Abstract
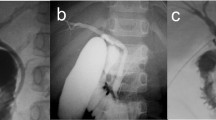
Pancreaticobiliary maljunction (PBM), which may be called by synonymous terms such as “anomalous arrangement of the pancreaticobiliary duct” or “anomalous union of biliopancreatic ducts,” is defined as an anatomical maljunction of the pancreatic duct and the biliary duct outside of the duodenal wall beyond the influence of the sphincter of Oddi. Pancreaticobiliary maljunction is classified into three groups according to the type of the pancreaticobiliary junction. Pancreaticobiliary maljunction is diagnosed mainly by endoscopic retrograde cholangiopancreatography; however, in pediatric patients, it may be diagnosed by intraoperative cholangiography, and more recently has been diagnosed by computed tomographic cholangiography or contrastenhanced helical computed tomography. Children with PBM without choledochal cysts usually do not show any symptoms except for abdominal pain and hyperamylasemia. Pancreaticobiliary maljunction is considered to be a major risk factor for biliary tract malignancy. In patients with PBM, free reflux of pancreatic juice into the biliary tract might induce biliary tract damage and biliary carcinogenesis. Thus, total resection of the extrahepatic bile duct and hepaticojejunostomy are recommended in children diagnosed with PBM with choledochal cyst. Early diagnosis and early surgical treatment provide a good prognosis with few complications. In addition, successive follow-up is necessary for early detection of biliary tract malignancy, especially in patients demonstrating postoperative complications.
Similar content being viewed by others
References
Babbitt DP. Congenital choledochal cyst: new etiological concept based on anomalous relationships of common bile duct and pancreatic bulb. Ann Radiol 1969;12:231–241.
Ohuchida J, Chijiiwa K, Hiyoshi M, Kobayashi K, Konomi H, Tanaka M. Long-term results of treatment for pancreaticobiliary maljunction without bile duct dilatation. Arch Surg 2006;141:1066–1070.
Kusano T, Takao T, Tachibana K, Tanaka Y, Kamachi M, Ikematsu Y, et al. Whether or not prophylactic excision of the extrahepatic bile duct is appropriate for patients with pancreaticobiliary maljunction without bile duct dilatation. Hepatogastroenterology 2005;52:1649–1653.
Funabiki T, Matsubara T, Miyakawa S, Ishihara S. Pancreaticobiliary maljunction and carcinogenesis to biliary and pancreatic malignancy. Langenbecks Arch Surg 2009;394:159–169.
Matsumoto Y, Fujii H, Itakura J, Matsuda M, Nobukawa B, Suda K. Recent advances in pancreaticobiliary maljunction. J Hepatobiliary Surg 2002;9:45–54.
Iwai N, Fumino S, Tsuda T, Ono S, Kimura O, Deguchi E. Surgical treatment for anomalous arrangement of the pancreaticobiliary duct with nondilatation of the common bile duct. J Pediatr Surg 2004;39:1794–1796.
Tashiro S, Imaizumi T, Ohkawa H, Okada A, Katoh T, Kawaharada Y, et al. Pancreaticobiliary maljunction: retrospective and nationwide survey in Japan. J Hepatobiliary Pancreat Surg 2003;10:345–351.
Ono S, Tokiwa K, Iwai N. Cellular activity in the gallbladder of children with anomalous arrangement of the pancreaticobiliary duct. J Pediatr Surg 1999;34:962–966.
Japanese Study Group on Pancreaticobiliary Maljunction (JSPBM), Committee of JSPBM for Diagnostic Criteria. Diagnostic criteria of pancreaticobiliary maljunction. J Hepatobiliary Pancreat Surg 1994;1:219–221.
Kamisawa T, Kurata M, Honda G, Tsuruta K, Okamoto A. Biliopancreatic reflux — pathophysiology and clinical implications. J Hepatobiliary Pancreat Surg 2009;16:19–24.
Kamisawa T, Tu Y, Nakajima H, Egawa N, Tsuruta K, Okamoto A, et al. Acute pancreatitis and a long common channel. Abdom Imaging 2007;32:365–369.
Dinsmore JE, Murphy JJ, Jamieson D. MRCP evaluation of choledochal cyst. J Pediatr Surg 2001;36:829–830.
Lam WWM, Lam TPW, Saing H, Chan FL, Chan KL. MR cholangiography and CT cholangiography of pediatric patients with choledochal cysts. Am J Roentgenol 1999;173:401–405.
Okada T, Sasaki F, Honda S, Naitou S, Onodera Y, Todo S. Usefulness of axial planes of helical computed tomography for diagnosis of pancreaticobiliary maljunction in early infants with negative findings on magnetic resonance cholangiopancreatography. J Pediatr Surg 2008;43:579–582.
Lilly JR, Stellin GP, Karen FM. Forme fruste choledochal cyst. J Pediatr Surg 1985;20:449–451.
Alonso-Lej F, River WB, Passagno DJ. Congenital choledochal cyst, with report of two and an analysis of 94 cases. Surg Gynecol Obstet Int Abstr Surg 1959;108:1–39.
Ono Y, Kaneko K, Tainaka T, Sumida W, Ando H. Pancreaticobiliary maljunction without bile duct dilatation in children: distinction from choledochal cyst. J Pediatr Gastroenterol Nutr 2008;46:555–560.
Fumono S, Ono S, Shimadera S, Kimura O, Iwai N. Impact of age at diagnosis on clinical features in children with anomalous arrangement of the pancreaticobiliary duct. Eur J Pediatr Surg 2010;20:325–329.
Ohkawa H, Sawaguchi S, Khalil B, Ishikawa A, Yamazaki Y. Cholangio- venous reflux as a cause of recurrent hyperamylasemia in choledochal dilatation with anomalous pancreaticobiliary ductal union: an experimental study. J Pediatr Surg 1985;20:53–57.
Kamisawa, T, Tu Y, Kuwata G, Egawa N, Nakajima H, Tsuruta K, et al. Biliary carcinoma risk in patients with pancreaticobiliary maljunction and the degree of extrahepatic bile duct dilatation. Hepatogastroenterology 2006;53:816–818.
Kobayashi S, Asano T, Yamasaki M, Kenmochi T, Saigo K, Ochiai T. Prophylactic excision of the gallbladder and bile duct for patients with pancreaticobiliary maljunction. Arch Surg 2001;136:759–763.
Iwai N, Deguchi E, Yanagihara J, Iwai M, Matsuo H, Todo S, et al. Cancer arising in a choledochal cyst in a 12-year-old girl. J Pediatr Surg 1990;25:1261–1263.
Armanino LP. Idiopathic dilatation of the common bile duct with coexistent primary hepatic carcinoma: report of a case. Ann Intern Med 1946;24:714–726.
Fujiwara Y, Ohizumi T, Kakizaki G, Ishidate T. A case of congenital choledochal cyst associated with carcinoma. J Pediatr Surg 1976;11:587–588.
Hida K, Matsueda K, Kawaguchi T. A 4-year-old boy of choledochal cyst with adenocarcinoma (in Japanese). J Jpn Surg Assoc 1980;41:87.
Nakasako T, Takada T, Satou Y. The youngest case of choledochal cyst with bile duct cancer (in Japanese). Jpn J Gastroenterol 1982;79:926–927.
Niimoto S, Shimada H, Kinoshita H. Proceedings of Japanese Study Group on Pancreaticobiliary Maljunction. A case of choledochal cyst with adenocarcinoma in 18-year-old female (in Japanese) 1983;6:80–81.
Takahashi M, Ohkubo T, Nakashima K. An 18-year-old boy with congenital biliary dilatation associated with common bile duct cancer (in Japanese). Jpn J Gastroenterol 1984;81:145.
Shiroishi M, Watanabe D, Ikeda Y. A case of early stage of cholangiocarcinoma arising from choledochal cyst (in Japanese). Jpn J Gastroenterol 1986;83:299.
Haraoka S, Satou H, Hidaka K. Proceedings of Japanese Study Group on Pancreaticobiliary Maljunction. A case of congenital biliary dilatation with intrapancreatic adenocarcinoma (in Japanese) 1988;11:84.
Fujiwara T, Kobayashi K, Ikeguchi S. Proceedings of Japanese Study Group on Pancreaticobiliary Maljunction. An 18-year-old female presenting cholangiocarcinoma with congenital biliary dilatation (in Japanese) 1989;12:32–33.
Kuriyama Y, Kawamura K, Enomoto H. Biliary carcinoma associated with choledochal cyst in a 15-year old girl. Jpn J Pediatr Surg 1997;32:314–318.
Yamashita S, Ashizawa T, Iijima N, Koyanagi Y, Aoki T, Tsutida A. Two cases of juvenile gallbladder cancer associated with pancreaticobiliary maljunction. J Jpn Pediatr Surg 1998;34:907–914.
Ueda J, Neduka H, Yamamoto S, Yoshimitsu H, Isobe Y, Yamaguchi T, et al. A case of pancreaticobiliary maljunction associated with congenital bile duct dilatation with early bile duct cancer in a 13-year-old girl (in Japanese). Tan To Sui 2000;21:593–597.
Tanaka S, Kubota M, Yagi M, Okuyama N, Ohtaki M, Yamazaki S, et al. An 11-year-old male patient demonstrating cholangiocarcinoma associated with congenital biliary dilatation. J Pediatr Surg 2006;41:E15–E19.
Nakamura H, Katayose Y, Rikiyama T, Onogawa T, Yamamoto K, Yoshida H, et al. Advanced bile duct carcinoma in a 15-year-old patient with pancreaticobiliary maljunction and congenital biliary cystic disease. J Hepatobiliary Pancreat Surg 2008;15:554–559.
Tokiwa K, Ono S, Iwai N. Mucosal cell proliferation activity of the gallbladder in children with anomalous arrangement of the pancreatobiliary duct. J Hepatobiliary Pancreat Surg 1999;6:213–217.
Tokiwa K, Iwai N. Early mucosal changes of the gallbladder in patients with anomalous arrangement of the pancreaticobiliary duct. Gastroenterology 1996;110:1614–1618.
Noguchi A. Cell kinetic studies on mucosa of the gallbladder by using anti-bromodeoxyuridine monoclonal antibody in patients with anomalous arrangement of the pancreatico-biliary duct system. Jpn J Gastroenterol Surg 1988;21:210–220.
Yoshioka H, Koyama K, Sato Y, Tanaka J, Matsushiro T, Yamazaki T. Cell kinetic studies on the gallbladder epithelium in patients with anomalous arrangement of pancreatobiliary duct. Jpn J Gastroenterol 1991;88:1089–1096.
Kubota D, Kinoshita H, Hirohashi K, Kudo S, Fujio N, Iwasa R, et al. Immunohistochemical staining of gallbladders from patients with pancreaticobiliary maljunction by antibody to proliferating cell nuclear antigen. Gastroenterol Jpn 1992;27:266.
Fujita T, Shimada H, Nakagawara G. Cell kinetic study of the gallbladder epithelium, with special reference to the pancreaticobiliary maljunction. J Hepatobiliary Pancreat Surg 1994;1:229–235.
Kaneko K, Ando H, Ito T, Kasai K, Watanabe Y, Seo T. Increased cell proliferation and transforming growth factor-α (TGFα) in the gall-bladder epithelium of patients with pancreaticobiliary maljunction. Pathol Int 1996;46:253–260
Ono S, Fumino S, Shimadera S, Iwai N. Long-term outcomes after hepaticojejunostomy for choledochal cyst: a 10- to 27-year followup. J Pediatr Surg 2010;45:376–378.
Watanabe Y, Toki A, Todani T. Bile duct cancer developed after cyst excision for choledochal cyst. J Hepatobiliary Pancreat Surg 1999;6:207–212.
Ono S, Sakai S, Kimura O, Iwai N. Development of bile duct cancer in a 26-year-old man after resection of infantile choledochal cyst. J Pediatr Surg 2008;43:E17–E19.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ono, S., Fumino, S. & Iwai, N. Diagnosis and treatment of pancreaticobiliary maljunction in children. Surg Today 41, 601–605 (2011). https://doi.org/10.1007/s00595-010-4492-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-010-4492-9