Abstract
Recently, the FLOW-i anaesthesia ventilator was developed based on the SERVO-i intensive care ventilator. The aim of this study was to test the FLOW-i’s tidal volume delivery in the presence of a leak in the breathing circuit. We ventilated a test lung model in volume-, pressure-, and pressure-regulated volume-controlled modes (VC, PC, and PRVC, respectively) with a FLOW-i. First, the circuit remained airtight and the ventilator was tested with fresh gas flows of 6, 1, and 0.3 L/min in VC, PC, and PRVC modes and facing 4 combinations of different resistive and elastic loads. Second, a fixed leak in the breathing circuit was introduced and the measurements repeated. In the airtight system, FLOW-i maintained tidal volume (VT) and circuit pressure at approximately the set values, independently of respiratory mode, load, or fresh gas flow. In the leaking circuit, set VT = 500 mL, FLOW-i delivered higher VTs in PC (about 460 mL) than in VC and PRVC, where VTs were substantially less than 500 mL. Interestingly, VT did not differ appreciably from 6 to 0.3 L/min of fresh air flow among the 3 ventilatory modes. In the absence of leakage, peak inspiratory pressures were similar, while they were 35–45 % smaller in PRVC and VC than in PC mode in the presence of leaks. In conclusion, FLOW-i maintained VT (down to fresh gas flows of 0.3 L/min) to 90 % of its preset value in PC mode, which was 4–5 times greater than in VC or PRVC modes.
Similar content being viewed by others
1 Introduction
New advanced ventilation technologies need to be independently evaluated [1–3]. Recently, important efforts have been made to improve the performance of the ventilators used in the operating room [4–6]. A new anaesthesia ventilator, the FLOW-i (Maquet, Solna, Sweden), has been developed based on the same gas delivery system (gas modules) used in the SERVO-i ventilator, and as such it brings ICU ventilator capabilities into the operating room. The gas modules are microprocessor-controlled flow-generators driven by the pressure exercised by the gas supply. Each gas module has the capacity to deliver a flow up to 200 L/min. Compared to SERVO-i, FLOW-i has two extra gas modules, one for nitrous oxide and one for the re-breathing system, the Volume reflector (VR). The VR is an oxygen-driven 1.2 L rigid reservoir that stores expired gases and replaces bellows and pistons present in other anaesthesia machines. In normal working conditions, the VR is always filled, and its design should guarantee that a certain volume would be delivered to the patient, even in the presence of a circle system leak. Recently some operational characteristics of FLOW-i have been evaluated [7–9], but not regarding a leaking system. We wanted to test this particular aspect of the FLOW-i: how well can the FLOW-i maintain tidal volume delivery in the presence of a circle system leak, and this with different ventilation modes, mechanical loads, and over a wide range of fresh gas flows (down to 0.3 L/min)? The quantitative difference between pressure controlled (PC) and volume controlled (VC) modes in the presence of leakage have been reported for other machines [10, 11], but the effect of pressure regulated volume controlled (PRVC), one of the FLOW-i’s ventilation modes, has not been tested yet in such a condition. Finally, we also aimed to verify if mathematical models could accurately describe experimentally gathered volumes and pressures.
2 Materials and methods
2.1 Equipment
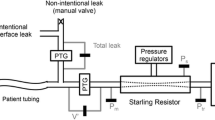
The FLOW-i machine was tested both in airtight and leaking circuit conditions, in two subsequent days in the same operating room under the following working conditions: dry gas, room temperature of 20 °C, relative humidity amounting to 50 %, and positive room pressure (6 Pa) over the ambient pressure. The ventilator was used in accordance to the manufacturer’s instructions and after a pre-use check. The schematic diagram of experimental setup is shown in Fig. 1. Silicone tubing connected inspiratory and expiratory limbs of the ventilator to a Y-piece. A flow sensor (Fleisch pneumotachograph Type 2, Lausanne, Switzerland) was inserted in the inspiratory limb to measure generated airflow \(\left( {{\text{V}}_{1}^{\prime } } \right)\). A filter (Pall Ultipor breathing system filter, Pall Medical, Freiburg, Switzerland) was placed between each limb of the circle breathing system and the ventilator. Distal to the Y-piece, another flow sensor (AWM730B5, Honeywell, Morristown, NJ, USA) \(\left( {{\text{V}}_{2}^{\prime } } \right)\) followed by a filter (Pall Ultipor breathing system filter, Pall Medical, Freiburg, Switzerland) were added to the circuit. The latter was used to simulate one of the most common leakage points at the Y-piece [12, 13] by removing the stopper of the filter. Airflow was measured again (AWM730B5, Honeywell, Morristown, NJ, USA) \(\left( {{\text{V}}_{3}^{\prime } } \right)\) right after the filter. Volumes were calculated by the digital integration of measured airflows: \({\text{V}}_{1}^{\prime }\) yielded the volume generated by the ventilator (VG); \({\text{V}}_{2}^{\prime }\) and \({\text{V}}_{3}^{\prime }\) provided the volumes measured upstream (V2) and downstream of the leakage point (V3), respectively. The latter is, thus, the volume delivered (VD) to the test lung. In the presence of leakage, the difference between V2 and V3 represents the volume lost during inspiration (VLi). Volume leaked during expiration (VLe) is the difference between the volume delivered to the lung model and that returned to the ventilator (VR). A pressure transducer (ASCX01DN, Honeywell, Morristown, NJ, USA) measured pressure (P) through a side-port in the tubing located right before the mechanical lung model.
The test lung ventilated by the FLOW-i was the ACCU LUNG (Fluke Biomedical, Carson City, NV, USA). It allows four combinations of resistances (R), namely, 5 and 20 cmH2O/(L/s) and compliances (C): 20, 50 mL/cmH2O, yielding R5C20, R5C50, R20C20, and R20C50. The loads used in our experiment were very close to those described in healthy anesthetized subjects [14] and similar to those employed in a recent study aiming at modelling restrictive and obstructive conditions [15], as well as in a bench study aiming at evaluating the precision of the delivered tidal volume in VC ventilation [4].
2.2 Experimental protocol
Respiratory frequency was always kept as 12 breaths per minute; I:E ratio corresponded to 1:2. No positive end-expiratory pressure (PEEP) was applied. Under VC and PRVC ventilatory modes VT was set to 500 mL, whereas under PC driving ventilation pressure was set to generate a VT of 500 mL. Ventilatory modes and fresh gas flow delivery (0.3, 1 and 6 L/min) were randomly established. The fresh gas flow composition was 50 % oxygen in air. P and V′ signals were sampled at 2 kHz by a 12-bit National Instruments acquisition board (PCI-6023E, Austin, TX, USA) and stored on a computer for off-line processing. Each combination of ventilatory modes, fresh gas flows and loads was recorded for 1 min. After the first five breaths and during the end-expiratory phase of the sixth cycle, leakage was produced by removing the stopper (ID = 4 mm) of the filter connected to the Y-piece (Fig. 1) and was maintained for the rest of acquisition time (Fig. 2). The stopper was then reinserted and a new experimental combination was tested. After 3 min of stabilization, a new recording period was started. In each experimental condition all tests were repeated three times.
Pressure and flow tracings obtained during PC, VC and PRVC (panel a, b and c respectively) ventilation provided by FLOW-i ventilator. From top to bottom: pressure, airflow measured at the inspiratory line of the ventilator, right before the leakage point, and right before the test lung, respectively. Leakage was introduced during the end-expiratory phase of the sixth breath and flow profiles changed immediately (second arrow). Resistive and elastic loads were R = 5 cmH2O/(L/s) C = 50 mL/cmH2O. Fresh gas flow delivery was set to 0.3 L/min and tidal volume to 500 mL. During leakage after the fifth breath a steady state was reached, as observed in all three flow tracings. Insp, inspiration
Total circuit compliance was 1.64 × 10−3 L/cmH2O, as calculated by the ventilator just before the experimental measurements. Special care was taken to detect circuit and lung model unwanted leakage by closing the adjustable pressure level valve on the FLOW-i. The total circuit was considered airtight when a plateau pressure of 40 cmH2O remained constant for 1 min. This manoeuvre was repeated after every experimental data collection. If leakage was detected, the measurement was repeated.
2.3 Statistical analysis
Mixed-linear effect modelling was used to describe the data [16]. The three ventilatory modes, the three fresh gas flow rates and the four mechanical loads were considered as fixed effects, the triplicate repeated measures as a random effect. We assessed airtight and leaking systems separately. Starting from a maximal model in which all covariates were present, the minimal adequate model in term of parsimony was achieved with a backward stepwise approach and a 5 % significance level. Computation was performed with lme4 package (R software) [17, 18]. Comparison between models was done by parametric bootstrapping [19]. To address multiple comparisons within different levels in fixed-effect factors, Tukey HSD test (multcomp package) was used [20].
3 Results
Measured volumes and pressures, listed as median, minimum and maximum values for R5C50, are presented in Tables 1 and 2, respectively. The tables regarding the other load combinations are available in the supplementary on-line material. The equations resulting from the mixed-effects model regressions are found below. Noteworthy, in all instances, both in airtight and leaking circuits, measured volume and pressure did not depend on fresh gas flow rates. Additionally, the RC product did not significantly influence the modelling.
3.1 Airtight circuit
In the airtight circuit the anaesthesia machine delivered the preset VTs to the lung model in each experimental setting. The mean values (±SEM) under PC, PRVC and VC did not differ and amounted to 504.31 ± 0.59, 504.24 ± 0.74 and 501.64 ± 0.74, respectively.
Peak pressures were inversely correlated with compliance. Pressures during PC, PRVC and VC ventilatory modes presented an identical dependency on C. Eq. (1) resulted from the ensemble data.
3.2 Leaking circuit
In the leaking circuit, the volumes generated (VG) by the ventilator depended solely on C. It did not differ between VC and PRVC, and thus, the results gathered in both modes were taken together and represented by
whereas in PC mode volume differed from the former modes and could be calculated as
The peak pressures varied according to the mechanical loads (both R and C). In PRVC and VC modes, pressure depended similarly on C and, hence, the values were integrated; in PC mode C-dependency of pressure differed statistically from the other modes. Pressure also depended on R to the same extent in the three cases. Thus, the following equations resulted
The volumes delivered to the lung model (VD) depended on C and did not differ significantly between VC and PRVC, which were, then, ensemble, providing
However, they differed from PC mode, where
The volumes leaked during inspiration (VLi) depended solely on C. In PRVC and VC modes the results were similar and the data were joined
They differed from the volumes in PC mode
On the other hand, the leaked volumes during expiration (VLe) depended additionally on R; PRVC and VC modes presented similar results that were, thus, the data were joined
In PC ventilation leaked volumes differed from those in the other two modes, thus
3.3 Determination of mathematical model accuracy
In order to assess accuracy of equations derived by statistical analysis (i.e. mixed-effects linear model) the measured volumes and pressures were plotted against estimated ones using Eqs. (1)–(11) (Fig. 3a, b). The figures show that the measured and calculated values are very similar.
4 Discussion
Leaks in the anaesthesia machine and breathing system account for about 10 % of critical incidents concerning anaesthesia equipment [21, 22]. During low fresh gas flow anaesthesia these leaks should be carefully considered because in some ventilators tidal volume delivery is not guaranteed [23].
In an airtight circuit, the FLOW-i delivers the set VT with all ventilation modes over the fresh gas flow and the tested mechanical load range. When a leak was present distal to the Y-piece, only PC ventilation ensured delivery of the set VT. The mathematical models could accurately describe the experimentally gathered volumes and pressures.
The peak pressure reached in the airtight circuit was inversely correlated to compliance in all three modes (Eq. 1) as expected in isovolumetric conditions. A recent work reports that in VC ventilation without leaks the FLOW-i ventilator delivered around 5–6 % more volume that the set VT (500 mL) [4]. In the present study, we found an error lower than 2 % in delivered volume. The different results could be explained by the diverse experimental setups.
In our study, in the presence of leaks in a breathing system, volume delivered to the lung (VD) model was best maintained in PC mode: 90.4 and 93.1 % (C50 and C20 mL/cmH2O, respectively) of the set tidal volume. On the other hand, in PRVC and VC modes VD decreased to 21.9 and 11.1 % (C50 and C20 mL/cmH2O, respectively) of the set tidal volume. Volumes generated by the ventilator (VG), delivered to the lung, and leaked during inspiration depended on C and on the ventilatory mode. In PC mode VD was similar despite different C (452.41 and 465.61 mL with C50 and C20 mL/cmH2O, respectively), while in PRVC and VC the amount of volume delivered to the lung was 55.72 and 109.42 mL for C20 and C50 mL/cmH2O, respectively. In this study, the PC mode reaches a set pressure because of the extra gas supplied to overcome leaks, irrespective of the set amount of fresh gas flow. In this case, the volume generated by the ventilator (VG) was around 1226 mL, while both in VC and PRVC the VG was around 506 and 532 mL for C50 and C20 mL/cmH2O, respectively. The pressures found in VC and PRVC in a leaking system were always considerably lower than in an airtight circuit in all cases (Table 2 and supplementary material). A similar bench study addressed inspiratory leaks (ID = 3 mm) in pressure- and volume-controlled ventilators comparing different compliances and it found that PC mode could better maintain the delivered volume [11]. The same issue also occurs in ICU devices providing non-invasive ventilation [24]. In this case SERVO-i in PC ventilation mode rapidly responds to leaks of 26–27 L/min, similar to those of the present study, without requiring a setting modification and it maintains 76 % of the preset tidal volume [24].
The results of our study can be explained by the rationale behind each ventilatory mode [25], as well as by the FLOW-i intrinsic gas delivery mechanism. During VC and PRVC the volume is a control variable. In VC mode the tidal volume is preset and the corresponding increase in pressure during inflation depends on the interplay between delivered volume and the respiratory system impedance. PRVC is a dual-control, breath-to-breath mode, with a preset constant VT, and automatic pressure limit related to compliance variations [26]. On the other hand, during PC, the ventilator functions as a pressure controller, and operates in a pressure-limited and time-cycled mode [26]. In PC mode delivery of airflow and tidal volume change according to respiratory system impedance variations. During this ventilatory mode the ventilator will constantly adjust flow so that the inspiratory pressure is maintained during the entire inspiratory time (Fig. 2a) [27]. Thus in the presence of leakage the PC logic responds with an increased flow and volume delivery so as to keep airway pressures close to the target (Fig. 2a). On the contrary, in VC and PRVC flow and volume are maintained close to the preset target and consequently the peak airway pressure decreases (Fig. 2b, c).
However, the capacity to deliver tidal volume in the presence of a leak depends also on the intrinsic mechanism determining gas delivery. The ratio between fresh gas and minute volume determines the re-breathing fraction used by the control system in FLOW-i. The control system activates the gas modules according to gas mixture and re-breathing. At low fresh gas flows the major part of a tidal volume is generated by the reflector gas module. In case of zero re-breathing (i.e. fresh gas flow > minute volume) only the fresh gas modules are active. However, different from other anesthesia machines, FLOW-i’s reflector driving gas can be used in the breathing circuit since no membrane prevents the driving gas (oxygen) to reach the circle system. Thus, by design, tidal volume delivery is not dependent on the set fresh gas flow (Fig. 4). In particular, the volume reflector allows for the circuit to refill and an extra volume delivery in order to compensate the leaks. As a consequence, important clinical variations on halogenate and oxygen concentrations must be carefully considered in a leaking circuit. In all instances, the design of the VR should provide a gas supply with an oxygen concentration up to 100 %.
Schematic overview of FLOW-i’s gas delivery system. Fresh gas flow line is supplied by three gas modules (1—O2, 2—Air and 3—N2O). In the re-breathing line the expired gases are stored in a reflector and its driving gas O2 is supplied by a dedicated gas module (4—O2). The control system activates the gas modules according to gas mixture and re-breathing. AA injector anesthetic agent injector, AGS, Anesthesia gas scavenging, EXP/PEEP/APL expiratory/positive end expiratory pressure/adjustable pressure level
Our study presents some limitations: (1) the equations provided by the mixed-effect model analysis are valid only in the range of used loads; (2) the same restrictions apply to the fresh gas flow range; (3) we used no PEEP and one tidal volume; (4) even if the VR provides an additional pure oxygen supply, in our study we cannot measure circuit O2 variation because the lung model does not consume O2. For the same reason, it does not produce CO2.
In conclusion, in a leaky breathing circuit, FLOW-i in PC mode ensures tidal volume delivery when R and C values are within the human physiological and pathological ranges at all fresh gas flows tested. However, this was not the case in VC and PRVC modes, and, furthermore, they presented similar behaviours. Finally, this study provides predictive linear equations that can be used to compare FLOW-i with other ventilatory machines in the same experimental setting.
References
Jaber S, Tassaux D, Sebbane M, Pouzeratte Y, Battisti A, Capdevilla X, Eledjam JJ, Jolliet P. Performance characteristics of five new anesthesia ventilators and four intensive care ventilators in pressure-support mode. Anesthesiology. 2006;105:944–52.
Thille AW, Lyazidi A, Richard J-CM, Galia F, Brochard L, Groupe de Travail sur les Respirateurs. A bench study of intensive-car-unit ventilators: new versus old and turbine-based versus compressed gas-based ventilators. Intensive Care Med. 2009;35:1368–76.
Takeuchi M, Williams P, Hess D, Kacmarek RM. Continuous positive airway pressure in new-generation mechanical ventilators. A lung model study. Anesthesiology. 2002;96:162–72.
Wallon G, Bonnet A, Guérin C. Delivery of tidal volume from four anaesthesia ventilators during volume-controlled ventilation: a bench study. Br J Anaesth. 2013;110:1045–51.
Bachiller PR, McDonough JM, Feldman JM. Do new anesthesia ventilators deliver small tidal volumes accurately during volume-controlled ventilation? Pediatr Anesthesiol. 2008;106:1392–400.
Nunn G. Low-flow anaesthesia. Contin Educ Anaesth Crit Care Pain. 2008;8:1–4. doi:10.1093/bjaceaccp/mkm052m.
Ghijselings IE, De Cooman S, Carette R, Peyton PJ, De Wolf AM, Hendrickx JF. Performance of an active inspired hypoxic guard. J Clin Monit Comput. 2015;. doi:10.1007/s10877-015-9684-9.
Carette R, De Wolf AM, Hendrickx JF. Automated gas control with the Maquet FLOW-i. J Clin Monit Comput. 2015;. doi:10.1007/s10877-015-9723-6.
Dehouwer A, Carette R, De Ridder S, De Wolf AM, Hendrickx JF. Accuracy of inhaled agent usage displays of automated target control anesthesia machines. J Clin Monit Comput. 2015;. doi:10.1007/s10877-015-9746-z.
Mushin WW, Rendell-Baker L, Thompson PW. Automatic ventilation of the lungs. 3rd ed. London: Blackwell Scientific Publications; 1980. p. 149–51.
Watt JW, Fraser MH. The effect of insufflation leaks upon ventilation. A quantified comparison of ventilators. Anaesthesia. 1994;49:320–3.
Orkin FK. Anesthetic systems. In: Miller RD, editor. Anesthesia. 2nd ed. New York: Churchill Livingstone; 1986. p. 149.
Riutort KT, Brockwell RC, Brull SJ, Andrews JJ. The anesthesia workstation and delivery systems. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Stock MC, editors. Clinical anesthesia. 6th ed. Philadelphia: Lippincott Williams & Wilkins; (2009). p. 677.
Behrakis PK, Higgs BD, Baydur A, Zin WA, Milic-Emili J. Respiratory mechanics during halothane anestesia and anesthesia-paralysis in humans. J Appl Physiol. 1983;55:1085–92.
Lujàn M, Sogo A, Pomares X, Monsó E, Sales B, Blanch L. Effect of leak and breathing pattern on the accuracy of volume estimation by commercial home ventilators: a bench study. Respir Care. 2013;58:770.
Pinheiro JC, Bates DM. Mixed-effects models in S and S-PLUS. New York: Springer; 2000. p. 4–96.
Bates D, Maechler M, Bolker B, Walker S. lme4: linear mixed-effects models using eigen and S4. R package version 1; 2014. pp. 1–7. http://CRAN.R-project.org/package=lme4. Accessed 15 Sep 2014.
R Development Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2012. http://www.R-project.org.Accessed 15 Sep 2014.
Faraway J. Extending the linear model with R: generalized linear, mixed effects and nonparametric regression models. London: Chapman & Hall/CRC; 2005. p. 159.
Hothorn T, Bretz F, Westfall P. Simultaneous inference in general parametric models. Biom J. 2008;50:346–63.
Cassidy CJ, Smith A, Arnot-Smith J. Critical incident reports concerning anaesthetic equipment: analysis of the UK national reporting and learning system (NRLS) data from 2006–2008. Anaesthesia. 2011;66:879–88.
Caplan RA, Vistiva MF, Posner KL, Cheney FW. Adverse anesthetic outcomes arising from gas delivery equipment. A closed claim analysis. Anesthesiology. 1997;87:741–8.
Lampotang S, Sanchez JC, BaiXi C, Graventein N. The effect of a bellows leak in an Ohmeda 7810 Ventilator on room contamination, inspired oxygen, airway pressure and tidal volume. Anesth Analg. 2005;101:151–4.
Ferreira JC, Chipman DW, Hill NS, Kacmarek RM. Bilevel vs ICU ventilators providing nonivasive ventilation: effect of system leaks. A COPD lung model comparison. Chest. 2009;136:448–56.
Guldager H, Nielsen SL, Soerensen MB. A comparison of volume control and pressure-regulated volume control ventilation in acute respiratory failure. Crit Care. 1997;1:75–7.
Tobin MJ. Principles and practice of mechanical ventilation. New York: McGraw Hill Professional; 2012.
Lucangelo U, Bernabè F, Blanch L. Lung mechanics at the bedside: make it simple. Curr Opin Crit Care. 2007;1:64–72.
Acknowledgments
The FLOW-i has been temporarily provided by Maquet for independent research purposes.
Funding
The study was funded exclusively by University of Trieste research funds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Because the measurements involved only the anaesthesia machine and lung test model without affecting patents in anyway, no IRB approval was sought.
Conflicts of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lucangelo, U., Ajčević, M., Accardo, A. et al. FLOW-i ventilator performance in the presence of a circle system leak. J Clin Monit Comput 31, 273–280 (2017). https://doi.org/10.1007/s10877-016-9867-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9867-z