Abstract
Purpose
To propose a fully automated deep learning (DL) framework for the vertebral morphometry and Cobb angle measurement from three-dimensional (3D) computed tomography (CT) images of the spine, and validate the proposed framework on an external database.
Methods
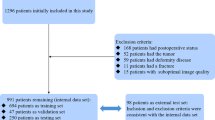
The vertebrae were first localized and segmented in each 3D CT image using a DL architecture based on an ensemble of U-Nets, and then automated vertebral morphometry in the form of vertebral body (VB) and intervertebral disk (IVD) heights, and spinal curvature measurements in the form of coronal and sagittal Cobb angles (thoracic kyphosis and lumbar lordosis) were performed using dedicated machine learning techniques. The framework was trained on 1725 vertebrae from 160 CT images and validated on an external database of 157 vertebrae from 15 CT images.
Results
The resulting mean absolute errors (± standard deviation) between the obtained DL and corresponding manual measurements were 1.17 ± 0.40 mm for VB heights, 0.54 ± 0.21 mm for IVD heights, and 3.42 ± 1.36° for coronal and sagittal Cobb angles, with respective maximal absolute errors of 2.51 mm, 1.64 mm, and 5.52°. Linear regression revealed excellent agreement, with Pearson’s correlation coefficient of 0.943, 0.928, and 0.996, respectively.
Conclusion
The obtained results are within the range of values, obtained by existing DL approaches without external validation. The results therefore confirm the scalability of the proposed DL framework from the perspective of application to external data, and time and computational resource consumption required for framework training.






Similar content being viewed by others
Notes
DSC is a standard metric for segmentation performance, computed as a double of the ratio of the achieved and reference segmentation overlap in pixels against the total number of pixels of both segmentations. As such, it is equal to the harmonic mean of the binary classification precision and recall, i.e., the F1 score.
References
Guglielmi G, Diacinti D, van Kuijk C et al (2008) Vertebral morphometry: current methods and recent advances. Eur Radiol 18:1484–1496. https://doi.org/10.1007/s00330-008-0899-8
Labrom FR, Izatt MT, Claus AP, Little JP (2021) Adolescent idiopathic scoliosis 3D vertebral morphology, progression and nomenclature: a current concepts review. Eur Spine J 30:1823–1834. https://doi.org/10.1007/s00586-021-06842-z
Al-Bashir AK, Al-Abed MA, Amari HK et al (2019) Computer-based Cobb angle measurement using deflection points in adolescence idiopathic scoliosis from radiographic images. Neural Comput Appl 31:1547–1561. https://doi.org/10.1007/s00521-018-3614-y
Štern D, Njagulj V, Likar B et al (2013) Quantitative vertebral morphometry based on parametric modeling of vertebral bodies in 3D. Osteoporos Int 24:1357–1368. https://doi.org/10.1007/s00198-012-2089-4
Neubert A, Fripp J, Engstrom C et al (2013) Three-dimensional morphological and signal intensity features for detection of intervertebral disc degeneration from magnetic resonance images. J Am Med Inform Assoc 20:1082–1090. https://doi.org/10.1136/amiajnl-2012-001547
Payer C, Štern D, Bischof H, Urschler M (2020) Coarse to fine vertebrae localization and segmentation with spatialconfiguration-net and U-net. In: Proceedings of 15th international joint conference on computer vision, imaging and computer graphics theory and applications—VISAPP 2020. SciTePress, Valetta, Malta, pp 124–133
Huang J, Shen H, Wu J et al (2020) Spine explorer: a deep learning based fully automated program for efficient and reliable quantifications of the vertebrae and discs on sagittal lumbar spine MR images. Spine J 20:590–599. https://doi.org/10.1016/j.spinee.2019.11.010
Tam CM, Zhang D, Chen B et al (2020) Holistic multitask regression network for multiapplication shape regression segmentation. Med Image Anal 65:101783. https://doi.org/10.1016/j.media.2020.101783
Cheng P, Yang Y, Yu H, He Y (2021) Automatic vertebrae localization and segmentation in CT with a two-stage dense-U-net. Sci Rep 11:22156. https://doi.org/10.1038/s41598-021-01296-1
Liu J, Yuan C, Sun X et al (2021) The measurement of Cobb angle based on spine X-ray images using multi-scale convolutional neural network. Phys Eng Sci Med 44:809–821. https://doi.org/10.1007/s13246-021-01032-z
Vrtovec T, Ibragimov B (2022) Spinopelvic measurements of sagittal balance with deep learning: systematic review and critical evaluation. Eur Spine J. https://doi.org/10.1007/s00586-022-07155-5
Ibragimov B, Korez R, Likar B et al (2017) Segmentation of pathological structures by landmark-assisted deformable models. IEEE Trans Med Imaging 36:1457–1469. https://doi.org/10.1109/TMI.2017.2667578
Vrtovec T, Pernuš F, Likar B (2009) A review of methods for quantitative evaluation of spinal curvature. Eur Spine J 18:593–607
Sekuboyina HME, Bayat A et al (2021) VerSe: a vertebrae labelling and segmentation benchmark for multi-detector CT images. Med Image Anal 73:102166. https://doi.org/10.1016/j.media.2021.102166
Sebaaly A, Silvestre C, Rizkallah M et al (2021) Revisiting thoracic kyphosis: a normative description of the thoracic sagittal curve in an asymptomatic population. Eur Spine J 30:1184–1189. https://doi.org/10.1007/s00586-020-06670-7
Langensiepen S, Semler O, Sobottke R et al (2013) Measuring procedures to determine the Cobb angle in idiopathic scoliosis: a systematic review. Eur Spine J 22:2360–2371. https://doi.org/10.1007/s00586-013-2693-9
Kim Y, Kim D (2009) A fully automatic vertebra segmentation method using 3D deformable fences. Comput Med Imaging Graph 33:343–352. https://doi.org/10.1016/j.compmedimag.2009.02.006
Wang Y, Yao J, Roth HR, et al. (2016) Multi-atlas segmentation with joint label fusion of osteoporotic vertebral compression fractures on CT. In: Proceedings of 3rd international workshop and challenge on computational methods and clinical applications for spine imaging - CSI 2015. Springer, Munich, Germany, pp 74–84
Yao J, Burns JE, Forsberg D et al (2016) A multi-center milestone study of clinical vertebral CT segmentation. Comput Med Imaging Graph 49:16–28. https://doi.org/10.1016/j.compmedimag.2015.12.006
Korez R, Ibragimov B, Likar B et al (2015) A framework for automated spine and vertebrae interpolation-based detection and model-based segmentation. IEEE Trans Med Imaging 34:1649–1662. https://doi.org/10.1109/TMI.2015.2389334
Zheng G, Chu C, Belavý DL et al (2017) Evaluation and comparison of 3D intervertebral disc localization and segmentation methods for 3D T2 MR data: a grand challenge. Med Image Anal 35:327–344. https://doi.org/10.1016/j.media.2016.08.005
Engelke K, Stampa B, Steiger P et al (2019) Automated quantitative morphometry of vertebral heights on spinal radiographs: comparison of a clinical workflow tool with standard 6-point morphometry. Arch Osteoporos 14:18. https://doi.org/10.1007/s11657-019-0577-2
Franchini R, Conversano F, Pisani P et al (2016) Automatic method for vertebral morphometry measurements. IET Sci Meas Technol 10:327–334. https://doi.org/10.1049/iet-smt.2015.0172
Sun Y, Xing Y, Zhao Z et al (2021) Comparison of manual versus automated measurement of Cobb angle in idiopathic scoliosis based on a deep learning keypoint detection technology. Eur Spine J. https://doi.org/10.1007/s00586-021-07025-6
Bernstein P, Metzler J, Weinzierl M et al (2021) Radiographic scoliosis angle estimation: spline-based measurement reveals superior reliability compared to traditional COBB method. Eur Spine J 30:676–685. https://doi.org/10.1007/s00586-020-06577-3
Prost M, Windolf J, Konieczny MR (2021) May bending radiographs be replaced by recumbent CT scans in patients with adolescent idiopathic scoliosis? Eur Spine J 30:3490–3497. https://doi.org/10.1007/s00586-021-06945-7
Acknowledgements
This research was financially supported by the Analytical Center for the Government of the Russian Federation (Agreement No. 70-2021-00143 01.11.2021). The funding sources did not influence this investigation or affect the outcomes and results.
Funding
Analytical Center for the Government of the Russian Federation, 70-2021-00143 01.11.2021, Bulat Ibragimov
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alukaev, D., Kiselev, S., Mustafaev, T. et al. A deep learning framework for vertebral morphometry and Cobb angle measurement with external validation. Eur Spine J 31, 2115–2124 (2022). https://doi.org/10.1007/s00586-022-07245-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07245-4