Abstract
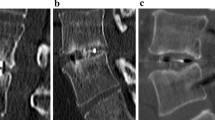
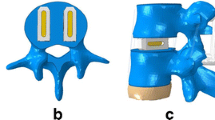
Chronic lumbar pain due to degenerative disc disease affects a large number of people, including those of fully active age. The usual self-repair system observed in nature is a spontaneous attempt at arthrodesis, which in most cases leads to pseudoarthrosis. In recent years, many possible surgical fusion techniques have been introduced; PLIF is one of these. Because of the growing interest in minimally invasive surgery and the unsatisfactory results reported in the literature (mainly due to the high incidence of morbidity and complications), a new titanium lumbar interbody cage (I-FLY) has been developed to achieve solid bone fusion by means of a stand-alone posterior device. The head of the cage is blunt and tapered so that it can be used as a blunt spreader, and the core is small, which facilitates self-positioning. From 2003 to 2007, 119 patients were treated for chronic lumbar discopathy (Modic grade III and Pfirrmann grade V) with I-FLY cages used as stand-alone devices. All patients were clinically evaluated preoperatively and after 1 and 2 years by means of a neurological examination, visual analogue score (VAS) and Prolo Economic and Functional Scale. Radiological results were evaluated by polyaxial computed tomography (CT) scan and flexion–extension radiography. Fusion was defined as the absence of segmental instability on flexion–extension radiography and Bridwell grade I or II on CT scan. Patients were considered clinical “responders” if VAS evaluation showed any improvement over baseline values and a Prolo value >7 was recorded. At the last follow-up examination, clinical success was deemed to have been achieved in 90.5% of patients; the rate of bone fusion was 99.1%, as evaluated by flexion–extension radiography, and 92.2%, as evaluated by CT scan. Morbidity (nerve root injury, dural lesions) and complications (subsidence and pseudoarthrosis) were minimal. PLIF by means of the stand-alone I-FLY cage can be regarded as a possible surgical treatment for chronic low-back pain due to high-degree DDD. This technique is not demanding and can be considered safe and effective, as shown by the excellent clinical and radiological success rates.




Similar content being viewed by others
References
Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR (1988) Degenerative disc disease: assessment of changes in vertebral body marrow with MRI Imaging. Radiology 166:194–199
Pfirrmann CWA, Matzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 17:1873–1878
Ross JS, Modic MT (1992) Current assessment of spinal degenerative disease with magnetic resonance imaging. Clin Orthop Relat Res. 279:68–81
Vaga S, Raimondi MT, Caiani EG, Costa F, Giordano C, Perona F et al (2008) Quantitative assessment of intervertebral disc glycosaminoglycan distribution by gadolinium-enhanced MRI in orthopedic patients. Magn Reson Med 59(1):85–95
Cloward RB (1953) The treatment of ruptured lumbar intervertebral discs by vertebral body fusion I. Indications, operative technique, after care. J Neurosurg 10(2):154–168
Branch CL, Branch CL Jr (1987) Posterior lumbar interbody fusion with the keystone graft: technique and results. Surg Neurol 27:449–454
Brantigan JW, Steffee AD, Geiger JM (1991) A carbon fiber implant to aid interbody lumbar fusion. Mechanical testing. Spine 16:S277–S282
Ray CD (1997) Threaded titanium cages for lumbar interbody fusions. Spine. 22:667–679 (discussion 79–80)
Simmons JW (1985) Posterior lumbar interbody fusion with posterior elements as chip grafts. Clin Orthop Relat Res. 193:85–89
Cole CD, McCall TD, Schmidt MH, Dailey AT (2009) Comparison of low back fusion techniques: transforaminal lumbar interbody fusion (TLIF) or posterior lumbar interbody fusion (PLIF) approaches. Curr Rev Musculoskelet Med 2(2):118–126
Krishna M, Pollock RD, Bhatia C (2008) Incidence, etiology, classification, and management of neuralgia after posterior lumbar interbody fusion surgery in 226 patients. Spine J. 8:374–379
Sears W (2005) Posterior lumbar interbody fusion for degenerative spondylolisthesis: restoration of sagittal balance using insert-and rotate interbody spacers. Spine J. 5:170–179
Freeman BJ, Davenport J (2006). Total disc replacement in the lumbar spine: a systematic review of the literature. Eur Spine J 15(Suppl 3):S439–S447
Blumenthal S, McAfee PC, Guyer RD, Hochschuler SH, Geisler FH, Holt RT et al (2005) A prospective, randomised multi-centre food and drug administration investigational device exemption study of lumbar total disc replacement with the Charite′ artificial disc versus lumbar fusion. Part I: evaluation of clinical outcomes. Spine 30:1565–1575 (discussion E387–E391) (erratum in Spine 2005 Oct 15;30(20):2356)
Geisler FH, Blumenthal SL, Guyer RD, McAfee PC, Regan JJ, Johnson JP et al (2004) Neurological complications of lumbar artificial disc replacement and comparison of clinical results with those related to lumbar arthrodesis in the literature: results of a multicentre, prospective, randomized investigational device exemption study of Charite intervertebral disc. J Neurosurg (Spine) 1:143–154
Guyer RD, McAfee PC, Banco RJ, Bitan FD, Cappuccino A, Geisler FH et al (2009) Prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: five-year follow-up. Spine J 9(5):374–386
Bono CM, Vaccaro AR (2007) Interspinous process devices in the lumbar spine. J Spinal Disord Tech. 20(3):255–261
AN MOR (1948) The meaning and measurement of pain. Practitioner 160(956):136–144
Prolo DJ, Oklund SA, Butcher M (1986) Toward uniformity in evaluating results of lumbar spine operations. A paradigm applied to posterior lumbar interbody fusions. Spine 11(6):601–606
Resnick DK, Choudhri TF, Dailey AT, Groff MW, Khoo L, Matz PG et al (2005) Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 4: radiographic assessment of fusion. J Neurosurg Spine 2(6):653–657
Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K (1995) Anterior structural allografts in the thoracic and lumbar spine. Spine 20:1410–1418
Amonoo Kuofi HS (1982) Maximum and minimum interpedicular distances in normal adult Nigerians. Am J Anat 135:225–233
Amonoo Kuofi HS, Patel PJ, Fatani JA (1990) Transverse diameter of the lumbar spinal canal in normal adult Saudis. Acta Anat 137:124–128
Chhabra S, Gopinathan K, Chhibber SR (1991) Transverse diameter of the lumbar vertebral canal in North Indians. J. Anat. Soc India Vol 41(1):25–32
Hinck VC, Clark WM, Hopkins CE (1966) Normal interpediculate distances (minimum and maximum) in children and adults. Am. J. Roentgnol. 97:141–153
Zdeblick TA (1995) The treatment of degenerative lumbar disorders. A critical review of the literature. Spine 20:126S–137S
Cristoferson LA, Selland B (1975) Intervertebral implants following excision of protruded lumbar discs. J Neurosurg 42:401–405
Hacker RJ (1997) Comparison of interbody fusion approaches for disabling low back pain. Spine 22:660–666
Kim Y (2001) Prediction of mechanical behaviors at interfaces between bone and two interbody cages of lumbar spine segments. Spine 26:1437–1442
Steffen T, Tsantrizos A, Aebi M (2000) Effect of implant design and endplate preparation on the compressive strength of interbody fusion constructs. Spine 25:1077–1084
Barnes B, Rodts GE, McLaughlin MR, Haid RW Jr (2001) Threaded cortical bone dowels for lumbar interbody fusion: over 1-year follow-up in 28 patients. J Neurosurg 95:1–4
Hee HT, Castro FP Jr, Majd ME, Holt RT, Myers L (2001) Anterior/posterior lumbar fusion versus transforaminal lumbar interbody fusion: analysis of complications and predictive factors. J Spinal Disord 14:533–540
Chen L, Yang H, Tang T (2005) Cage migration in spondylolisthesis treated with posterior lumbar interbody fusion using BAK cages. Spine 30(19):2171–2175
Brantigan JW, Steffee DA, Lewis ML, Quinn LM, Persenaire JM (2000) Lumbar interbody fusion using the Bratigan I/F cage for posterior lumbar interbody fusion and the variable pedicle screw placement system. Spine 25:1437–1446
Kuslich SD, Ulstrom CL, Griffith SL, Ahern JW, Dowdle JD (1998) The Bagby and Kuslich method of lumbar interbody fusion. History, techniques, and 2-year follow-up results of a United States prospective, multicenter trial. Spine Jun 1; 23 (11):1267–1278 (discussion 1279) [comment in Spine 1999 Sep 1; 24(17):1857]
Brislin B, Vaccaro AR (2002) Advances in posterior lumbar interbody fusion. Orthop Clin N Am 33(2):367–374
DiPaola CP, Molinari RW (2008) Posterior lumbar interbody fusion. J Am Acad Orthop Surg. 16(3):130–139
Fantigrossi A, Galbusera F, Raimondi MT, Sassi M, Fornari M (2007) Biomechanical analysis of cages for posterior lumbar interbody fusion. Med Eng Phys 29(1):101–109
Vishteh AG, Crawford NR, Chamberlain RH, Thramann JJ, Park SC, Craigo JB et al (2005) Biomechanical comparison of anterior versus posterior lumbar threaded interbody fusion cages. Spine. Feb 1; 30 (3):302–310
Weiner BK, Fraser RD (1998) Spine update lumbar interbody cages. Spine 23(5):634–640
Piera V, Rodroguez A, Cobos A, Hernandez R, Cobos P (1988) Morphology of lumbar vertebral canal. Acta Anat 131:25–40
Elias WJ, Simmons NE, Kaptain GJ, Chadduck JB, Whitehill R (2000) Complications of posterior lumbar interbody fusion when using a titanium threaded cage device. J Neurosurg 93:45–52
Freeman BJC, Licina P, Mehdian SH (2000) Posterior lumbar interbody fusion combined with instrumented postero-lateral fusion: 5-year results in 60 patients. Eur Spine J 9:42–46
Vamvanij V, Fredrickson BE, Thorpe JM, Stadnick ME, Yuan HA (1998) Surgical treatment of internal disc disruption: an outcome study of four fusion techniques. J Spinal Disord 11(5):375–382
Resnick DK, Choudhri TF, Dailey AT, Groff MW, Khoo L, Matz PG et al (2005) Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 11: interbody techniques for lumbar fusion. J Neurosurg Spine 2 (6):692–699
Brodsky AE, Kovalsky ES, Khalil MA (1991) Correlation of radiologic assessment of lumbar spine fusions with surgical exploration. Spine Jun; 16(6 Suppl):S261–S265
Burkus JK, Dorchak JD, Sanders DL (2003). Radiographic assessment of interbody fusion using recombinant human bone morphogenetic protein type 2. Spine. Feb 15; 28(4):372–377
Cleveland M, Bosworth DM, Thompson FR (1948) Pseudarthrosis in the lumbosacral spine. J Bone Jt Surg Am 30A(2):302–312
Lang P, Genant HK, Chafetz N, Steiger P, Morris JM (1998) Three-dimensional computed tomography and multiplanar reformations in the assessment of pseudarthrosis in posterior lumbar fusion patients. Spine 13(1):69–75
Shah RR, Mohammed S, Saifuddin A, Taylor BA (2003) Comparison of plain radiographs with CT scan to evaluate interbody fusion following the use of titanium interbody cages and transpedicular instrumentation. Eur Spine J Aug; 12(4):378–385
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Costa, F., Sassi, M., Ortolina, A. et al. Stand-alone cage for posterior lumbar interbody fusion in the treatment of high-degree degenerative disc disease: design of a new device for an “old” technique. A prospective study on a series of 116 patients. Eur Spine J 20 (Suppl 1), 46–56 (2011). https://doi.org/10.1007/s00586-011-1755-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-011-1755-0