Abstract
Purpose
This study aimed to examine the incidence, case fatality rate, and characteristics of perioperative symptomatic pulmonary thromboembolism (PS-PTE) throughout Japan.
Methods
From 2002 to 2011, confidential questionnaires were mailed annually to all Japanese Society of Anesthesiologists-certified training hospitals for data collection to determine the incidence and case fatality rate of PS-PTE patients. Data from 10,537 institutions in which a total of 11,786,489 surgeries had been performed were analyzed using the Mann–Whitney and Chi-square tests.
Results
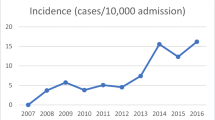
In total, 3,667 PS-PTE cases were identified. The average incidence of PS-PTE was 3.1 (2.2–4.8) per 10,000 surgeries, and the average case fatality rate was 17.9 % (12.9–28.8 %). The incidence of PS-PTE began to significantly decrease in 2004 compared with that of 2002 (0.0036 vs. 0.0044 %: p < 0.01). The case fatality rate temporarily increased toward 2005 (17.9 to 28.8 %); however, it gradually decreased since 2008 (15.7 %) and was the lowest (12.9 %) in 2011. Regarding the trends in prophylaxis, the rate of mechanical prophylaxis increased significantly in 2003 compared with that of 2002 (59.5 vs. 35.0 %: p < 0.01), and almost plateaued (73.1–83.1 %) after 2004. Furthermore, the rate of pharmacological prophylaxis started increasing in 2008 (17.6 %) and reached around 30 % after 2009 (28.8–30.2 %).
Conclusions
The results of our 10-year survey study show that the incidence of PS-PTE decreased significantly since 2004, and the case fatality rate seemed to show a downward trend since 2008. Major changes in the distribution of prophylaxis in PS-PTE patients were observed.




Similar content being viewed by others
References
Sandler DA, Martin JF. Autopsy proven pulmonary embolism in hospital patients: are we detecting enough deep vein thrombosis? J R Soc Med. 1989;82:203–5.
Lindblad B, Eriksson A, Bergqvist D. Autopsy-verified pulmonary embolism in a surgical department: analysis of the period from 1951 to 1988. Br J Surg. 1991;78:849–52.
Kuroiwa M, Furuya H, Seo N, Morita K, Sha M, Iwao Y, Sasaki J, Ito M. Incidence and characteristics of perioperative pulmonary thromboembolism in Japan. Masui. 2004;53:454–63 (in Japanese).
Kuroiwa M, Furuya H, Seo N, Morita K, Sha M, Iwao Y, Sasaki J, Ito M. Incidence and characteristics of perioperative pulmonary thromboembolism in Japan in 2003. Masui. 2005;54:822–8 (in Japanese).
Kuroiwa M, Seo N, Furuya H, Irita K, Sawa T, Ito M, Nakamura M. Incidence and characteristics of perioperative pulmonary thromboembolism in Japan in 2004. Masui. 2006;55:1031–8 (in Japanese).
Kuroiwa M, Furuya H, Seo N, Irita K, Sawa T, Ito M, Nakamura M, Kitaguchi K, Sakuma M, Morita K, Chuma R. Incidence and characteristics of perioperative pulmonary thromboembolism in Japan from 2005 through 2007–results of research by Japanese Society of Anesthesiologists, Committee on Patient Safety and Risk Management. Perioperative Pulm Thromboembolism Work Gr. Masui. 2009;58:1567–73 (in Japanese).
Kuroiwa M, Furuya H, Seo N, Kitaguchi K, Nakamura M, Sakuma M, Chuma R. Incidence and clinical characteristics of perioperative pulmonary thromboembolism in Japan in 2008–results from the annual study of Japanese Society of Anesthesiologists, Committee on Patient Safety and Risk Management. Perioperative Pul Thromboembolism Work Gr. Masui. 2010;59:667–73 (in Japanese).
Gould MK, Garcia DA, Wren SM, Karanicolas PJ, Arcelus JI, Heit JA, Samama CM. American College of Chest Physicians. Prevention of VTE in non-orthopedic surgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e227S–77S.
Irita K, Tsuzaki K, Sanuki M, Sawa T, Nakatsuka H, Makita K, Morita K. Recent changes in the incidence of life-threatening events in the operating room: JSA surveys between 2001 and 2005. Masui. 2007;56:1433–46 (in Japanese).
Nakamura M. Japanese Guidelines for Prevention of Venous Thromboembolism. J Jpn Soc Clin Anesth. 2004;24:480–7.
Haut ER, Lau BD, Kraenzlin FS, Hobson DB, Kraus PS, Carolan HT, Haider AH, Holzmueller CG, Efron DT, Pronovost PJ, Streiff MB. Improved prophylaxis and decreased rates of preventable harm with the use of a mandatory computerized clinical decision support tool for prophylaxis for venous thromboembolism in trauma. Arch Surg. 2012;147:901–7.
Shackford SR, Rogers FB, Terrien CM, Bouchard P, Ratliff J, Zubis R. A 10-year analysis of venous thromboembolism on the surgical service: the effect of practice guidelines for prophylaxis. Surgery. 2008;144:3–11.
Nicolaides AN, Breddin HK, Fareed J, Goldhaber S, Haas S, Hull R, Kalodiki E, Myers K, Samama M, Sasahara A, Cardiovascular Disease Educational and Research Trust and the International Union of Angiology. Prevention of venous thromboembolism. International Consensus Statement. Guidelines compiled in accordance with the scientific evidence. Int Angiol. 2001;20:1–37.
Shoda N, Yasunaga H, Horiguchi H, Matsuda S, Ohe K, Kadono Y, Tanaka S. Risk factors affecting in-hospital mortality after hip fracture: retrospective analysis using the Japanese Diagnosis Procedure Combination Database. BMJ Open. 2012;4(2):e000416.
Gangireddy C, Rectenwald JR, Upchurch GR, Wakefield TW, Khuri S, Henderson WG, Henke PK. Risk factors and clinical impact of postoperative symptomatic venous thromboembolism. J Vasc Surg. 2007;45:335–41.
De Martino RR, Goodney PP, Spangler EL, Wallaert JB, Corriere MA, Rzucidlo EM, Walsh DB, Stone DH. Variation in thromboembolic complications among patients undergoing commonly performed cancer operations. J Vasc Surg. 2012;55:1035–40.
Stein PD, Beemath A, Meyers FA, Skaf E, Sanchez J, Olson RE. Incidence of venous thromboembolism in patients hospitalized with cancer. Am J Med. 2006;119:60–8.
Kunisawa S, Ikai H, Imanaka Y. Incidence and prevention of postoperative venous thromboembolism: are they meaningful quality indicators in Japanese health care settings? World J Surg. 2012;36:280–6.
Hill J, Treasure T. National Clinical Guideline Centre for Acute and Chronic Conditions. Reducing the risk of venous thromboembolism in patients admitted to hospital: summary of NICE guidance. BMJ. 2010;340:c95.
Yamada N, Ota S, Liu Y, Crane MM, Chang CM, Thaker S, Nakamura M, Ito M. Risk factors for nonfatal pulmonary embolism in a Japanese population: a hospital-based case-control study. Angiology. 2010;61:269–74.
Sakon M, Maehara Y, Yoshikawa H, Akaza H. Incidence of venous thromboembolism following major abdominal surgery: a multi-center, prospective epidemiological study in Japan. J Thromb Haemost. 2006;4:581–6.
Yu YB, Gau JP, Liu CY, Yang MH, Chiang SC, Hsu HC, Hong YC, Hsiao LT, Liu JH, Chiou TJ, Chen PM, Lee TS, Chou LF, Tzeng CH, Chen TJ. A nation-wide analysis of venous thromboembolism in 497,180 cancer patients with the development and validation of a risk-stratification scoring system. Thromb Haemost. 2012;108:225–35.
Yang SS, Yu CS, Yoon YS, Yoon SN, Lim SB, Kim JC. Symptomatic venous thromboembolism in Asian colorectal cancer surgery patients. World J Surg. 2011;35:881–7.
Liew NC, Chang YH, Choi G, Chu PH, Gao X, Gibbs H, Ho CO, Ibrahim H, Kim TK, Kritpracha B, Lee LH, Lee L, Lee WY, Li YJ, Nicolaides AN, Oh D, Pratama D, Ramakrishnan N, Robless PA, Villarama-Alemany G. Wong R; Asian Venous Thrombosis Forum. Asian venous thromboembolism guidelines: prevention of venous thromboembolism. Int Angiol. 2012;31:501–16.
Desciak MC, Martin DE. Perioperative pulmonary embolism: diagnosis and anesthetic management. J Clin Anesth. 2011;23:153–65.
Spyropoulos AC, Hussein M, Lin J, Battleman D. Rates of symptomatic venous thromboembolism in US surgical patients: a retrospective administrative database study. J Thromb Thrombolysis. 2009;28:458–64.
McNamara I, Sharma A, Prevost T, Parker M. Symptomatic venous thromboembolism following a hip fracture. Acta Orthop. 2009;80:687–92.
Milbrink J, Bergqvist D. The incidence of symptomatic venous thromboembolic events in orthopaedic surgery when using routine thromboprophylaxis. Vasa. 2008;37:353–7.
Stein PD, Kayali F, Olson RE, Milford CE. Pulmonary thromboembolism in Asians/Pacific Islanders in the United States: analysis of data from the National Hospital Discharge Survey and the United States Bureau of the Census. Am J Med. 2004;116:435–42.
Klatsky AL, Armstrong MA, Poggi J. Risk of pulmonary embolism and/or deep venous thrombosis in Asian-Americans. Am J Cardiol. 2000;85:1334–7.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix A: The percentage of surgeries in each condition
2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Average | |
|---|---|---|---|---|---|---|---|---|---|---|---|
Age (years) | |||||||||||
0-5 | 6.2 | 6.1 | 6.0 | 6.0 | 6.0 | 6.0 | 5.2 | 4.8 | 4.8 | 4.5 | 5.5 |
6-18 | 7.0 | 6.8 | 6.6 | 6.6 | 6.6 | 6.6 | 6.1 | 6.0 | 5.9 | 6.0 | 6.4 |
19-65 | 54.7 | 53.8 | 53.4 | 53.4 | 53.4 | 53.4 | 50.7 | 50.0 | 49.5 | 49.5 | 52.2 |
66-85 | 29.8 | 30.9 | 31.5 | 31.5 | 31.5 | 31.5 | 34.9 | 35.9 | 36.2 | 36.4 | 33.0 |
86- | 2.3 | 2.4 | 2.6 | 2.6 | 2.6 | 2.6 | 3.1 | 3.3 | 3.6 | 3.7 | 2.9 |
Sex | |||||||||||
Male | No data | no data | 49.6 | 49.6 | 49.6 | 49.6 | 48.5 | 48.8 | 48.5 | 48.5 | 49.1 |
Female | No data | no data | 50.4 | 50.4 | 50.4 | 50.4 | 51.5 | 51.2 | 51.5 | 51.5 | 50.9 |
Surgical site | |||||||||||
Brain | 3.8 | 3.7 | 3.6 | 3.6 | 3.6 | 3.6 | 3.3 | 3.2 | 3.3 | 3.6 | 3.5 |
Thorax | 3.5 | 3.6 | 3.5 | 3.5 | 3.5 | 3.5 | 3.3 | 3.4 | 3.5 | 3.4 | 3.5 |
Heart and/or major vascular | 3.4 | 3.4 | 3.3 | 3.3 | 3.3 | 3.3 | 3.1 | 3.0 | 3.2 | 3.4 | 3.3 |
Thorax and abdomen | 0.6 | 0.6 | 0.6 | 0.6 | 0.6 | 0.6 | 0.5 | 0.4 | 0.5 | 0.5 | 0.6 |
Abdomen | 29.4 | 29.1 | 30.1 | 30.1 | 30.1 | 30.1 | 29.2 | 29.1 | 28.7 | 33.0 | 29.9 |
Cesarean section | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 3.7 | 3.7 | 3.6 | 3.6 | 3.6 |
Head, pharynx,larynx | 15.2 | 15.0 | 14.9 | 14.9 | 14.9 | 14.9 | 14.2 | 14.0 | 13.9 | 13.0 | 14.5 |
Chest/abdominal wall/perineum | 15.6 | 16.3 | 15.7 | 15.7 | 15.7 | 15.7 | 15.5 | 15.8 | 15.6 | 12.0 | 15.4 |
Spine | 3.6 | 3.7 | 3.7 | 3.7 | 3.7 | 3.7 | 4.6 | 4.8 | 5.0 | 4.9 | 4.1 |
Hip, upper/lower limbs | 18.0 | 18.0 | 18.5 | 18.5 | 18.5 | 18.5 | 19.6 | 20.2 | 20.1 | 20.3 | 19.0 |
Appendix B: The estimated number of surgeries in each condition
2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Total | Average | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Total number of surgeries | 837,540 | 925,260 | 1,131,154 | 922,453 | 1,209,135 | 1,150,783 | 1,177,626 | 1,422,034 | 1,560,987 | 1,449,517 | 11,786,489 | 1,178,649 |
Age (years) | ||||||||||||
0-5 | 51,901 | 56,176 | 67,499 | 55,046 | 72,153 | 68,671 | 61,452 | 68,288 | 75,167 | 65,347 | 641,700 | 64,170 |
6-18 | 58,295 | 63,070 | 74,935 | 61,109 | 80,101 | 76,236 | 71,816 | 85,517 | 91,812 | 86,873 | 749,763 | 74,976 |
19-65 | 458,487 | 497,691 | 603,742 | 492,350 | 645,363 | 614,219 | 596,468 | 710,718 | 772,573 | 716,952 | 6,108,562 | 610,856 |
66-85 | 249,985 | 285,994 | 355,925 | 290,256 | 380,462 | 362,101 | 411,266 | 510,675 | 565,447 | 526,928 | 3,939,037 | 393,904 |
86- | 18,873 | 22,329 | 29,053 | 23,693 | 31,056 | 29,557 | 36,625 | 46,836 | 55,988 | 53,417 | 347,427 | 34,743 |
Male | N/A | N/A | 560,509 | 457,094 | 599,150 | 570,236 | 571,676 | 694,260 | 756,960 | 702,783 | 4,912,668 | 614,084 |
Female | N/A | N/A | 570,645 | 465,359 | 609,985 | 580,547 | 605,950 | 727,774 | 804,027 | 746,734 | 5,111,021 | 638,878 |
Surgical site | ||||||||||||
Brain | 31,831 | 34,439 | 40,519 | 33,043 | 43,312 | 41,222 | 38,776 | 46,185 | 51,308 | 51,748 | 412,383 | 41,238 |
Thorax | 29,417 | 33,613 | 39,788 | 32,447 | 42,531 | 40,479 | 39,303 | 48,112 | 55,360 | 49,308 | 410,359 | 41,036 |
Heart and/or major vascular | 28,483 | 31,060 | 37,443 | 30,535 | 40,024 | 38,093 | 37,091 | 42,318 | 50,176 | 49,702 | 384,924 | 38,492 |
Thorax and abdomen | 5,373 | 5,594 | 6,732 | 5,490 | 7,196 | 6,849 | 5,786 | 6,176 | 7,659 | 6,811 | 63,665 | 6,367 |
Abdomen | 246,621 | 269,105 | 340,032 | 277,295 | 363,474 | 345,933 | 344,175 | 413,200 | 448,640 | 478,104 | 3,526,578 | 352,658 |
Cesarean section | 29,426 | 32,784 | 39,862 | 32,507 | 42,610 | 40,553 | 44,140 | 52,489 | 55,447 | 51,967 | 421,785 | 42,178 |
Head, pharynx,larynx | 127,209 | 138,648 | 168,741 | 137,608 | 180,374 | 171,669 | 167,179 | 198,841 | 217,726 | 188,351 | 1,696,347 | 169,635 |
Chest/abdominal wall/perineum | 130,924 | 150,695 | 177,753 | 144,957 | 190,008 | 180,838 | 182,888 | 224,855 | 244,127 | 174,100 | 1,801,146 | 180,115 |
Spine | 30,312 | 34,199 | 41,755 | 34,051 | 44,633 | 42,479 | 54,676 | 68,396 | 77,778 | 71,009 | 499,289 | 49,929 |
Hip, upper/lower limbs | 150,541 | 166,723 | 209,660 | 170,977 | 224,114 | 213,299 | 231,085 | 286,974 | 314,499 | 294,028 | 2,261,899 | 226,190 |
About this article
Cite this article
Kuroiwa, M., Morimatsu, H., Tsuzaki, K. et al. Changes in the incidence, case fatality rate, and characteristics of symptomatic perioperative pulmonary thromboembolism in Japan: Results of the 2002–2011 Japanese Society of Anesthesiologists Perioperative Pulmonary Thromboembolism (JSA-PTE) Study. J Anesth 29, 433–441 (2015). https://doi.org/10.1007/s00540-014-1939-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-014-1939-y