Abstract
Purpose
ALIF with cages is expected to restore disc height and stabilize the spine promoting fusion, while avoiding damage attributed to rod-pedicle screw fixation. However, it may be related to an increased risk of fusion failure and subsidence. A prospective study was conducted by five investigators across three centers to confirm performance of a PEEK cage for stand-alone ALIF in the treatment of lumbar degenerative disc disease (DDD).
Methods
Sixty-five patients, with back ± leg pain, requiring surgery for DDD, were included. Efficacy and safety were evaluated at 6 weeks, 3, 6, and 12 months post-operatively. Fusion and subsidence were assessed through CT-images at 12-month follow-up. Disc height was measured. Clinical outcomes included back and leg pain (VAS), disability (Oswestry Disability Index), Quality of Life (Short-Form 36), and adverse events.
Results
The fusion and the subsidence rates were 96.3 and 2.0 %, respectively. ALIF surgery restored anterior and posterior disc height compared to baseline. There were no device-related serious adverse events, and no revision surgeries. Clinical outcomes improved significantly through 12-month follow-up.
Conclusion
Safety and efficacy of this stand-alone cage with integrated intracorporeal plates was confirmed through 12 months for treatment of degenerative conditions. The design of the cage and plates may contribute to the decreased subsidence rate observed.
Similar content being viewed by others
Introduction
Among the various fusion techniques dedicated to surgically treat lumbar Degenerative Disc Disease (DDD), Anterior Lumbar Interbody Fusion (ALIF) with cage has been extensively used since introduced by Bagby in 1988 [1]. Reinforcement and stabilization of the anterior column of the spine, after disc removal, restores the disc height and the segmental lordosis and can have many mechanical advantages [2, 3]. Also, the anterior approach avoids posterior muscular damage [4] and neurological injuries [5]. Despite positive results [6], the stability of stand-alone cages has been questioned during the low muscular preloading phases when the cage has been suspected to be less stable [7]. The instability during the bone healing process is hypothesized to be one of the main reasons for pseudarthrosis [8–10] and subsidence [3]. Compared with stand-alone cage, supplementary fixation increases the stiffness and stability [3] and significantly improves the fusion rate [11]. The addition of rod-pedicle screw fixation increases the risk of compromising neurological and muscular elements and produces worse clinical outcomes when compared to stand-alone procedure [12] while also increasing the occurrence of adjacent disc degeneration [13]. Anterior plating has been proposed but increases blood loss and length of procedure. Furthermore, anatomical configuration in L4-L5 and L5-S1 can make it either difficult or impossible, so lower profile cages integrating anterior fixation screws were designed to facilitate these cases [10, 12, 14].
A new concept of lumbar cage integrating a zero-profile plating system has been designed and the purpose of this study was to evaluate the safety and efficacy of this system.
Population and methods
Study design
A prospective, non-interventional study has been conducted in France to evaluate the clinical efficacy and the stability of the device used for one-level ALIF procedures in the surgical treatment of DDD of the lumbar spine.
Participants
Inclusion criteria were
-
adult patient, (≥18 years of age)
-
with back ± leg pain unresponsive to appropriate conservative treatment,
-
requiring 1-level surgery for DDD with or without degenerative spondylolisthesis.
Exclusion criteria were
-
contraindication to anterior approach of the lumbar spine,
-
excluded disc herniation,
-
narrow canal requiring a posterior decompression,
-
presence of a prior posterior device at the level to be treated.
Patient enrollment began with the first implantation in September, 2007. Training cases have been included in the total 65-patient cohort. Patients were included regardless of smoking status, previous surgical history (with exception of exclusion criteria above), and work-related injuries. Five investigators from three centers were responsible for surgical procedures and patient follow-up.
According to French regulation, each patient was appropriately informed of his/her freedom to decline or agree to participate in the study and of his rights regarding medical data collection.
Surgical technique
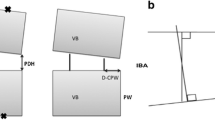
ROI-A® (LDR Médical, Troyes, France) is an intersomatic Polyetheretherketone (PEEK) cage for ALIF, which includes an integrated supplemental fixation system—the intracorporeal locking system (VerteBRIDGE®) eliminates the need for additional fixation, such as anterior plate or pedicular screws (Fig. 1), in appropriate patients.
The anterior approach was either midline or anterolateral retroperitoneal according to the operated level. After the discectomy, endplate cartilage was removed with usual precautions and proper implant size was determined using the trial implants under fluoroscopy. In case of narrow disc space, the distraction was performed using a parallel distractor. Particular attention was placed to endplate preparation, which was achieved using a straight curette, as shavers were prohibited. An adjacent healthy disc was examined to obtain sagittal balance, and heights (anterior and posterior) to ensure optimal cage contact with both vertebral endplates. Once the proper cage was selected, filled with the bone grafting material (at the surgeon’s discretion), it was inserted into the intervertebral space using fluoroscopy. Once the position of the cage was optimal, the anchoring plate (composed of two self-guided half-anchoring plates) was impacted. The half-anchoring plates were inserted one-by-one under fluoroscopy. Post-operative care was at the discretion of the surgeon.
Outcomes
Each patient was followed-up prospectively with pre-operative and post-operative evaluations (6 weeks, 3, 6, 12 months). The study is ongoing, and follow-up is planned for up to 10 years.
Primary clinical outcomes
The primary outcome was fusion rate, evaluated at the best from Computed Tomography (CT) images at 12-month follow-up using sagittal and coronary plane reconstructions [15]. The CT-reconstructions were evaluated by the principal investigator and an orthopedic senior spine surgeon, independent of the investigator’s group and unaware of the clinical results. In case of disagreement, both readers reconsidered the images to obtain a final statement. Fusion rate was evaluated as follows:
-
acquired fusion: trabecular bone continuity between the two vertebrae within and/or out of the cage on at least one image in the sagittal and/or coronary plane.
-
Fusion failure: no trabecular bone continuity between the two vertebrae within and/or out of the cage in both planes of the CT.
-
Doubtful fusion
Secondary clinical outcomes
Usual demographics and peri-operative data were collected. Analgesic use (class and frequency) was documented pre-operatively and at each post-operative visit. Early or late complications and re-operations were monitored up to the final follow-up. Each adverse event was graded as serious (leading to death, life-threatening condition, requiring hospitalization or lengthening of hospital stay, leading to permanent or significant disability) and not serious.
At each visit, patients filled an auto-questionnaire, including Visual Analog Scale (VAS) for lumbar and leg pain (0–10 cm), the Oswestry Disability Index (ODI 0–100 %), and the Short-Form 36 (SF-36) quality of life scale.
In a self-satisfaction index, patients were asked to rate their satisfaction (Very satisfied/satisfied/not satisfied/dissatisfied) of overall result of the surgery, back and leg pain. Their willingness to undergo the operation again under the same conditions was recorded.
Secondary radiographic outcomes
The index disc height was measured anteriorly and posteriorly. Post-operative X-ray calibration/sizing was performed using the known length of each implanted plate. These index measurements were performed pre-operatively, before discharge, and at final follow-up by a single reader using the OsiriX software.
The radiographic behavior of the cage was assessed by the two readers mentioned above. The following events were systematically monitored:
-
Subsidence of the cage was defined as any violation of vertebral endplate integrity which could be visible on CT-images in sagittal and/or coronal plane, as recommended by Lee et al. [16], and assessed by comparing images on the CT-scan completed before discharge and at final follow-up.
-
Cage displacement out of the disc space was assessed by comparing cage positioning before discharge and at final follow-up from standing neutral lateral X-rays.
-
Plate mobilization, plate fracture and bony fracture were assessed by comparing standing neutral lateral X-rays before discharge and at late follow-up.
Statistical analysis
The data were analyzed using Prism 5.03 software. Comparisons between pre-op and post-op continuous variables were performed using 2-sided t tests or Wilcoxon matched-pairs signed rank tests, depending on normal distribution of the data. The MacNemar’s test was used for comparison of categorical data. The significance level was p < 0.05. All available data have been taken into account.
Results
Sixty-five patients were included and operated on between September, 2007 and November, 2010.
Baseline data
On average, the population (16 Men, 49 Women) was 57.1 ± 11.1 years old (range 35–82). 20 patients (30.8 %) were smokers, and 6 (9.2 %) had work-related injury.
Baseline data and clinical characteristics are summarized in Table 1, and intra-operative data in Table 2.
All procedures were performed with the PEEK cage and VerteBRIDGE® plates without any additional anterior or posterior fixation (stand-alone configuration).
Twelve-month follow-up was achieved by 64/65 patients (98.9 %). At the time of database lock, no deaths and no premature study endings were reported.
Fusion rate
At 12 months, 54/65 CT’s were available for fusion assessment (11 CT’s were incomplete: not performed, or with missing views).
Results indicate 52/54 levels were fused; 2/54 levels were doubtful. One was a 73-year-old male smoker with a BMI of 31.8 with autologous bone graft used. The other was a 50-year-old non-smoking male, with autologous bone and bone morphogenetic protein used. There were no fusion failures.
The fusion rate was 96.3 % (52/54 at 12-month follow-up (95 % confidence interval ranging from 86.74 to 99.70 %); Fig. 2.
Patient 1–13, anterolateral L4–L5 ROI-A®. Pre-operative neutral lateral X-ray (a) and Computed Tomography-reconstruction (b); neutral lateral X-ray (c) and Computed Tomography-reconstruction (d) performed 7 days following surgery; Computed Tomography-reconstruction at 12 months of follow-up (e) with achieved fusion
Secondary outcomes
Clinical and radiographic adverse events
Two serious adverse events were reported: one superior level reoperation by posterior approach for another lumbar spine disease and one persistent L5 paresia.
All the other adverse events were graded as “not serious”: 13 surgery-related: 12 resolved without sequelae (1 phlebitis, 2 peritoneal tears, 3 motor complications, 3 sympathetic complications, 2 sexual complications, 1 urinary complication.) and 1 sensitive complication was persistent at 12 months.
No infections, eventrations, dural tears or vascular tears were reported.
Two device-related events were reported from the radiological evaluation: one migration of superior plate, remaining stable through time; one cage subsidence occurred within 12-month follow-up in a 76-year-old female; however, interbody fusion was attained. Neither event had clinical consequence.
Subsidence rate was 2.0 % at 12-month follow-up (1 subsidence/51 CT analyzed; 3 cases not analyzed because the CT before discharge was not performed).
The radiological analysis reported neither cage migration nor plate or bony fracture (60 complete radiographic files were available for analysis at 12-month follow-up).
There were no revision surgeries at the index level in this population.
Pain and disability
Both back and leg pain decreased immediately after surgery. The difference from baseline was statistically significant from 6 weeks and through the follow-up period (Fig. 3).
Visual Analog Scale (VAS 0–10 cm) results for back pain (black line) and for leg pain (gray line) over time-course of the follow-up (pre-op; and 6 weeks, 3, 6, and 12 months after ALIF procedures). Results are expressed as mean ± SEM. *p ≤ 0.0001 compared to pre-op baseline; § p = 0.0003 compared to pre-op baseline
Functional outcomes also showed improvement: mean ODI decreased significantly compared to baseline, from early post-op and up to 12-month follow-up (Fig. 4). The change in ODI score at 12-month follow-up compared to baseline averaged 26.6 points (range −30 to 60 %). Within the ODI questionnaire, walking, ranging from 0 to 5, also decreased significantly from baseline to 12 months (1.94 and 0.64 respectively, p < 0.0001).
Quality of life
Outcomes for quality of life also show improvement (Fig. 5): SF-36 increased significantly compared to baseline for both physical and mental scales.
Figure 6 shows the use of any class of analgesic, opioids or non-steroidal anti-inflammatory drugs over time: medication use decreased following the ALIF procedures. The rate of patients using analgesics was significantly lower at 12 months compared to baseline (p < 0.0001).
Satisfaction
Patient satisfaction is shown in Table 3. At 12-month follow-up, 88.7 % of patients were very satisfied or satisfied with overall surgery results, 81.1 % with results on back pain, and 78.9 % with results on leg pain.
Additionally, at 12-month follow-up, 80.4 % of the patients (41/51) reported their willingness to undergo the same surgery again.
Radiographic performances
Anterior and posterior disc heights increased significantly after ALIF procedure (Fig. 7).
Discussion
Despite some positive results [17–19], stand-alone cages have not proven their full efficacy [9, 20]. Stand-alone ALIF with integrated screws have shown better clinical outcomes when compared to classical cages with posterior pedicle screws [12].
In our study, we observed similar improvements of clinical outcomes. Symptom relief was similar for back and radicular symptoms, suggesting that surgeries were effective in treating both. Furthermore, no revision surgeries were reported. Limitations of this study arise from the small size of the population and a selection bias due to the fact that 74.7 % of the inclusions were made by one highly experienced surgeon, which could have had an influence regarding the results transposability. However, smoking, work-related injury, previous lumbar surgeries, and training cases have been included.
The main goals of an ALIF are a solid fusion of the segment, and preservation or restoration of disc height and spinal alignment. Fusion rate data are very heterogeneous in the literature. Li et al. [9] reported a range between 51.9 and 88.9 % fusion in a literature review. Anjarwalla et al. [21] assessed the fusion rate of one stand-alone cage ALIF versus the same ALIF cage with different techniques of posterior supplemental fixation. The fusion rate for the stand-alone cage was 51 % versus 89 % and 88 % for the two groups supplemented with pedicle screws. The difference was significant. Strube et al. [12] using a cage with four integrated screws reported 91.2 %.
This heterogeneity is mainly related to the difficulty of assessing fusion via non invasive methods. Authors generally consider the radiographic assessment as reliable, but the threshold value of motion on dynamic X-rays varied from 1° for Brantigan to 5° for Kuslich [22]. In our study, we chose CT assessment. As Santos [15] and Zebdlick [2] reported, CT is the best way to visualize the bone continuity, because technical measurements errors are unavoidable on standard X-rays and finally because we can avoid the disputed motion threshold. In our study we reported a fusion rate of 96.3 %. We assume that among other biomechanical reasons supporting this result, the wide grafting area provided by this implant (up to 388 mm2) is crucial and despite some heterogeneity in graft type (90.2 % of it was made of autologous bone + BMP), which could be regarded as a limitation of this study.
Subsidence is a common problem with cages and difficult to define. Le et al. [23] considers subsidence as “any compromise of either endplate” due to the cage. For Beutler et al. [24], subsidence is characterized by a decrease in the specific vertical height on lateral X-rays. Another difficulty faced is the way to measure subsidence and to determine a threshold. Le et al. [23] have used a viewing station with calibrated linear measurements. Beutler et al. [24] defined subsidence as a height loss of greater than 2 mm. Lee et al. [16] measured the “endplate destruction length” on CT in coronal and sagittal planes, which is definitely the most accurate measurement technique published to date.
Choi et al. [25] reported 76.7 % subsidence with a carbon cage. Weiner et al. [26] in their Brantigan ALIF cage series reported 50 %, while Butler [24] reported 10 % in ALIF with a pair of threaded cages, and Lee et al. [16], in a study on 54 patients with supplemented posterior lumbar interbody fusion, reported 22 and 28 % subsidence rates in sagittal and coronal planes, respectively.
We have reported 1 subsidence (out of 51 analyzed cases) from CT examination. Several reasons are possible: the preparations of the endplates was meticulous, without drilling or shaving; the design of the integrated self-guided titanium plating and the size of contact surface of the PEEK cages (up to 835 mm2) theoretically provide immediate stability in a safe way and share the loading [22] (the typical surface of vertebral endplates is 1,259 mm2).
Conclusion
Safety and efficacy of this new concept of supplemented stand-alone cage was confirmed at these 12 months for treatment of degenerative conditions with significant improvement in both pain and function, a low subsidence rate, no device-related serious adverse events, and no revision surgeries at the index level. We intend to proceed further in this study (up to 10 years) to confirm these results and to analyze the rate of adjacent level disease.
References
Bagby GW (1988) Arthrodesis by the distraction-compression method using a stainless steel implant. Orthopedics 11(6):931–934
Zdeblick TA, Phillips FM (2003) Interbody cage devices. Spine 28(15 Suppl):2–7. doi:10.1097/01.brs.0000076841.93570.78
Kettler A, Wilke HJ, Dietl R, Krammer M, Lumenta C, Claes L (2000) Stabilizing effect of posterior lumbar interbody fusion cages before and after cyclic loading. J Neurosurg 92(1 Suppl):87–92
Fan S, Hu Z, Zhao F, Zhao X, Huang Y, Fang X (2010) Multifidus muscle changes and clinical effects of one-level posterior lumbar interbody fusion: minimally invasive procedure versus conventional open approach. Eur Spine J 19(2):316–324. doi:10.1007/s00586-009-1191-6
Faundez AA, Schwender JD, Safriel Y, Gilbert TJ, Mehbod AA, Denis F, Transfeldt EE, Wroblewski JM (2009) Clinical and radiological outcome of anterior-posterior fusion versus transforaminal lumbar interbody fusion for symptomatic disc degeneration: a retrospective comparative study of 133 patients. Eur Spine J 18(2):203–211. doi:10.1007/s00586-008-0845-0
Sasso RC, Kitchel SH, Dawson EG (2004) A prospective, randomized controlled clinical trial of anterior lumbar interbody fusion using a titanium cylindrical threaded fusion device. Spine 29(2):113–122. doi:10.1097/01.brs.0000107007.31714.77 (discussion 121-2)
Phillips FM, Cunningham B, Carandang G, Ghanayem AJ, Voronov L, Havey RM, Patwardhan AG (2004) Effect of supplemental translaminar facet screw fixation on the stability of stand-alone anterior lumbar interbody fusion cages under physiologic compressive preloads. Spine 29(16):1731–1736
Button G, Gupta M, Barrett C, Cammack P, Benson D (2005) Three- to six-year follow-up of stand-alone BAK cages implanted by a single surgeon. Spine J 5(2):155–160. doi:10.1016/j.spinee.2004.06.021
Li J, Dumonski ML, Liu Q, Lipman A, Hong J, Yang N, Jin Z, Ren Y, Limthongkul W, Bessey JT, Thalgott J, Gebauer G, Albert TJ, Vaccaro AR (2010) A multicenter study to evaluate the safety and efficacy of a stand-alone anterior carbon I/F Cage for anterior lumbar interbody fusion: two-year results from a Food and Drug Administration investigational device exemption clinical trial. Spine 35(26):1564–1570. doi:10.1097/BRS.0b013e3181ef5c14
Cho CB, Ryu KS, Park CK (2010) Anterior lumbar interbody fusion with stand-alone interbody cage in treatment of lumbar intervertebral foraminal stenosis: comparative study of two different types of cages. J Korean Neurosurg Soc 47(5):352–357. doi:10.3340/jkns.2010.47.5.352
Gerber M, Crawford NR, Chamberlain RH, Fifield MS, LeHuec JC, Dickman CA (2006) Biomechanical assessment of anterior lumbar interbody fusion with an anterior lumbosacral fixation screw-plate: comparison to stand-alone anterior lumbar interbody fusion and anterior lumbar interbody fusion with pedicle screws in an unstable human cadaver model. Spine 31(7):762–768. doi:10.1097/01.brs.0000206360.83728.d2
Strube P, Hoff E, Hartwig T, Perka CF, Gross C, Putzier M (2011) Stand-alone anterior versus anteroposterior lumbar interbody single-level fusion after a mean follow-up of 41 months. J Spinal Disord Tech. doi:10.1097/BSD.0b013e3182263d91
Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine 29(17):1938–1944
Madan SS, Boeree NR (2003) Comparison of instrumented anterior interbody fusion with instrumented circumferential lumbar fusion. Eur Spine J 12(6):567–575. doi:10.1007/s00586-002-0516-5
Santos ER, Goss DG, Morcom RK, Fraser RD (2003) Radiologic assessment of interbody fusion using carbon fiber cages. Spine 28(10):997–1001. doi:10.1097/01.BRS.0000061988.93175.74
Lee JH, Jeon DW, Lee SJ, Chang BS, Lee CK (2010) Fusion rates and subsidence of morselized local bone grafted in titanium cages in posterior lumbar interbody fusion using quantitative three-dimensional computed tomography scans. Spine 35(15):1460–1465. doi:10.1097/BRS.0b013e3181c4baf5
Kuslich SD, Ulstrom CL, Griffith SL, Ahern JW, Dowdle JD (1998) The Bagby and Kuslich method of lumbar interbody fusion. History, techniques, and 2-year follow-up results of a United States prospective, multicenter trial. Spine 23(11):1267–1278 (discussion 1279)
Penta M, Fraser RD (1997) Anterior lumbar interbody fusion. A minimum 10-year follow-up. Spine 22(20):2429–2434
Rahn KA, Shugart RM, Wylie MW, Reddy KK, Morgan JA (2010) The effect of lordosis, disc height change, subsidence, and transitional segment on stand-alone anterior lumbar interbody fusion using a nontapered threaded device. Am J Orthop (Belle Mead, NJ) 39(12):124–129
Zelle B, Konig F, Enderle A, Bertagnoli R, Dorner J (2002) Circumferential fusion of the lumbar and lumbosacral spine using a carbon fiber ALIF cage implant versus autogenous bone graft: a comparative study. J Spinal Disord Tech 15(5):369–376
Anjarwalla NK, Morcom RK, Fraser RD (2006) Supplementary stabilization with anterior lumbar intervertebral fusion—a radiologic review. Spine 31(11):1281–1287. doi:10.1097/01.brs.0000217692.90624.ab
McAfee PC, Boden SD, Brantigan JW, Fraser RD, Kuslich SD, Oxland TR, Panjabi MM, Ray CD, Zdeblick TA (2001) Symposium: a critical discrepancy—a criteria of successful arthrodesis following interbody spinal fusions. Spine 26(3):320–334
Le TV, Baaj AA, Dakwar E, Burkett CJ, Murray G, Smith DA, Uribe JS (2012) Subsidence of polyetheretherketone intervertebral cages in minimally invasive lateral retroperitoneal transpsoas lumbar interbody fusion. Spine 37(14):1268–1273. doi:10.1097/BRS.0b013e3182458b2f
Beutler WJ, Peppelman WC Jr (2003) Anterior lumbar fusion with paired BAK standard and paired BAK proximity cages: subsidence incidence, subsidence factors, and clinical outcome. Spine J 3(4):289–293
Choi JY, Sung KH (2006) Subsidence after anterior lumbar interbody fusion using paired stand-alone rectangular cages. Eur Spine J 15(1):16–22. doi:10.1007/s00586-004-0817-y
Weiner BK, Fraser RD (1998) Spine update lumbar interbody cages. Spine 23(5):634–640
Conflict of interest
J. A is currently receiving royalties for the development of the considered product. T. V. has currently or previously financial activity for the work under consideration.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Allain, J., Delecrin, J., Beaurain, J. et al. Stand-alone ALIF with integrated intracorporeal anchoring plates in the treatment of degenerative lumbar disc disease: a prospective study on 65 cases. Eur Spine J 23, 2136–2143 (2014). https://doi.org/10.1007/s00586-014-3364-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3364-1