Abstract
Background
Thoracic kyphosis, or loss of lumbar lordosis, is often equated with osteoporosis because vertebral fractures are assumed to be a major causative factor, in addition to degeneration related to age. Despite the few studies aiming to measure the natural change in global sagittal alignment (GSA) that occurs with advancing age, the overall effect of conservatively managed osteoporotic vertebral compression fractures (OVCF) on the GSA in the elderly remains poorly understood.
Objective
To systematically evaluate the relevant literature regarding the influence of OVCF on the GSA compared to patients of similar age without fractures using the following radiological parameters: Pelvic Incidence (PI), Pelvic Tilt (PT), Lumbar Lordosis (LL), Thoracic Kyphosis (TK), Sagittal Vertical Axis (SVA) and Spino-sacral Angle (SSA).
Methods
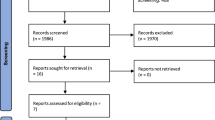
A systematic review of the English language literature dating up until October 2022, was undertaken utilizing the PRISMA guidelines.
Results
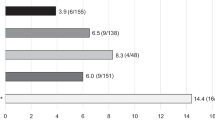
Of a total of 947 articles, 10 studies met the inclusion criteria (4 Level II, 4 level III and 2 level IV evidence) and were subsequently analyzed. Overall, 584 patients (8 studies) of mean age 73.7 years (69.3–77.1) had acute OVCF of one or more vertebra that were managed conservatively. The male to female ratio was 82:412. Five studies mentioned the number of fractured vertebrae, with a total of 393 in 269 patients (average of 1.4 fractured vertebrae per patient). Their pre-operative radiological parameters on standing X-rays showed a mean PI of 54.8°, PT 24°, LL 40.8°, TK 36.5°, PI-LL 14°, SVA 4.8 cm, and SSA 115°. In addition, 437 patients were used as a control group with osteoporosis without fractured vertebrae, (6 studies) with an average age of 72.4 years (67–77.8) and male to female ratio of 96:210 (5 studies). They all had upright X-rays to assess their global sagittal alignments. Radiological parameters showed an average PI of 54.3°, PT 17.3°, LL 43.4°, TK 31.25°, PI-LL 10.95°, SVA 1.27 cm and SSA 125°. A statistical analysis comparing the OVCF group with the control group (4 studies), showed a significant increase in PT of 5.97° (95%CI 2.63, 9.32; P < 0.0005), a significant increase in TK by 8.28° (95%CI 2.15, 14.4; P < 0.008), an increase in PI-LL by 6.72° (95%CI 3.39, 10.04; P < 0.0001), an increase in SVA by 1.35 cm (95%CI 0.88, 1.83; P < 0.00001), and a decrease in SSA by 10.2° (95%CI 10.3, 23.4; P < 0.00001).
Conclusion
Osteoporotic vertebral compression fractures managed conservatively appear to be a significant causate factor of global sagittal imbalance.


Similar content being viewed by others
Availability of data and material
The data that support the findings of this study are available on request from the corresponding author.
Code availability
Not applicable.
References
LeBoff MS, Greenspan SL, Insogna KL, Lewiecki EM, Saag KG, Singer AJ, Siris ES (2022) The clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 33:2049–2102. https://doi.org/10.1007/s00198-021-05900-y
Zethraeus N, Borgstrom F, Strom O, Kanis JA, Jonsson B (2007) Cost-effectiveness of the treatment and prevention of osteoporosis—a review of the literature and a reference model. Osteoporos Int 18:9–2
Fechtenbaum J et al. (2005) Reporting of vertebral fractures on spine X-rays. Osteoporosis Int 16(12).
European Prospective Osteoporosis Study (EPOS) Group, Felsenberg D, Silman AJ et al (2002) Incidence of vertebral fracture in Europe: results from the European Prospective Study (EPOS). J Bone Miner Res 17(4):716–724
Spiegl UJ, Josten C, Devitt BM, Heyde CE (2017) Incomplete burst fractures of the thoracolumbar spine: a review of literature. Eur Spine J 26(12):3187–3198
Francis RM, Aspray TJ, Hide G, Sutcliffe AM, Wilkinson P (2008) Back pain in osteoporotic vertebral fractures. Osteoporos Int 19(7):895–903. https://doi.org/10.1007/s00198-007-0530-x. (Epub 2007 Dec 11)
Lafage R, Schwab F, Challier V, Henry JK, Gum J, Smith J et al (2016) Defining spino-pelvic alignment thresholds: should operative goals in adult spinal deformity surgery account for age? Spine (Phila Pa 1976) 41:62–68
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359(9319):1761–1767
Lamartina C, Berjano P (2014) Classification of sagittal imbalance based on spinal alignment and compensatory mechanisms. Eur Spine J 23(6):1177–1189. https://doi.org/10.1007/s00586-014-3227. (PMID: 24682355)
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1):1–9
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2021) Cochrane handbook for systematic reviews of interventions. Cochrane, Oxford
Fechtenbaum J, Etcheto A, Kolta S, Feydy A, Roux C, Briot K (2016) Sagittal balance of the spine in patients with osteoporotic vertebral fractures. Osteoporos Int 27(2):559–567
Cao Z, Wang G, Hui W, Liu B, Liu Z, Sun J (2020) Percutaneous kyphoplasty for osteoporotic vertebral compression fractures improves spino-pelvic alignment and global sagittal balance maximally in the thoracolumbar region. PLoS ONE 15(1):e0228341
Yokoyama K, Kawanishi M, Yamada M, Tanaka H, Ito Y, Kawabata S, Kuroiwa T (2015) Postoperative change in sagittal balance after Kyphoplasty for the treatment of osteoporotic vertebral compression fracture. Eur Spine J 24(4):744–749
Pumberger M, Schitz F, Bürger J, Schömig F, Putzier M, Palmowski Y (2020) Kyphoplasty restores the global sagittal balance of the spine independently from pain reduction. Sci Rep 10(1):8894
Chau LTC, Hu Z, Ko KSY, Man GCW, Yeung KH, Law YY, Lau LCM, Wong RMY, Chu WCW, Cheng JCY, Law SW (2021) Global sagittal alignment of the spine, pelvis, lower limb after vertebral compression fracture and its effect on quality of life. BMC Musculoskelet Disord 22(1):476
Baek SW, Kim C, Chang H (2015) The relationship between the spinopelvic balance and the incidence of adjacent vertebral fractures following percutaneous vertebroplasty. Osteoporos Int 26(5):1507–1513
Sutipornpalangkul W, Zambrana L, Gianakos A, Lane JM (2016) Comparison of sagittal balance between radiofrequency targeted vertebral augmentation and balloon kyphoplasty in treatment of vertebral compression fracture: a retrospective study. J Med Assoc Thai 99(9):1025–1032 (PMID: 29927208)
Kim DH, Choi DH, Park JH, Lee JH, Choi YS (2015) What is the effect of spino-pelvic sagittal parameters and back muscles on osteoporotic vertebral fracture? Asian Spine J 9(2):162–169
Takeda N, Kobayashi T, Atsuta Y, Matsuno T, Shirado O, Minami A (2009) Changes in the sagittal spinal alignment of the elderly without vertebral fractures: a minimum 10-year longitudinal study. J Orthop Sci 14(6):748–753
Canbek U, Rosberg DBH, Rosberg HE, Canbek TD, Akgün U, Comert A (2021) The effect of age, BMI, and bone mineral density on the various lumbar vertebral measurements in females. Surg Radiol Anat 43(1):101–108
Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H (2011) The Oxford CEBM evidence levels of evidence (introductory document). Oxford Centre for Evidence-Based Medicine, Oxford
Roussouly P, Nnadi C (2010) Sagittal plane deformity: an overview of interpretation and management. Eur Spine J 19:1824–1836
Lee JS, Lee HS, Shin JK, Goh TS, Son SM (2013) Prediction of sagittal balance in patients with osteoporosis using spinopelvic parameters. Eur Spine J 22:1053–1058
Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A (2019) Sagittal balance of the spine. Eur Spine J 28:1889–1905
Cirillo Totera JI, Fleiderman Valenzuela JG, Garrido Arancibia JA, Pantoja Contreras ST, Lalanne LB, Alvarez-Lemos FL (2021) Sagittal balance: from theory to clinical practice. EFORT Open Rev 6(12):1193–1202. https://doi.org/10.1302/2058-5241.6.210062.
Le Huec JC, Hasegawa K (2016) Normative values for the spine shape parameters using 3D standing analysis from a database of 268 asymptomatic Caucasian and Japanese subjects. Eur Spine J Of Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 25:3630–3637. https://doi.org/10.1007/s00586-016-4485-5
Takeda N, Kobayashi T, Atsuta Y, Matsuno T, Shirado O, Minami A (2009) Changes in the sagittal spinal alignment of the elderly without vertebral fractures: a minimum 10-year longitudinal study. J Orthop Sci 14:748–753
Roux C, Fechtenbaum J, Kolta S, Said-Nahal R, Briot K, Benhamou CL (2010) Prospective assessment of thoracic kyphosisin postmenopausal women with osteoporosis. J Bone Miner Res 25(2):362–368
Dai J, Yu X, Huang S, Fan L, Zhu G, Sun H, Tang X (2015) Relationship between sagittal spinal alignment and the incidence of vertebral fracture in menopausal women with osteoporosis: a multicenter longitudinal follow-up study. Eur Spine J 24(4):737–743
Schwab FJ, Patel A, Ungar B, Farcy JP, Lafage V (2010) Adult spinal deformity: postoperative standing imbalance. How much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine 35:2224–2231
Diebo BG, Varghese JJ, Lafage R, Schwab FJ, Lafage V (2015) Sagittal alignment of the spine: What do you need to know? Clin Neurol Neurosurg 139:295–301
Glassman SD, Bridwell K, Dimar JR et al (2005) The impact of positive sagittal balance in adult spinal deformity. Spine 30:2024–2029
Roussouly P, Gollogly S, Noseda O, Berthonnaud E, Dimnet J (2006) The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine 31(11):E320–E325
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
NAQ, KS and EN contributed to the study conception and design. Data collection and analysis were performed by EN, DP, AM and MM. The first draft of the manuscript was written by EN. And all authors commented on previous versions of the manuscript. Final version of the article reviewed by NAQ, KS and EN and SK.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no competing interests. No financial support was provided for this study, and no potential conflict of interest or associated biases were present from any of the authors.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Najjar, E., Pasku, D., Mardashti, A. et al. The influence of osteoporotic vertebral fractures on global sagittal alignment in elderly patients: a systematic review and meta-analysis. Eur Spine J 32, 2580–2587 (2023). https://doi.org/10.1007/s00586-023-07780-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07780-8