predict acute pancreatitis in children with pancreaticobiliary maljunction. Surg Today 53, 316–321 (2023). https://doi.org/10.1007/s00595-022-02571-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02571-y