Abstract
Background
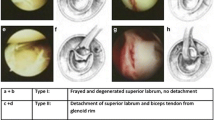
Among the uncommon and frequently missed orthopedics injuries is the posterior shoulder dislocation, accounting for about 2–4 % of all shoulder dislocations. Commonly, it is associated with the well-known reverse Hill–Sachs lesion. Several surgical treatment modalities such as transfer of subscapularis tendon or lesser tuberosity, humeral rotational osteotomy, osteochondral grafts were used to repair this defect. Hemiarthroplasty or total shoulder arthroplasty was used as salvage procedure in non-constructable defect or neglected old dislocation.
Patients and methods
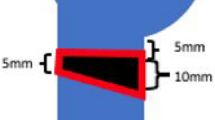
This study included 11 patients with locked chronic posterior shoulder dislocation and reverse Hill–Sachs defects falling in the target range (25–50 % of the head size). The mean age of the patients was 39 (range 31–49) years. Mean time from injury to surgery was 9 (range 3–18) weeks. Open reduction in the dislocated head with the transfer of subscapularis tendon and the attached lesser tuberosity was done to reconstruct the reverse Hill–Sachs defect. The transferred tuberosity was fixed with size 5 Ethibond sutures.
Results
The mean follow-up period was 29 (range 24–39) months. The median of the scores was much improved, reaching 30 (range 20–34) (satisfactory) compared with preoperative median of 24 (range 20–25) (unsatisfactory). This was statistically highly significant (P = 0.002). Postoperatively, 9 patients had no pain or restricted daily living activities. No patient had symptoms of shoulder instability. According to the modified UCLA shoulder rating scale, there were 4 patients rated excellent, 5 patients rated good, one patient rated fair and one patient rated poor.
Conclusion
Reconstructing the reverse Hill–Sachs defect provides adequate stability, pain relief and function in patients with locked chronic posterior shoulder dislocation and a defect involving 25–50 % of the humeral head. The used technique is simple and cost effective with no need for subsequent hardware removal.
Level of evidence
II.







Similar content being viewed by others
References
Amstutz HC, Sew Hoy AL, Clarke IC (1981) UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res 155:7–20
Aparicio G, Calvo E, Bonilla L, Espejo L (2000) Neglected traumatic posterior dislocations of the shoulder: controversies on indications for treatment and new CT scan findings. J Orthop Sci 5:37–42
Bock P, Kluger R, Hintermann B (2007) Anatomical reconstruction for reverse Hill–Sachs lesions after posterior locked shoulder dislocation fracture. Arch Orthop Trauma Surg 127:543–548
Charalambous CP, Gullett TK, Ravenscroft MJ (2009) Modification of McLaughlin procedure for persistent shoulder instability: technical note. Arch Orthop Trauma Surg 129:753–755
Checchia SL, Santos PD, Miyazaki AN (1998) Surgical treatment of acute and chronic posterior fracture dislocation of the shoulder. J Shoulder Elbow Surg 7:53–65
Chen AL, Hunt SA, Zuckerman JD (2005) Humeral head impression fractures and head-splitting fractures. In: Zuckerman JD, Koval KJ (eds) Shoulder fractures: the practical guide to management. Thieme, New York, NY, pp 120–143
Cicak N (2004) Posterior dislocation of the shoulder. J Bone Joint Surg (Br) 86(3):324–332
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 6:160–164
Delcogliano A, Caporaso A, Chiossi S, Delcogliano M (2005) Surgical management of chronic, unreduced posterior dislocation of the shoulder. Knee Surg Sports Traumatol Arthrosc 13:151–155
Dubousset J (1967) Posterior dislocations of the shoulder [in French]. Rev Chir Orthop Reparatrice Appar Mot 53(1):65–85
Gerber C (1991) L’instabilité postérieure de l’épaule. In: Cahiers d’Enseignement de la SOFCOT. Expansion Scienti-fique Française, Paris, pp 223–245
Gerber C, Lambert SM (1996) Allograft reconstruction of segmental defects of the humeral head for the treatment of chronic locked posterior dislocation of the shoulder. J Bone Joint Surg (Am) 78:376–382
Hawkins RJ, Neer CS, Pianta RM, Mendoza FX (1987) Locked posterior dislocation of the shoulder. J Bone Joint Surg 69:9–18
Keppler P, Holz U, Thielemann FW, Meinig R (1994) Locked posterior dislocation of the shoulder: treatment using rotational osteotomy of the humerus. J Orthop Trauma 8:286–292
Kokkalis ZT, Mavrogenis AF, Ballas EG, Papanastasou J, Papajelopoulos PJ (2013) Modified McLaughlin technique for neglected locked posterior dislocation of the shoulder. Orthopedics 36(7):912–916
Kronberg M, Brostrom LA (1995) Rotation osteotomy of the proximal humerus to stabilise the shoulder. Five years’ experience. J Bone Joint Surg (Br) 77(6):924–927
Loebenberg MI, Cuomo F (2000) The treatment of chronic anterior and posterior dislocations of the glenohumeral joint and associated articular surface. Orthop Clin North Am 31:23–34
McLaughlin HL (1952) Posterior dislocation of the shoulder. J Bone Joint Surg (Am) 24:584–590
Ozkan M, Gul O, Bacakoglu K, Ozcan C, Ekin A (2000) Treatment of posterior locked fracture dislocation of the shoulder with hemiarthroplasty. Acta Orthop Traumatol Turc J 34:45–49
Robinson CM (2005) Posterior shoulder dislocations and fracture dislocations. J Bone Joint Surg (Am) 87:639–650
Robinson CM, Akhtar A, Mitchell M, Beavis C (2007) Complex posterior fracture-dislocation of the shoulder. Epidemiology, injury patterns, and results of operative treatment. J Bone Joint Surg 89:1454–1466
Sperling JW, Cofield RH, Rowland CM (2004) Minimum fifteen-years follow-up of Neer hemiarthroplasty and total shoulder arthroplasty in patients aged fifty years or younger. J Shoulder Elbow Surg 13:604–613
Wadlington VR, Hendrix RW, Rogers LF (1992) Computed tomography of posterior fracture-dislocations of the shoulder: case reports. J Trauma 32:113–115
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interests for this study.
Ethical review committee statement
This study was conducted after approval of the University ethical committee, and a written approval statement was collected from all the included subjects before surgery. This study was conducted at Menofiya University Hospitals and Tanta University Hospitals.
Rights and permissions
About this article
Cite this article
Shams, A., El-Sayed, M., Gamal, O. et al. Modified technique for reconstructing reverse Hill–Sachs lesion in locked chronic posterior shoulder dislocation. Eur J Orthop Surg Traumatol 26, 843–849 (2016). https://doi.org/10.1007/s00590-016-1825-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-016-1825-4