Abstract
Purpose
To develop machine learning (ML) models to predict the surgical risk of children with pancreaticobiliary maljunction (PBM) and biliary dilatation.
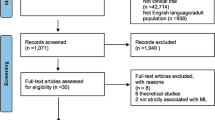
Methods
The subjects of this study were 157 pediatric patients who underwent surgery for PBM with biliary dilatation between January, 2015 and August, 2022. Using preoperative data, four ML models were developed, including logistic regression (LR), random forest (RF), support vector machine classifier (SVC), and extreme gradient boosting (XGBoost). The performance of each model was assessed via the area under the receiver operator characteristic curve (AUC). Model interpretations were generated by Shapley Additive Explanations. A nomogram was used to validate the best-performing model.
Results
Sixty-eight patients (43.3%) were classified as the high-risk surgery group. The XGBoost model (AUC = 0.822) outperformed the LR (AUC = 0.798), RF (AUC = 0.802) and SVC (AUC = 0.804) models. In all four models, enhancement of the choledochal cystic wall and an abnormal position of the right hepatic artery were the two most important features. Moreover, the diameter of the choledochal cyst, bile duct variation, and serum amylase were selected as key predictive factors by all four models.
Conclusions
Using preoperative data, the ML models, especially XGBoost, have the potential to predict the surgical risk of children with PBM and biliary dilatation. The nomogram may provide surgeons early warning to avoid intraoperative iatrogenic injury.







Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are not publicly available due to local restrictions of data protection but are available from the corresponding author on reasonable request.
References
Kamisawa T, Takuma K, Anjiki H, Egawa N, Kurata M, Honda G, et al. Pancreaticobiliary maljunction. Clin Gastroenterol Hepatol. 2009;7:S84–8.
Kamisawa T, Ando H, Suyama M, Shimada M, Morine Y, Shimada H, et al. Japanese clinical practice guidelines for pancreaticobiliary maljunction. J Gastroenterol. 2012;47:731–59.
Hamada Y, Ando H, Kamisawa T, Itoi T, Urushihara N, Koshinaga T, et al. Diagnostic criteria for congenital biliary dilatation 2015. J Hepatobiliary Pancreat Sci. 2016;23:342–6.
Morine Y, Shimada M, Takamatsu H, Araida T, Endo I, Kubota M, et al. Clinical features of pancreaticobiliary maljunction: update analysis of 2nd japan-nationwide survey. J Hepatobiliary Pancreat Sci. 2013;20:472–80.
Nambirajan L, Taneja P, Singh MK, Mitra DK, Bhatnagar V. The liver in choledochal cyst. Trop Gastroenterol. 2000;21:135–9.
Madadi-Sanjani O, Wirth TC, Kuebler JF, Petersen C, Ure BM. Choledochal cyst and malignancy: a plea for lifelong follow-up. Eur J Pediatr Surg. 2019;29:143–9.
Diao M, Li L, Cheng W. Timing of choledochal cyst perforation. Hepatology. 2020;71:753–6.
Ishibashi H, Shimada M, Kamisawa T, Fujii H, Hamada Y, Kubota M, et al. Japanese clinical practice guidelines for congenital biliary dilatation. J Hepatobiliary Pancreat Sci. 2017;24:1–16.
Qiao G, Li L, Li S, Tang S, Wang B, Xi H, et al. Laparoscopic cyst excision and roux-y hepaticojejunostomy for children with choledochal cysts in china: a multicenter study. Surg Endosc. 2015;29:140–4.
Tang ST, Yang Y, Wang Y, Mao YZ, Li SW, Tong QS, et al. Laparoscopic choledochal cyst excision, hepaticojejunostomy, and extracorporeal Roux-en-Y anastomosis: a technical skill and intermediate-term report in 62 cases. Surg Endosc. 2011;25:416–22.
Diao M, Li L, Cheng W. Laparoscopic management for aberrant hepatic duct in children with choledochal cysts. Surg Endosc. 2019;33:2376–80.
Ngiam KY, Khor IW. Big data and machine learning algorithms for health-care delivery. Lancet Oncol. 2019;20:e262–73.
Van Calster B, Wynants L. Machine learning in medicine. N Engl J Med. 2019;380:2588.
Han X, Geng J, Zhang XX, Zhao L, Wang J, Guo WL. Using machine learning models to predict acute pancreatitis in children with pancreaticobiliary maljunction. Surg Today. 2022;53:316–21.
Tseng PY, Chen YT, Wang CH, Chiu KM, Peng YS, Hsu SP, et al. Prediction of the development of acute kidney injury following cardiac surgery by machine learning. Crit Care. 2020;24:478.
Yokoyama S, Hamada T, Higashi M, Matsuo K, Maemura K, Kurahara H, et al. Predicted prognosis of patients with pancreatic cancer by machine learning. Clin Cancer Res. 2020;26:2411–21.
Chen KA, Joisa CU, Stitzenberg KB, Stem J, Guillem JG, Gomez SM, et al. Development and validation of machine learning models to predict readmission after colorectal surgery. J Gastrointest Surg. 2022;26:2342–50.
Kamisawa T, Ando H, Hamada Y, Fujii H, Koshinaga T, Urushihara N, et al. Diagnostic criteria for pancreaticobiliary maljunction 2013. J Hepatobiliary Pancreat Sci. 2014;21:159–61.
Diao M, Li L, Zhang JS, Cheng W. Laparoscopic-assisted clearance of protein plugs in the common channel in children with choledochal cysts. J Pediatr Surg. 2010;45:2099–102.
Chokshi NK, Guner YS, Aranda A, Shin CE, Ford HR, Nguyen NX. Laparoscopic choledochal cyst excision: lessons learned in our experience. J Laparoendosc Adv Surg Tech A. 2009;19:87–91.
Komi N, Udaka H, Ikeda N, Kashiwagi Y. Congenital dilatation of the biliary tract; new classification and study with particular reference to anomalous arrangement of the pancreaticobiliary ducts. Gastroenterol Jpn. 1977;12:293–304.
Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263–9.
Ogunleye A, Wang QG. Xgboost model for chronic kidney disease diagnosis. IEEE/ACM Trans Comput Biol Bioinform. 2020;17:2131–40.
Deng YH, Luo XQ, Yan P, Zhang NY, Liu Y, Duan SB. Outcome prediction for acute kidney injury among hospitalized children via extreme gradient boosting algorithm. Sci Rep. 2022;12:8956.
Rankin S, Han L, Scherzer R, Tenney S, Keating M, Genberg K, et al. A machine learning model for predicting mortality within 90 days of dialysis initiation. Kidney360. 2022;3:1556–65.
Yilmaz A, Hayiroglu MI, Salturk S, Pay L, Demircali AA, Coskun C, et al. Machine learning approach on high risk treadmill exercise test to predict obstructive coronary artery disease by using p, qrs, and t waves’ features. Curr Probl Cardiol. 2022;48:101482.
Nguyen Thanh L, Hien PD, le Dung A, Son TN. Laparoscopic repair for choledochal cyst: Lessons learned from 190 cases. J Pediatr Surg. 2010;45:540–4.
Diao M, Li L, Li Q, Ye M, Cheng W. Challenges and strategies for single-incision laparoscopic roux-en-y hepaticojejunostomy in managing giant choledochal cysts. Int J Surg. 2014;12:412–7.
Yu BH, Lin F. Clinical effects in resection of congenital choledochal cyst of children and jejunum roux-y anastomosis by laparoscope. Eur Rev Med Pharmacol Sci. 2016;20:4530–4.
Lal R, Behari A, Hari RH, Sikora SS, Yachha SK, Kapoor VK. Variations in biliary ductal and hepatic vascular anatomy and their relevance to the surgical management of choledochal cysts. Pediatr Surg Int. 2013;29:777–86.
Chen W, Zhao L, Wang J, Guo WL. Hepatic vascular variations and visual three-dimensional reconstruction technique in pediatric patients with choledochal cyst. Surg Radiol Anat. 2020;42:1489–99.
Kumar S, Singla S, Kumar S, Singh RK, Raj AK, Mandal M. Tactics, techniques, and challenges in the management of giant choledochal cyst in adolescents and adults: a retrospective cohort study. Langenbecks Arch Surg. 2021;406:1925–33.
Wen Z, Cheng W, Liang Q, Liu T, Liang J, Zhang B, et al. Laparoscopic management of choledochal cysts associated with aberrant hepatic ducts. J Laparoendosc Adv Surg Tech A. 2019;29:1060–6.
Oh C, Cheun JH, Kim HY. Clinical comparison between the presence and absence of protein plugs in pediatric choledochal cysts: experience in 390 patients over 30 years in a single center. Ann Surg Treat Res. 2021;101:306–13.
Acknowledgements
This work was partially supported by the National Natural Science Foundation of China (No.81971685), Scientific Research Project of Jiangsu Provincial Health Commission (No.ZD2022015) and Science and Technology Development Project of Suzhou(SKY2022054).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
We have no conflicts of interest to declare.
Ethical statement
The authors are accountable for all aspects of the work to ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Ethics Committee of the Children’s Hospital of Soochow University (no. 20150105015).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mao, Hm., Huang, Sg., Yang, Y. et al. Using machine learning models to predict the surgical risk of children with pancreaticobiliary maljunction and biliary dilatation. Surg Today 53, 1352–1362 (2023). https://doi.org/10.1007/s00595-023-02696-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02696-8