Abstract
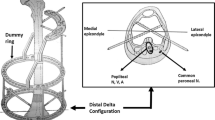
The purpose of this study was to develop a technique allowing a faster return to previous activities after surgical treatment of short transverse and oblique fractures of the diaphysis of the fifth metacarpal. It consisted of an anterograde and retrograde centromedullary double pinning connected. Our series included 40 patients of average age 25 years including 2 women. In 20 cases (group I), an anterograde centromedullary pinning with a 1.6- or 2-mm pin was performed followed by a 6-week orthosis and then 2-week self-education. In 20 cases (group II), an anterograde and retrograde centromedullary double pinning was performed using 2 1.5-mm pins connected by a connector (MétaHUS®, Arex™). A first pin was introduced into the canal antegrade, then the second retrograde. The 2 externalized pins were connected, and self-rehabilitation was encouraged. Mean tourniquet time was 14.75 min (group I) and 15.8 min (group II), respectively. At the last follow-up, the average pain was 0.35/10 and 0.2/10, the Quick DASH 0.68/100 and 0.57/100, the strength of the hand 94.65% and 94.35%, the active flexion MCP 98.5% and 99%, respectively. MCP active extension was 98.5% and 98.75%; the sick leave was 8.4 and 6.3 weeks. All fractures healed without recovery with 3 complications: 2 infections on pins, in each group, 1 CRPS1 (group I). Our results seem to show that the technique of anterograde and retrograde centromedullary double pinning connected in the treatment of short transverse and oblique fractures of the diaphysis of the fifth metacarpal gives results at least as good as the reference technique with a non-negligible socioeconomic advantage, a less time off work.
Résumé
Le but de cette étude était d’évaluer une technique permettant un retour plus rapide aux activités antérieures après traitement chirurgical des fractures transversales et obliques courtes de la diaphyse du cinquième métacarpien. Elle consistait en un double brochage centromédullaire antérograde et rétrograde connecté. Notre série comprenait 40 patients d’âge moyen 25 ans dont 2 femmes. Dans 20 cas (groupe I) un brochage centromédullaire antérograde avec une broche de 1.6 ou 2mm a été réalisé suivie d’une orthèse 6 semaines puis autorééducation 2 semaines. Dans 20 cas (groupe II) un double brochage centromédullaire antéro- et rétrograde a été réalisé à l’aide de 2 broches de 1.5 mm reliées par un connecteur (MétaHUS®, Arex™). Une première broche était introduite dans le canal en antérograde, puis la seconde en rétrograde. Les 2 broches extériorisées étaient connectées et l’autorééducation encouragée. Le temps de garrot moyen était 14.75min (groupe I) et 15.8min (groupe II) respectivement. Au dernier recul, la douleur moyenne était de 0.35/10 et 0.2/10, le Quick DASH 0.68/100 et 0.57/100, la force de la poigne 94.65% et 94.35%, la flexion active MCP 98.5% et 99 %, l’extension active MCP 98.5% et 98.75 %, l’arrêt de travail 8.4 et 6.3 semaines. Toutes les fractures ont consolidé sans reprise avec 3 complications : 2 infections sur broches, dans chacun des groupes, 1 SDRC1 (groupe I). Nos résultats semblent montrer que la technique du double brochage centromédullaire antérograde et rétrograde connecté dans le traitement des fractures transversales et obliques courtes de la diaphyse du cinquième métacarpien donne des résultats au moins aussi bons que la technique de référence avec un avantage socioéconomique non négligeable, une moindre durée d’arrêt de travail.


Similar content being viewed by others
References
Kollitz KM, Hammert WC, Vedder NB, Huang JI (2014) Metacarpal fractures: treatment and complications. Hand 9:16–23
Corkum JP, Davison PG, Lalonde DH (2013) Systematic review of the best evidence in intramedullary fixation for metacarpal fractures. Hand (NY) US 8:253–260
Lamraski G, Monsaert A, De Maeseneer M, Haentjens P (2006) Reliability and validity of plain radiographs to assess angulation of small finger metacarpal neck fractures: human cadaveric study. J Orthop Res 24:37–45
Court-Brown CM (2015) The epidemiology of fractures. In: Court-Brown CM, Heckman JD, McQueen MM, Ricci WM, Tornetta P (eds) Rockwood and Green’s fractures in adults, 8th edn. Wolters Kluwer Health, Philadelphia, pp 59–108
de Jonge JJ, Kingma J, van der Lei B, Klasen HJ (1994) Fractures of the metacarpals. A retrospective analysis of incidence and aetiology and a review of the English-language literature. Injury 25:365–369
Low CK, Wong HC, Low YP, Wong HP (1995) A cadaver study of the effects of dorsal angulation and shortening of the metacarpal shaft on the extension and flexion force ratios of the index and little fingers. J Hand Surg Br 20:609–613
Soong M, Got C, Katarincic J (2010) Ring and little finger metacarpal fractures: mechanisms, locations, and radiographic parameters. J Hand Surg Am 35:1256–1259
Fusetti C, Meyer H, Borisch N (2002) Complications of plate fixation in metacarpal fractures. J Trauma 52:535–539
Firoozbakhsh KK, Moneim MS, Doherty W, Naraghi FF (1996) Internal fixation of oblique metacarpal fractures: a biomechanical evaluation by impact loading. Clin Orthop Relat Res 325:296–301
Mann RJ, Black D, Constine R, Daniels AU (1985) A quantitative comparison of metacarpal fracture stability with five different methods of internal fixation. J Hand Surg Am 10:1024–1028
Curtis BD, Fajolu O, Ruff ME, Litsky AS (2015) Fixation of metacarpal shaft fractures: biomechanical comparison of intramedullary nail crossed K-wires and plate-screw constructs. Orthop Surg 7:256–260
Vanik RK, Weber RC, Matloub HS, Sanger JR, Gingrass RP (1984) The comparative strengths of internal fixation techniques. J Hand Surg Am 9:216–221
Facca S, Ramdhian R, Pelissier A (2010) Fifth metacarpal neck fracture fixation: locking plate versus K-wire? Orthop Traumatol Surg Res 96:506–512
Lee SK, Kim KJ, Choy WS (2013) Modified retrograde percutaneous intramedullary multiple Kirschner wire fixation for treatment of unstable displaced metacarpal neck and shaft fractures. Eur J Orthop Surg Traumatol 23:535–543
Meals C, Meals R (2013) Hand fractures: a review of current treatment strategies. J Hand Surg Am 38:1021–1031
Sarmiento A, Latt L, Uliol A, Sinclair W (1974) The role of soft tissues in the stabilization of tibial fractures. Clin Orthop 105:116–129
Lord R (1957) Intramedullary fixation of metacarpal fractures. JAMA 164:1746–1749
Foucher G (1995) “Bouquet” osteosynthesis in metacarpal neck fractures: a series of 66 patients. J Hand Surg Am 20:86–90
Cheah A, Yao J (2016) Hand fractures: indications, the tried and the true and new innovations. J Hand Surg Am 41:712–722
Zhang B, Hu P, Yu KL, Bai JB, Tian DH, Zhang GS, Shao XZ, Zhang YZ (2016) Comparison of AO titanium locking plate and screw fixation versus anterograde intramedullary fixation for isolated unstable metacarpal and phalangeal fractures. Orthop Surg 8:316–322
Ozer K, Gillani S, Williams A, Peterson S, Morgan S (2008) Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg Am 33:1724–1731
Faraj AA, Davis TR (1999) Percutaneous intramedullary fixation of metacarpal shaft fractures. J Hand Surg Br 24:76–79
Hiatt SV, Begonia MT, Thiagarajan G, Hutchison RL (2015) Biomechanical comparison of 2 methods of intramedullary K-wire fixation of transverse metacarpal shaft fractures. J Hand Surg Am 40:1586–1590
Hargreaves DG, Drew SJ, Eckersley R (2004) Kirschner wire pin tract infection rates: a randomized controlled trial between percutaneous and buried wires. J Hand Surg Br 29:374–376
Ridley TJ, Freking W, Erickson LO, Ward CM (2017) Incidence of treatment for infection of buried versus exposed Kirschner wires in phalangeal, metacarpal, and distal radial fractures. J Hand Surg Am 42:525–531
Hsu LP, Schwartz EG, Kalainov DM, Chen F, Makowiec RL (2011) Complications of K-wire fixation in procedures involving the hand and wrist. J Hand Surg Am 36:610–616
Van Bussel EM, Houwert RM, Kootstra TJM, van Heijl M, Van der Velde D, Wittich P, Keizer J (2019) Anterograde intramedullary Kirschner wire fixation of displaced metacarpal shaft fractures. Eur J Trauma Emerg Surg 45:65–71
Shehadi SI (1991) External fixation of metacarpal and phalangeal fractures. J Hand Surg Am 16:544–550
Bible JE, Mir HR (2015) External fixation: principles and applications. J Am Acad Orthop Surg 23:683–690
Westbrook AP, Davis TR, Armstrong D (2008) The clinical significance of malunion of fractures of the neck and shaft of the little finger metacarpal. J Hand Surg Eur 33:732–739
WIRE Research Collaborative (2018) Buried versus exposed Kirschner wires following fixation of hand fractures: I clinician and patient surveys. Plast Reconstr Surg Glob Open 6(4):1747. https://doi.org/10.1097/gox.0000000000001747
Del Pinal F, Moraleda E, Ruas JS, de Piero GH, Cerezal L (2015) Minimally invasive fixation of fractures of the phalanges and metacarpals with intramedullary cannulated headless compression screws. J Hand Surg Am 40:692–700
Avery M, Klinge S, Dyrna F, Pauzenberger L, Lam D, Cote M, DiVenere J, Mazzocca A, Rodner C (2017) Headless compression screw versus Kirschner wire fixation for metacarpal neck fractures: a biomechanical study. J Hand Surg Am 42:3921–3926
Ruchelsman D, Puri S, Feinberg-Zadek N, Leibman MI, Belsky MR (2014) Clinical outcomes of limited-open retrograde intramedullary headless screw fixation of metacarpal fractures. J Hand Surg Am 39:2390–2395
Acknowledgements
Professor Erik-André Sauleau, Methods Group in Clinical Research, Public Health Service, Strasbourg University Hospitals, who carried out the statistical study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Philippe Liverneaux has a relationship with Newclip Technics, Biomodex, Zimmer Biomet, Argomedical. None of the other authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lazarus, P., Hidalgo Diaz, J.J., Xaxier, F. et al. Transverse and oblique fractures of the diaphysis of the fifth metacarpal: surgical outcomes for antegrade intramedullary pinning versus combined antegrade and retrograde intramedullary pinning. Eur J Orthop Surg Traumatol 30, 425–433 (2020). https://doi.org/10.1007/s00590-019-02587-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02587-0
Keywords
- Fifth metacarpal fracture
- Antegrade intramedullary pinning
- Combined antegrade and retrograde intramedullary pinning