Abstract
Purpose
The relationship between biomechanical instability and degenerative changes in the lumbar spine in chronic low back pain (CLBP) patients remains controversial. The main objective of this retrospective radiographical study was to evaluate changes in kinematics at different lumbar levels (in particular the L5–S1 level) with progressive grades of disc degeneration and facet joint osteoarthritis in CLBP patients.
Methods
Using standing neutral and dynamic flexion/extension (Fx/Ex) radiographs of the lumbar spine, in vivo segmental kinematics at L1–L2 through L5–S1 were evaluated in 72 consecutive CLBP patients. Disc degeneration was quantified using changes in signal intensity and central disc height on mid-sagittal T2-weighted magnetic resonance (MR) scans. Additionally, the presence or absence of facet joint osteoarthritis was noted on T2-weighted axial MR scans.
Results
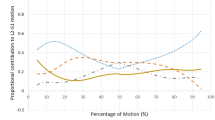
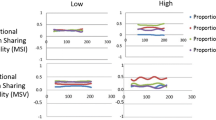
Disc degeneration and facet joint osteoarthritis occurred independent of each other at the L5–S1 level (p = 0.188), but an association was observed between the two at L4–L5 (p < 0.001) and L3–L4 (p < 0.05) levels. In the absence of facet joint osteoarthritis, the L5–S1 segment showed a greater range of motion (ROM) in Ex (3.3° ± 3.6°) and a smaller ROM in Fx (0.6° ± 4.2°) compared with the upper lumbar levels (p < 0.05), but the differences diminished in the presence of it. In the absence of facet joint osteoarthritis, no change in L5–S1 kinematics was observed with progressive disc degeneration, but in its presence, restabilisation of the L5–S1 segment was observed between mild and severe disc degeneration states.
Conclusion
The L5–S1 motion segment exhibited unique degenerative and kinematic characteristics compared with the upper lumbar motion segments. Disc degeneration and facet joint osteoarthritis occurred independent of each other at the L5–S1 level, but not at the other lumbar levels. Severe disc degeneration in the presence of facet joint osteoarthritis biomechanically restabilised the L5–S1 motion segment.


Similar content being viewed by others
References
Kirkaldy-Willis WH, Farfan HF (1982) Instability of the lumbar spine. Clin Orthop Relat Res 165:110–123
Fujiwara A, Lim TH, An HS, Tanaka N, Jeon CH, Andersson GB, Haughton VM (2000) The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine 25:3036–3044
Tanaka N, An HS, Lim TH, Fujiwara A, Jeon CH, Haughton VM (2001) The relationship between disc degeneration and flexibility of the lumbar spine. Spine J 1:47–56
Oxland TR, Lund T, Jost B, Cripton P, Lippuner K, Jaeger P, Nolte LP (1996) The relative importance of vertebral bone density and disc degeneration in spinal flexibility and interbody implant performance. An in vitro study. Spine 21:2558–2569
Kettler A, Rohlmann F, Ring C, Mack C, Wilke HJ (2011) Do early stages of lumbar intervertebral disc degeneration really cause instability? Evaluation of an in vitro database. Eur Spine J 20:578–584
Boden SD, Wiesel SW (1990) Lumbosacral segmental motion in normal individuals. Have we been measuring instability properly? Spine 15:571–576
Hayes MA, Howard TC, Gruel CR, Kopta JA (1989) Roentgenographic evaluation of lumbar spine flexion–extension in asymptomatic individuals. Spine 14:327–331
Pearcy M, Portek I, Shepherd J (1984) Three-dimensional X-ray analysis of normal movement in the lumbar spine. Spine 9:294–297
Kanayama M, Abumi K, Kaneda K, Tadano S, Ukai T (1996) Phase lag of the intersegmental motion in flexion–extension of the lumbar and lumbosacral spine. An in vivo study. Spine 21:1416–1422
Bali T, Kumar MN (2015) Relative contribution of upper and lower lumbar spinal segments to flexion/extension: comparison between normal spines and spines with disc disease in Asian patients. Asian Spine J 9:770–775
Li G, Wang S, Passias P, Xia Q, Li G, Wood K (2009) Segmental in vivo vertebral motion during functional human lumbar spine activities. Eur Spine J 18:1013–1021
Passias PG, Wang S, Kozanek M, Xia Q, Li W, Grottkau B, Wood KB, Li G (2011) Segmental lumbar rotation in patients with discogenic low back pain during functional weight-bearing activities. J Bone Jt Surg Am 93:29–37
Aiyangar A, Zheng L, Anderst W, Zhang X (2015) Apportionment of lumbar L2–S1 rotation across individual motion segments during a dynamic lifting task. J Biomech 48:3718–3724
Wong KWN, Leong JCY, M-k Chan, Luk KDK, Lu WW (2004) The flexion–extension profile of lumbar spine in 100 healthy volunteers. Spine 29:1636–1641
Harada M, Abumi K, Ito M, Kaneda K (2000) Cineradiographic motion analysis of normal lumbar spine during forward and backward flexion. Spine 25:1932–1937
Wong KW, Luk KD, Leong JC, Wong SF, Wong KK (2006) Continuous dynamic spinal motion analysis. Spine 31:414–419
Pearcy M, Portek I, Shepherd J (1985) The effect of low-back pain on lumbar spinal movements measured by three-dimensional X-ray analysis. Spine 10:150–153
Davis Richard A (1994) A long-term outcome analysis of 984 surgically treated herniated lumbar discs. J Neurosurg 80:415–421
Weinstein JN, Tosteson TD, Lurie JD et al (2006) Surgical vs nonoperative treatment for lumbar disk herniation: the spine patient outcomes research trial (sport): a randomized trial. JAMA 296:2441–2450
Weinstein JN, Lurie JD, Tosteson TD, Hanscom B, Tosteson ANA, Blood EA, Birkmeyer NJO, Hilibrand AS, Herkowitz H, Cammisa FP, Albert TJ, Emery SE, Lenke LG, Abdu WA, Longley M, Errico TJ, Hu SS (2007) Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med 356:2257–2270
Hicks GE, George SZ, Nevitt MA, Cauley JA, Vogt MT (2006) Measurement of lumbar lordosis: inter-rater reliability, minimum detectable change and longitudinal variation. J Spinal Disord Tech 19:501–506
Rihn JA, Lee JY, Khan M, Ulibarri JA, Tannoury C, Donaldson WF 3rd, Kang JD (2007) Does lumbar facet fluid detected on magnetic resonance imaging correlate with radiographic instability in patients with degenerative lumbar disease? Spine 32:1555–1560
Schellinger D, Wener L, Ragsdale BD, Patronas NJ (1987) Facet joint disorders and their role in the production of back pain and sciatica. Radiographics 7:923–944
Caterini R, Mancini F, Bisicchia S, Maglione P, Farsetti P (2011) The correlation between exaggerated fluid in lumbar facet joints and degenerative spondylolisthesis: prospective study of 52 patients. J Orthop Traumatol 12:87–91
Butler D, Trafimow JH, Andersson GB, McNeill TW, Huckman MS (1990) Discs degenerate before facets. Spine 15:111–113
Fujiwara A, Tamai K, Yamato M, An HS, Yoshida H, Saotome K, Kurihashi A (1999) The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J 8:396–401
Videman T, Battie MC, Gill K, Manninen H, Gibbons LE, Fisher LD (1995) Magnetic resonance imaging findings and their relationships in the thoracic and lumbar spine. Insights into the etiopathogenesis of spinal degeneration. Spine 20:928–935
Luk K, Ho H, Leong J (1986) The iliolumbar ligament. A study of its anatomy, development and clinical significance. J Bone Jt Surg (British Volume) 68-B:197–200
Leong JCY, Luk KDK, Chow DHK, Woo CW (1987) The biomechanical functions of the iliolumbar ligament in maintaining stability of the lumbosacral junction. Spine 12:669–674
Acknowledgements
The authors thank George Assaad, Leo Ho, Ifrah Zubair and Nerida Grewal for their help with data collection. This work was supported by internal research funds from Spine Service.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest related to this work.
Rights and permissions
About this article
Cite this article
Sabnis, A.B., Chamoli, U. & Diwan, A.D. Is L5–S1 motion segment different from the rest? A radiographic kinematic assessment of 72 patients with chronic low back pain. Eur Spine J 27, 1127–1135 (2018). https://doi.org/10.1007/s00586-017-5400-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5400-4