Abstract
Purpose
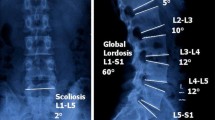
We investigated the flexion–extension range of motion and centre of rotation of lumbar motion segments in a large population of 602 patients (3612 levels), and the associations between lumbar motion and other parameters such as sex, age and intervertebral disc degeneration.
Methods
Lumbar radiographs in flexion–extension of 602 patients suffering from low back pain and/or suspect instability were collected; magnetic resonance images were retrieved and used to score the degree of disc degeneration for a subgroup of 354 patients. Range of motion and centre of rotation were calculated for all lumbosacral levels with in-house software allowing for high degree of automation. Associations between motion parameters and age, sex, spinal level and disc degeneration were then assessed.
Results
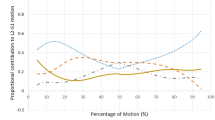
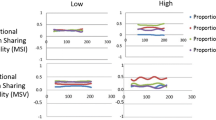
The median range of motion was 6.6° (range 0.1–28.9°). Associations between range of motion and age as well as spinal level, but not sex, were found. Disc degeneration determined a consistent reduction in the range of motion. The centre of rotation was most commonly located at the centre of the lower endplate or slightly lower. With progressive degeneration, centres of rotation were increasingly dispersed with no preferential directions.
Conclusion
This study constitutes the largest analysis of the in vivo lumbar motion currently available and covers a wide range of clinical scenarios in terms of age and degeneration. Findings confirmed that ageing determines a reduction in the mobility independently of degeneration and that in degenerative levels, centres of rotation are dispersed around the centre of the intervertebral space.






Similar content being viewed by others
Code availability
The code used to calculate the motion parameters is confidential.
References
Cossette JW, Farfan HF, Robertson GH, Wells RV (1971) The instantaneous center of rotation of the third lumbar intervertebral joint. J Biomech 4:149–153. https://doi.org/10.1016/0021-9290(71)90025-x
Gertzbein SD, Holtby R, Tile M, Kapasouri A, Chan KW, Cruickshank B (1984) Determination of a locus of instantaneous centers of rotation of the lumbar disc by moiré fringes. A new technique Spine 9:409–413. https://doi.org/10.1097/00007632-198405000-00015
Yamamoto I, Panjabi MM, Crisco T, Oxland T (1989) Three-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine 14:1256–1260. https://doi.org/10.1097/00007632-198911000-00020
Negrini S, Piovanelli B, Amici C, Cappellini V, Bovi G, Ferrarin M, Zaina F, Borboni A (2016) Trunk motion analysis: a systematic review from a clinical and methodological perspective. Eur J Phys Rehabil Med 52:583–592
Rohlmann A, Consmüller T, Dreischarf M, Bashkuev M, Disch A, Pries E, Duda GN, Schmidt H (2014) Measurement of the number of lumbar spinal movements in the sagittal plane in a 24-hour period. Eur Spine J 23:2375–2384. https://doi.org/10.1007/s00586-014-3588-0
Andreoni G, Negrini S, Ciavarro GL, Santambrogio GC (2005) ZooMS: a non invasive analysis of global and metameric movement of the lumbar spine. Eura Medicophys 41:7–16
Dreischarf M, Albiol L, Rohlmann A, Pries E, Bashkuev M, Zander T, Duda G, Druschel C, Strube P, Putzier M, Schmidt H (2014) Age-related loss of lumbar spinal lordosis and mobility–a study of 323 asymptomatic volunteers. PLoS ONE 9:e116186. https://doi.org/10.1371/journal.pone.0116186
Dvořák J, Vajda EG, Grob D, Panjabi MM (1995) Normal motion of the lumbar spine as related to age and gender. Eur Spine J 4:18–23. https://doi.org/10.1007/BF00298413
McGregor AH, McCarthy ID, Hughes SP (1995) Motion characteristics of the lumbar spine in the normal population. Spine 20:2421–2428. https://doi.org/10.1097/00007632-199511001-00009
Lee S-W, Wong KWN, Chan M-K, Yeung H-M, Chiu JLF, Leong JCY (2002) Development and validation of a new technique for assessing lumbar spine motion. Spine 27:E215–E220. https://doi.org/10.1097/00007632-200204150-00022
Stucovitz E, Vitale J, Galbusera F (2018) In Vivo Measurements: Motion Analysis. In: Biomechanics of the Spine. Elsevier, pp 189–201
Bakke S (1931) Rontgenologische beobachtungen uber die bewegungen der halswirbelsaule. Acta Radiol Suppl 13:76
Wiles P (1935) Movements of the Lumbar Vertebræ during Flexion and Extension: (Section of Orthopædics). Proc R Soc Med 28:647–651
Tanz SS (1953) Motion of the lumbar spine; a roentgenologic study. Am J Roentgenol Radium Ther Nucl Med 69:399–412
Pennal GF, Conn GS, McDonald G, Dale G, Garside H (1972) Motion studies of the lumbar spine: a preliminary report. J Bone Joint Surg Br 54:442–452
Frobin W, Brinckmann P, Biggemann M, Tillotson M, Burton K (1997) Precision measurement of disc height, vertebral height and sagittal plane displacement from lateral radiographic views of the lumbar spine. Clin Biomech 12(Suppl 1):S1–S63. https://doi.org/10.1016/s0268-0033(96)00067-8
Morgan FP, King T (1957) Primary instability of lumbar vertebrae as a common cause of low back pain. J Bone Joint Surg Br 39-B:6–22
Knutsson F (1944) The Instability Associated with Disk Degeneration in the Lumbar Spine. Acta Radiol 25:593–609
Dvorak J, Panjabi MM, Novotny JE, Chang DG, Grob D (1991) Clinical Validation of Functional Flexion-Extension Roentgenograms of the Lumbar Spine. SPINE 16:943–950
Dvořák J, Panjabi MM, Chang DG, Theiler R, Grob D (1991) Functional Radiographic Diagnosis of the Lumbar Spine. Spine 16:562–571
Pearcy MJ (1985) Stereo radiography of lumbar spine motion. Acta Orthop Scand Suppl 212:1–45. https://doi.org/10.3109/17453678509154154
Pearcy MJ, Tibrewal SB (1984) Axial rotation and lateral bending in the normal lumbar spine measured by three-dimensional radiography. Spine 9:582–587. https://doi.org/10.1097/00007632-198409000-00008
Wong KWN, Leong JCY, Chan M-K, Luk KDK, Lu WW (2004) The Flexion-Extension Profile of Lumbar Spine in 100 Healthy Volunteers. Spine 29:1636. https://doi.org/10.1097/01.BRS.0000132320.39297.6C
Staub BN, Holman PJ, Reitman CA, Hipp J (2015) Sagittal plane lumbar intervertebral motion during seated flexion-extension radiographs of 658 asymptomatic nondegenerated levels. J Neurosurg Spine 23:731–738. https://doi.org/10.3171/2015.3.SPINE14898
Panjabi M, Chang D, Dvorák J (1992) An analysis of errors in kinematic parameters associated with in vivo functional radiographs. Spine 17:200–205. https://doi.org/10.1097/00007632-199202000-00014
Wilke H-J, Rohlmann F, Neidlinger-Wilke C, Werner K, Claes L, Kettler A (2006) Validity and interobserver agreement of a new radiographic grading system for intervertebral disc degeneration: Part I. Lumbar spine Eur Spine J 15:720–730. https://doi.org/10.1007/s00586-005-1029-9
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26:1873–1878. https://doi.org/10.1097/00007632-200109010-00011
Hua C (1990) An inverse transformation for quadrilateral isoparametric elements: Analysis and application. Finite Elem Anal Des 7:159–166. https://doi.org/10.1016/0168-874X(90)90007-2
Wilke HJ, Rohlmann A, Neller S, Schultheiss M, Bergmann G, Graichen F, Claes LE (2001) Is it possible to simulate physiologic loading conditions by applying pure moments? A comparison of in vivo and in vitro load components in an internal fixator. Spine 26:636–642. https://doi.org/10.1097/00007632-200103150-00014
Kettler A, Rohlmann F, Ring C, Mack C, Wilke H-J (2011) Do early stages of lumbar intervertebral disc degeneration really cause instability? Evaluation of an in vitro database. Eur Spine J 20:578–584. https://doi.org/10.1007/s00586-010-1635-z
Mimura M, Panjabi MM, Oxland TR, Crisco JJ, Yamamoto I, Vasavada A (1994) Disc degeneration affects the multidirectional flexibility of the lumbar spine. Spine 19:1371–1380. https://doi.org/10.1097/00007632-199406000-00011
Schneider G, Pearcy MJ, Bogduk N (2005) Abnormal motion in spondylolytic spondylolisthesis. Spine 30:1159–1164. https://doi.org/10.1097/01.brs.0000162400.06685.37
Aiyangar A, Zheng L, Anderst W, Zhang X (2017) Instantaneous centers of rotation for lumbar segmental extension in vivo. J Biomech 52:113–121. https://doi.org/10.1016/j.jbiomech.2016.12.021
White AA, Panjabi MM Clinical biomechanics of the spine (1990) Philadelphia. PA, USA Lippincott
Boos N, Aebi M (2008) Spinal disorders: fundamentals of diagnosis and treatment. Springer
Gertzbein SD, Seligman J, Holtby R, Chan KH, Kapasouri A, Tile M, Cruickshank B (1985) Centrode patterns and segmental instability in degenerative disc disease. Spine 10:257–261. https://doi.org/10.1097/00007632-198504000-00014
Rousseau M-A, Bradford DS, Hadi TM, Pedersen KL, Lotz JC (2006) The instant axis of rotation influences facet forces at L5/S1 during flexion/extension and lateral bending. Eur Spine J 15:299–307. https://doi.org/10.1007/s00586-005-0935-1
Patwardhan A, Wharton N, Lorenz M, Havey R, Carandang G, Patrick O, ’leary, Nicolakis M, Voronov L, Zindrick M, Hipp J, Ghanayem A, (2006) P35. Location and Mobility of Instantaneous Centers of Rotation in the Lumbar Spine – Implications to Design of Lumbar Disc Prostheses. The Spine Journal 6:100S-101S
Schmidt H, Heuer F, Claes L, Wilke H-J (2008) The relation between the instantaneous center of rotation and facet joint forces – A finite element analysis. Clin Biomech 23:270–278
Alapan Y, Demir C, Kaner T, Guclu R, Inceoğlu S (2013) Instantaneous center of rotation behavior of the lumbar spine with ligament failure. J Neurosurg Spine 18:617–626. https://doi.org/10.3171/2013.3.SPINE12923
Ogston NG, King GJ, Gertzbein SD, Tile M, Kapasouri A, Rubenstein JD (1986) Centrode patterns in the lumbar spine. Baseline studies in normal subjects Spine 11:591–595. https://doi.org/10.1097/00007632-198607000-00010
Haher TR, Bergman M, O’Brien M, Felmly WT, Choueka J, Welin D, Chow G, Vassiliou A (1991) The effect of the three columns of the spine on the instantaneous axis of rotation in flexion and extension. Spine 16:S312–S318
Schmidt H, Heuer F, Wilke H-J (2008) Interaction between finite helical axes and facet joint forces under combined loading. Spine 33:2741–2748. https://doi.org/10.1097/BRS.0b013e31817c4319
Bashkuev M, Reitmaier S, Schmidt H (2019) Relationship between intervertebral disc and facet joint degeneration: A probabilistic finite element model study. J Biomech. https://doi.org/10.1016/j.jbiomech.2019.109518
Cui JH, Kim Y-C, Lee K, Park G-T, Kim K-T, Kim SM (2019) Relationship between facet joint tropism and degeneration of facet joints and intervertebral discs based on a histological study. Journal of Orthopaedics 16:123–127
Rousseau M-A, Bradford DS, Bertagnoli R, Hu SS, Lotz JC (2006) Disc arthroplasty design influences intervertebral kinematics and facet forces. Spine J 6:258–266. https://doi.org/10.1016/j.spinee.2005.07.004
Byrne RM, Aiyangar AK, Zhang X (2019) A Dynamic Radiographic Imaging Study of Lumbar Intervertebral Disc Morphometry and Deformation In Vivo. Sci Rep 9:15490. https://doi.org/10.1038/s41598-019-51871-w
Wattananon P, Intawachirarat N, Cannella M, Sung W, Silfies SP (2018) Reduced instantaneous center of rotation movement in patients with low back pain. Eur Spine J 27:154–162. https://doi.org/10.1007/s00586-017-5054-2
Wawrose RA, LeVasseur CM, Byrapogu VK, Dombrowski ME, Donaldson WF, Shaw JD, Lee JY, Anderst WJ, Aiyangar AK (2020) In vivo changes in adjacent segment kinematics after lumbar decompression and fusion. J Biomech 102:109515. https://doi.org/10.1016/j.jbiomech.2019.109515
Funding
The study was partially supported by the Italian Ministry of Health ("Ricerca Corrente").
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethics approval
The study has been approved by the Ethics Committee of Ulm University (no. 50/20).
Consent to participate
All patients provided informed consent for the use of anonymized data for scientific and educational purposes.
Consent for publication
All patients provided informed consent for the use of anonymized data in scientific publications.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Galbusera, F., Niemeyer, F., Tao, Y. et al. ISSLS Prize in Bioengineering Science 2021: in vivo sagittal motion of the lumbar spine in low back pain patients—a radiological big data study. Eur Spine J 30, 1108–1116 (2021). https://doi.org/10.1007/s00586-021-06729-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06729-z