Abstract
Purpose
High-frequency oscillatory ventilation (HFOV) is thought to protect the lungs of acute respiratory distress syndrome (ARDS) patients. The performance and mechanical characteristics of high-frequency oscillatory ventilators, especially with regard to delivering appropriate tidal volume (V T) to compromised lungs, might affect the outcome of patients. We evaluated the performance of two such ventilators using a model lung with a position sensor.
Methods
We tested the Metran R100 and SensorMedics 3100B. V T was measured using the model lung with the compliance set at 20 or 50 ml/cmH2O and the resistance at 0 or 20 cmH2O/l/s. Oscillator frequency was set at 5, 7, and 9 Hz, and amplitude was set at 25%, 50%, 75%, and 100% (100% being maximum amplitude available at each setting configuration).
Results
At each model lung setting, R100 delivered greater V T at 5 Hz. V T differences between the ventilators decreased as frequency increased and were negligible at 9 Hz. At each model lung setting and frequency, as amplitude increased from 25% to 100%, V T increased proportionally more with R100. With an I:E ratio of 1:1, 3100B delivered greater V T than with 1:2.
Conclusion
Because it is able to deliver comparably greater V T, R100 may be a better choice for HFOV in critical ARDS patients. Better proportionality may be a result of more effective amplitude titration for adjusting PaCO2 during oscillation.
Similar content being viewed by others
Introduction
To prevent barotrauma, high-frequency oscillatory ventilation (HFOV) has long been used for neonates and infants. In HFOV, lungs are inflated with a tidal volume (V T) less than anatomic deadspace and at a high respiratory rate (3–20 Hz) [1]. The advantage of HFOV is that, with the maintenance of high mean airway pressure (PEEP), it can ventilate patients without raising peak alveolar pressure. This mode of ventilation is thought to avoid the transmission of pressure swings from the central airways to the peripheral airways or alveoli [2]. Many investigators have reported that HFOV provides better oxygenation [3], ventilation [4], and lung protection [5, 6].
In acute respiratory distress syndrome (ARDS) patients, lung-protective ventilation, using low tidal volume to prevent barotrauma or volutrauma [7] and high PEEP to prevent collapse and subsequent reopening of injured airways and alveoli [8–10], has been applied clinically. The ARDS Network reported better survival for ARDS or acute lung injury (ALI) patients ventilated with 6 ml/kg V T than with 12 ml/kg V T [11]. HFOV is considered protective because peak and mean airway pressures, and PEEP, are almost the same as in alveoli and it is easy to provide enough levels of PEEP with limiting peak airway pressures at the same time. Recently, ventilators that provide HFOV in adult patients have been developed and introduced for clinical use [12]. In a randomized, controlled clinical trial comparing HFOV with conventional mechanical ventilation (CMV) in ARDS patients, the 30-day mortality rate in the HFOV group was found to be lower than in the CMV group, although there was not statistical significance (P = 0.057) [13]. However, reports from several other clinical trials comparing HFOV with CMV [14–16] have failed to corroborate these results.
Other studies have reported successful 9 Hz [17] and 3–5 Hz [13] oscillation in ARDS patients. It is not clear if the reported success of the strategy was the result of the performance characteristics of the high-frequency oscillatory ventilator or was skewed by studying what might have been milder cases of ARDS. Even so, it is widely conjectured that as HFOV frequency increases, so does its lung-protective effect. Because oscillatory ventilator performance may crucially affect patient outcome, we evaluated how two adult high-frequency oscillatory ventilators delivered V T to a model lung with a position sensor.
Materials and methods
Model lung
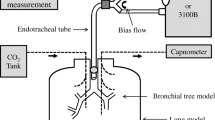
To monitor the volume change, a position sensor was fixed to the model lung (TTL; Michigan Instruments, Grand Rapids, MI, USA). This position sensor converts the movement of a metal bar attached to the model lung into measurable electrical output (0–5 V). Volume in the model lung was calibrated using a 1-l syringe. As a result of this approximation of arc movement as linear, 7% overestimation of V T could exist at maximum depending on the mean airway pressure in our pilot study. With and without an additional resistor of 20 cmH2O/l/s (Pneuflo; Michigan Instruments), an 8.0-mm internal-diameter endotracheal tube was set at the airway opening of the model lung. The compliance of the model lung was set at 20 or 50 ml/cmH2O. We were thus able to test the model lung at four basic settings. The combination of a compliance of 50 ml/cmH2O and no additional resistance simulated a normal lung; 20 ml/cmH2O and no additional resistance simulated restrictive lung disease; 50 ml/cmH2O and additional resistance of 20 cmH2O/l/s simulated obstructive lung disease; and 20 ml/cmH2O and an additional resistance of 20 cmH2O/l/s simulated mixed lung dysfunction.
Ventilators
Two high-frequency oscillatory ventilators for adults were evaluated: SensorMedics 3100B (Yorba Linda, CA, USA) and Metran R100 (Saitama, Japan). Each of these uses a diaphragm for oscillation. Developed in Japan, R100 is a model with approval in Japan and Korea for clinical use with adult patients.
Protocol
Each ventilator was tested with frequency set at 5, 7, and 9 Hz and with amplitude set at 100% (i.e., maximum amplitude at each setting combination) and at 75%, 50%, and 25%. I:E ratio was set at 1:1 and 1:2 with the SensorMedics 3100B and at 1:1 with the Metran R100. Mean airway pressure set at 15 cmH2O and the fraction of inspiratory oxygen concentration set at 0.21 throughout the experiment. On 3100B, constant flow was set at 15 l/min and on R100, at 20 l/min.
Measurements and analysis
Airway pressures between the endotracheal tube and ventilator circuit Y-piece (Paw) and between the resistor and model lung (Ptr) were monitored using pressure transducers with built-in amplifiers (Fig. 1). This type of device measures airway pressure directly without tubing, thus eliminating the risk of underestimating airway pressure owing to the damping effect of high-frequency oscillation.
Measured analog signals of airway pressures and lung volume were sampled at 667 Hz and stored in a personal computer using an A–D converter (DI-220; Dataq Instruments, Akron, OH, USA). These data were analyzed using a playback software (Windaqex; Dataq Instruments).
Amplitude of oscillation was calculated as the pressure difference between highest and lowest Paw and Ptr in each oscillatory cycle. Delivered tidal volume (V T) was calculated as the volume difference between highest and lowest model lung volume in each oscillatory cycle. Three consecutive oscillatory cycles were analyzed, and average values were used. We did not show the results of statistical analysis in this study because standard deviation in each setting was almost zero so that significant difference existed in every comparison.
Results
Table 1 shows V T for R100 or 3100B at each setting of the model lung. With both ventilators, V T decreased along with the decreased compliance or increased resistance of the model lung. At each setting, R100 delivered greater V T than 3100B at 5 Hz. The difference in V T between the two ventilators decreased as frequency increased and was negligible at 9 Hz.
Figure 2a, b shows the V T delivered with frequency set at 5 Hz by R100 (Fig. 2a) and 3100B (Fig. 2b) at various model lung settings and amplitude set at 25%, 50%, or 100% (of maximum). Results show that R100 delivered proportionally greater V T at each amplitude (for each combination of settings, amplitude was set according to values available on the graphic display of the ventilator).
Figure 3 shows the effect of I:E ratio on V T using 3100B with frequency set at 5 Hz. The delivered V T was greater when the I:E ratio is 1:1 than when 1:2.
Discussion
The major findings of this study are (1) R100 delivers more V T than 3100B, especially at 5 Hz; (2) at the combinations of the settings tested, R100 is capable of delivering greater V T proportional to the amplitude; and (3) 3100B delivered greater V T when the I:E ratio was 1:1 than when it was 1:2.
So far as we know, this is the first report comparing high-frequency oscillatory ventilators for adults. During HFOV, delivered V T at each frequency is an important clinical variable that is difficult to measure using conventional flow-metering methods. Hatcher et al. [18] measured V T with high-frequency oscillatory ventilators for neonates using a bodyplethysmograph in an animal model. It is difficult to use a bodyplethysmograph for large animals. In addition, the lung model is more suitable than an animal model when comparing ventilator performances with changing lung mechanics. In this study, we directly measured V T in a model lung during HFOV using a position sensor and compared the results obtained with two high-frequency oscillatory ventilators.
The position sensor used in this study converts movement of a metal bar to electrical voltage: through travel of 0–50 mm, with a maximum resolution of 0.01 mm, movement is measured as DC voltage of 0–5 V. The distance is sufficient and the resolution fine enough for the purposes of this study [19].
3100B has an available frequency range of 3–15 Hz. The range for R100 is 5–15 Hz. In the overlapping range, we tested three settings, 5, 7, and 9 Hz, but did not test above 10 Hz because such frequencies are rarely used in adult patients. In addition, at frequencies greater than 10 Hz, we detected resonance in our model lung.
Although the diameter of a diaphragms used in the ventilators are similar—3100B, 185 mm; R100, 180 mm—we found that R100 delivered comparatively more V T, especially at the lowest frequency tested. Because the specifications have not been published, we can only speculate that the oscillating surface of the diaphragm in R100 is designed to travel a greater distance than the diaphragm in 3100B.
While 3100B allows the inspiratory time to be set at 30–50% of the oscillatory cycle, R100 is fixed at 50%. When we compared V T using I:E ratios of 1:2 and 1:1, we found a lesser V T when the ratio was 1:2. We surmise that V T declines owing to the shorter inspiratory time when the I:E ratio is 1:2. Even so, an I:E ratio of 1:2 may be indicated if air trapping is clinically suspected. When devising a strategy, however, it is necessary to weigh the effect on V T of both of I:E ratio and the reported relationship between I:E and mean alveolar pressure [20].
3100B has featured in most of the clinical reports of the application of HFOV for ARDS patients [13–16]. When ventilating severe ARDS patients, it is sometimes very difficult to maintain normocapnia. In such situations, frequency is usually reduced to increase V T; this may result in deflation of the endotracheal-tube cuff. Moreover, if hypercapnia persists, it may become necessary to administer sodium bicarbonate when blood pH cannot be maintained above a certain level [13]. To avoid or postpone such complications, it is better to ensure that V T remains as high as possible. Because R100 is capable of delivering comparably greater V T, it may be a better choice for ventilating more severe ARDS patients.
In conclusion, owing to its ability to deliver comparably greater HFOV, R100 may be a better choice for ventilating critical ARDS patients. Better V T proportionality with increasing amplitude may be the result of better titration of amplitude when adjusting PaCO2 during oscillation.
References
Smith RB. Ventilation at high respiratory frequencies. Anaesthesia. 1982;37:1011–8.
Venegas JG, Fredberg JJ. Oscillatory mechanics: the pressure cost of high-frequency ventilation. In: Boynton BR, Carlo WA, Jobe AH, editors. New therapies for neonatal respiratory failure: a physiologic approach. New York: Cambridge University Press; 1994. p. 192–201.
Marchak BE, Thompson WK, Duffty P, Miyaki T, Bryan MH, Bryan AC, Froese AB. Treatment of RDS by high-frequency oscillatory ventilation: a preliminary report. J Pediatr. 1981;99:287–92.
Mehta S, Lapinsky SE, Hallett DC, Merker D, Groll RJ, Cooper AB, MacDonald RJ, Stewart TE. Prospective trial of high-frequency oscillation in adults with acute respiratory distress syndrome. Crit Care Med. 2001;29:1360–9.
Imai Y, Nakagawa S, Ito Y, Kawano T, Slutsky AS, Miyasaka K. Comparison of lung protection strategies using conventional and high-frequency oscillatory ventilation. J Appl Physiol. 2001;91:1836–44.
Courtney SE, Durand DJ, Asselin JM, Hudak ML, Aschner JL, Shoemaker CT. High-frequency oscillatory ventilation versus conventional mechanical ventilation for very-low-birth-weight infants. N Engl J Med. 2002;347:643–52.
Dreyfuss D, Saumon G. Role of tidal volume, FRC, and end-inspiratory volume in the development of pulmonary edema following mechanical ventilation. Am Rev Respir Dis. 1993;148:1194–203.
Muscedere JG, Mullen JB, Gan K, Slutsky AS. Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med. 1994;149:1327–34.
Ranieri VM, Suter PM, Tortorella C, Tullio RD, Dayer JM, Brienza A, Bruno F, Slutsky AS. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA. 1999;282:54–61.
Amato MBP, Barbas CSV, Medeiros DM, Magaldi RB, Schettino GPP, Filho GL, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CRR. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338:347–54.
The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342:1301–8.
Fort P, Farmer C, Westerman J, Johannigman J, Beninati W, Dolan S, Derdak S. High-frequency oscillatory ventilation for adult respiratory distress syndrome: a pilot study. Crit Care Med. 1997;25:937–47.
Derdak S, Mehta S, Stewart TE, Smith T, Rogers M, Buchman TG, Carlin B, Lowson S, Granton J, The Multicenter Oscillatory Ventilation for Acute Respiratory Distress Syndrome Trial (MOAT) Study Investigators. High-frequency oscillatory ventilation for acute respiratory distress syndrome in adults. A randomized, controlled trial. Am J Respir Crit Care Med. 2002;166:801–8.
Mehta S, Granton J, MacDonald RJ, Bowman SD, Matte-Martyn A, Bachman T, Smith T, Stewart TE. High-frequency oscillatory ventilation in adults. Chest. 2004;126:518–27.
Bollen CW, van Well GT, Sherry T, Beale RJ, Shah S, Findlay G, Monchi M, Chiche JD, Weiler N, Uiterwaal CS, van Vught AJ. High frequency oscillatory ventilation compared with conventional mechanical ventilation in adult respiratory distress syndrome: a randomized controlled trial. Crit Care. 2005;9:R430–9.
Ferguson ND, Chiche J-D, Kacmarek RM, Hallett DC, Mehta S, Findlay GP, Granton JT, Slutsky AS, Stewart TE. Combining high-frequency oscillatory ventilation and recruitment maneuvers in adults with early acute respiratory distress syndrome: the treatment with oscillation and an open lung strategy (TOOLS) trial pilot study. Crit Care Med. 2005;33:479–86.
Nagano O, Fujii H, Morimatsu H, Mizobuchi S, Goto K, Katayama H, Hirakawa M, Yamada Y. An adult with ARDS managed with high-frequency oscillatory ventilation and prone position. J Anesth. 2002;16:75–8.
Hatcher D, Watanabe H, Ashbury T, Vincent S, Fisher J, Froese A. Mechanical performance of clinically available, neonatal, high-frequency, oscillatory-type ventilators. Crit Care Med. 1998;26:1081–8.
Hirao O, Iguchi N, Uchiyama A, Mashimo T, Nishimura M, Fujino Y. Influence of endotracheal tube bore on tidal volume during high frequency oscillatory ventilation: a model lung study. Med Sci Monit. 2009;15:M1–4.
Pillow JJ, Neil H, Wilkinson MH, Ramsden CA. Effect of I/E ratio on mean alveolar pressure during high-frequency oscillatory ventilation. J Appl Physiol. 1999;87:407–14.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Iguchi, N., Hirao, O., Uchiyama, A. et al. Evaluation of performance of two high-frequency oscillatory ventilators using a model lung with a position sensor. J Anesth 24, 888–892 (2010). https://doi.org/10.1007/s00540-010-1032-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-010-1032-0