Abstract
Background
Special subtypes of pancreatic cancer, such as acinar cell carcinoma (ACC), adenosquamous carcinoma (ASC), and anaplastic carcinoma of the pancreas (ACP), are rare, and so data on them are limited. Using the C-CAT database, we analyzed clinical and genomic characteristics of patients with these and evaluated differences on comparison with pancreatic ductal adenocarcinoma (PDAC) patients.
Methods
We retrospectively reviewed data on 2691 patients with unresectable pancreatic cancer: ACC, ASC, ACP, and PDAC, entered into C-CAT from June 2019 to December 2021. The clinical features, MSI/TMB status, genomic alterations, overall response rate (ORR), disease control rate (DCR), and time to treatment failure (TTF) on receiving FOLFIRINOX (FFX) or GEM + nab-PTX (GnP) therapy as first-line treatment were evaluated.
Results
Numbers of patients with ACC, ASC, ACP, and PDAC were 44 (1.6%), 54 (2.0%), 25 (0.9%), and 2,568 (95.4%), respectively. KRAS and TP53 mutations were prevalent in ASC, ACP, and PDAC (90.7/85.2, 76.0/68.0, and 85.1/69.1%, respectively), while their rates were both significantly lower in ACC (13.6/15.9%, respectively). Conversely, the rate of homologous recombination-related (HRR) genes, including ATM and BRCA1/2, was significantly higher in ACC (11.4/15.9%) than PDAC (2.5/3.7%). In ASC and ACP, no significant differences in ORR, DCR, or TTF between FFX and GnP were noted, while ACC patients showed a trend toward higher ORR with FFX than GnP (61.5 vs. 23.5%, p = 0.06) and significantly more favorable TTF (median 42.3 vs. 21.0 weeks, respectively, p = 0.004).
Conclusions
ACC clearly harbors different genomics compared with PDAC, possibly accounting for differences in treatment efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer is one of the most lethal malignancies, with a 5-year survival rate of less than 5% [1, 2]. Its incidence has been increasing, and it is now ranked as the world's third leading cause of cancer mortality [3]. Most are cases of pancreatic ductal adenocarcinoma (PDAC), although rare subtypes of pancreatic cancer, such as acinar cell carcinoma (ACC), adenosquamous carcinoma (ASC), and anaplastic carcinoma of the pancreas (ACP, also known as undifferentiated carcinoma), may also be identified. Among all pancreatic cancers, ACC accounts for up to 2% [4,5,6], ASC for 1–4% [7, 8], and ACP for approximately 1% [9, 10]. While the demographics, clinical characteristics, and prognoses associated with these subtypes are reportedly distinct from those of PDAC, information is limited, with very few reports. According to the results of previous phase III trials, for patients with unresectable PDAC and a good performance status, FOLFIRINOX (FFX) (fluorouracil, folinic acid, irinotecan, and oxaliplatin) or gemcitabine plus nab-paclitaxel (GnP) therapy is recommended as first-line chemotherapy [11, 12]. However, the efficacy of these two regimens remains unclear for the rare subtypes.
As genome analysis using next-generation sequencers has become easier in recent years, it has become evident that the types of genomic mutations detected in cancer tissues differ among cancers, and that these mutations show wide-ranging associations with the development, progression, and treatment of cancer. In Japan, the government established a Center for Cancer Genomics and Advanced Therapeutics (C-CAT) in June 2018, which collects genomic and clinical information on all patients in Japan who have received genomic profiling tests to support hospitals for cancer genomic medicine, and it facilitates the appropriate secondary use of centralized information for future innovative research [13, 14].
In PDAC, activating mutations in the KRAS oncogene, and inactivating mutations in tumor suppressor genes such as TP53, SMAD4, and CDKN2A, which are the four major alterations, have been identified [3, 15, 16], and homologous recombination repair (HRR) gene abnormalities such as BRCA1/2 and PALB2, which a subset of them harbors, have attracted attention, accelerating drug discovery for therapeutic targets [17,18,19]. A recent study reported that 42 resected specimens of Japanese PDAC patients underwent targeted sequencing analyses, and BRCA1/2 or PALB2 was detected in 12 (28.6%) cases [20]. Evidence on genomic mutations in rare subtypes of pancreatic cancer from Japan are severely limited, with one report showing BRCA2 mutations found in 3 of 7 ACC patients [21], though no collective reports on ACP or ASC are available. Therefore, promoting genomic analysis and acquiring insights into the rare subtypes of pancreatic cancer should be further encouraged.
Due to their rarity, there have been no prospective trials involving these special subtypes, and so there is no widespread consensus on treatment. In this study, using the Japanese nationwide C-CAT database, we aimed to analyze the clinical and genomic characteristics of patients with unresectable ACC, ASC, and ACP and compare them with PDAC patients to expand our understanding of these rare subtypes and explore effective chemotherapy.
Materials and methods
Study population
We conducted this retrospective observational study using data obtained from the C-CAT database. This national database inclusively aggregates clinical and genomic information on Japanese patients who underwent genomic profiling tests. Namely, basic clinical information such as age, gender, cancer type, pathological diagnosis, and metastatic organs, as well as the chemotherapy regimens given before the genomic profiling test, duration of treatment, best response, occurrence of serious adverse events and information of clinical trials provided by C-CAT. Genomic information includes the genomic variants detected, their variation types, allele frequency and clinical significance, MSI and TMB status. Three genomic profiling tests: OncoGuide™ NCC Oncopanel System (NCC) (Sysmex Co., Ltd., Kobe, Japan), FoundationOne® CDx (F1CDx), and FoundationOne® Liquid CDx (F1L) (Foundation Medicine Inc., Cambridge, USA), have been approved for all solid tumors. Under the National Health Insurance System, patients appropriate for tumor profiling tests include those who have completed or are nearing completion of standard treatment for solid tumors with locally advanced or metastatic disease, and who are considered eligible for chemotherapy after tumor profiling tests. All case data entered from June 2019 to December 2021 for which analysis was available at the time of data update in April 2022 were included. Based on the cancer classification platform OncoTree [22], of all 3,074 cases registered as ‘Pancreas’, 383 cases registered as ‘Cystic Tumor of the Pancreas’ (including Intraductal Papillary Mucinous Neoplasm), ‘Pancreatic Neuroendocrine Carcinoma’, Pancreatic Neuroendocrine Tumor’, ‘Pancreatoblastoma’, ‘Solid pseudopapillary Neoplasm of the Pancreas’, or with unknown histology were excluded. Consequently, the remaining 2,691 cases consisted of those entered as ‘Acinar Cell Carcinoma’, ‘Adenosquamous Carcinoma’, ‘Undifferentiated Carcinoma’, and ‘Pancreatic Adenocarcinoma’ with definite histological diagnosis. This study was approved by the Medical Ethics Review Committee of Kyoto Prefectural University of Medicine (Approval Number: ERB-C-2138) and by the review board of C-CAT (C-CAT Control Number: CDU2021-003N).
Methods
The following background characteristics and categories related to treatment of the patients were collected using standardized data collection procedures: age, sex, Eastern Cooperative Oncology Group performance status (ECOG-PS), pathological diagnosis, smoking history, history of heavy alcohol consumption, tumor profiling tests, sampling methods and locations, metastatic organs, and chemotherapy regimens with treatment lines. For treatment lines, only regimens for unresectable cancer were counted, and neoadjuvant and postoperative chemotherapies were excluded. To evaluate the treatment efficacy, the overall response rate (ORR), disease control rate (DCR), and time to treatment failure (TTF) associated with each regimen were estimated. ORR was defined as the proportion of all enrolled patients showing a complete or partial response, and DCR was defined as the proportion of all enrolled patients showing a complete response, partial response, or stable disease. These were evaluated based on Response Evaluation Criteria In Solid Tumors version 1.1 (RECIST 1.1) as a guide together with response assessed by the physicians. TTF was defined as the date of the start of treatment to that of treatment discontinuation or death due to any cause. Genomic information was accumulated on representative gene mutations associated with pancreatic cancer, the microsatellite instability (MSI) status, and data on the tumor mutation burden (TMB). To evaluate truly targetable genomic mutations, only variants which were assessed as ‘oncogenic’, ‘pathogenic’, ‘likely oncogenic’, and ‘likely pathogenic’ in the clinical annotation of C-CAT findings were extracted, and variants of unknown significance (VUS) were not included. The clinical annotation of C-CAT was based on the Cancer Knowledge Data Base (CKDB) constructed by C-CAT, which accumulates information on gene mutations, drugs, and clinical trials from public genomic medicine-related databases available worldwide [14]. Due to the nature of the database, which is based on data manually entered by each attending physician, some cases were found to have missing data. Therefore, rates for each variable were based on the number of patients with available data, and analyses were performed including patients with fixed data.
Statistical analysis
Fisher’s exact test was used to compare all categorical variables and the ANOVA test with Bonferroni correction was used for continuous variables. TTF was estimated with the 95% confidence interval (CI) using the Kaplan–Meier method and compared by the log-rank test. All statistical tests were two-sided and P < 0.05 was set as the level of significance. Statistical analyses were conducted using JMP® pro 15 (SAS Institute Inc., Cary, NC, USA) and R version 4.1.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Frequency of rare-subtype pancreatic cancers and clinical features
The group of 2,691 patients in this study was composed of 44 patients (1.6%) with ACC, 54 (2.0%) with ASC, 25 (0.9%) with ACP, and 2,568 (95.4%) with PDAC (Fig. 1). Table 1 summarizes the clinical characteristics of all patients according to their cancer types. On grouping together patients with all four tumor types, the mean age was in the early 60 s, with most having ECOG-PS = 0 or 1. No significant differences were noted among the four groups in terms of age, sex, smoking habit, heavy alcohol consumption, ECOG-PS, sampling method, or site of tumor sampling. Among the genomic profiling tests, F1CDx was the most frequently performed in all groups, followed by NCC, with F1L being the least frequent, with significant differences among the four groups. No notable differences were noted in the proportion of lung and peritoneum metastasis, while the difference in lymph node metastasis was close to significance among the four groups. Moreover, liver metastasis was found in 72.2% of ASC patients, being significantly higher compared with that in PDAC patients (49.5%, p < 0.01).
Genomic characteristics
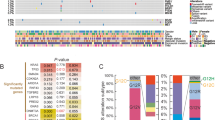
Overall genomic alterations (small-scale variant, deletion, amplification, and rearrangement) with the MSI and TMB status of the four tumor types are shown in Fig. 2a–d, and the top 10 genes in PDAC are compared among the four groups by charts shown in Fig. 3a, b. The list of genes following these frequent gene mutations are presented in Supplemental Table 1. In PDAC patients, the most frequently observed variants were KRAS (85.1%), TP53 (69.1%), CDKN2A (35.4%), and SMAD4 (19.4%). ASC and ACP patients showed similar results, with 90.7 and 76.0% for KRAS, 85.2 and 68.0% for TP53, 51.9 and 40.0% for CDKN2A, and 25.9 and 8.0% for SMAD4, respectively. In contrast, in patients with ACC, KRAS and TP53 were significantly less frequently detected in comparison with the other three tumor types, at 13.6 and 15.9%, respectively (p < 0.01 for TP53 between ACC and ACP, p < 0.001 for the rest). In addition, CDKN2A alteration was found in 25.0% of ACC patients, which was also significantly lower than in ASC (p < 0.001). For more detail regarding KRAS, G12D and G12V were found to be the most common in either group, followed by G12R. G12C, which is well-known for its high detection rate in lung cancer and the recent development of its inhibitor sotorasib [23], was observed only in 2.2% of KRAS mutant PDAC patients, and none in ACC, ASC, and ACP patients (Fig. 3c). The genomic variants which followed the above top 4 variants in PDAC patients were CDKN2B (17.6%), ARID1A (7.1%), STK11 (7.0%), MYC (3.2%), KDM6A (3.0%), and DNMT3A (3.0%). The proportions of these genomic mutations in ACC, ASC, and ACP patients were as follows: CDKN2B (20.5, 29.6, and 36.0%, respectively), ARID1A (9.1, 14.8, and 8.0%, respectively), STK11 (4.6, 14,8, and 4.0%, respectively), MYC (0, 7.4, and 4.0%, respectively), KDM6A (2.3, 5.6, and 4.0%, respectively), and DNMT3A (4.6, 1.9, and 0%, respectively). No differences were observed for these genomic variants.
The frequency of major genomic alterations among rare subtypes of pancreatic cancer and pancreatic ductal adenocarcinoma (PDAC). Data are shown for a top 4 and b 5th-10th gene mutations found in PDAC. c shows the distribution of KRAS subtypes, d and e show the frequencies of the representative homologous recombination repair (HRR) and mismatch repair (MMR) genes among the four tumor types, respectively
Representative HRR gene mutations are shown in Fig. 3d. These genes were chosen based on previous reports [24, 25]. In PDAC patients, the frequencies of ATM, ATR, BRCA1, BRCA2, and PALB2 were 2.5, 0.2, 0.9, 2.9, and 0.9%, respectively. HRR genes were generally less common in ASC and ACP patients, with only 3.7% for BRCA2 in ASC and 4% for PALB2 in ACP. On the other hand, in ACC patients, the rates for ATR and BRCA1 were not high (0 and 2.3%, respectively), while ATM and BRCA2 were 11.4 and 13.6%, respectively, which were both significantly higher compared with PDAC patients (p < 0.05 and p < 0.01, respectively). Thus, 15.9% of ACC patients had BRCA1 or BRCA2, and 25.0% had at least one of these five genes, both of which were markedly more frequent in comparison with PDAC patients. Detailed data on the other 13 HRR genes including BAP1, BARD1, BRIP1, CHEK1/2, RAD51B/C/D, FANCA/C/L, MRE, and NBN, are shown in Supplemental Table 1 (with yellow markers). Considering all these 18 HRR genes, 9.4% of PDAC patients, 25% of ACC patients, 9.3% of ASC patients, and 4.0% of ACP patients had at least one of the HRR genes, showing markedly higher rates in ACC compared with PDAC (p = 0.01).
Data regarding mismatch repair (MMR) gene alterations are presented in Fig. 3e. In PDAC patients, the frequencies of MLH1, MSH2, MSH6, and PMS2 were 0.3, 0.2, 1.6, and 0.04%, respectively. MSH6 was found in 4.6% of ACC patients, 1.9% of ASC patients, and 4.0% of ACP patients. MLH1 was detected in 3.7% of patients with ASC. There were no cases of patients with ACC, ASC, or ACP with MSH2 or PMS2.
Other notable gene mutations besides those mentioned above included BRAF and CTNNB1. BRAF alterations was detected in 15.9% of ACC patients, being significantly higher than that of PDAC (1.7%, p < 0.001). In particular, BRAF fusions were detected in 13.6% of ACC, 0.2% of PDAC, and none of ASC or ACP, indicating that this fusion was present almost exclusively in ACC patients. CTNNB1 was also a frequently detectable gene in ACC (13.6%), compared with PDAC (0.8%), ASC (0%), and ACP (4.0%). PTEN was a variant identified in 7.4% of ASC patients, being significantly more common than in PDAC patients (0.9%, p < 0.05). Furthermore, KMT2D was found in 12.0% of ACP patients, showing a trend toward a higher prevalence than in PDAC (1.8%) (Supplemental Table 1).
Figure 4 shows data on the MSI and TMB status among the four tumor types. These are biomarkers predicting the efficacy of immunotherapy [26, 27]. The proportion of MSI-H was 0.3% in PDAC, compared with 2.6% in ACC, 2.3% in ASC, and 0% in ACP, with no significant differences among the four groups (Fig. 4a). TMB-high (> 10 mutations/Mb) tumors were observed in 1.8% of PDAC, 7.9% of ACC, 2.3% of ASC, and 0% of ACP, with a slightly higher trend in ACC compared with PDAC (p = 0.18) (Fig. 4b). Additionally, the median TMB was 2.51 mutations/Mb for PDAC, 3.99 for ACC, 3.93 for ASC, and 1.78 for ACP, showing no significant difference among the four groups (Fig. 4c).
Treatment response
Table 2 summarizes ORR and DCR of first-line FFX and GnP therapy for each tumor type. Among 1977 PDAC patients, ORRs of FFX and GnP were comparable, at 24.1 and 25.2%, respectively. DCR was 60.3% for FFX and 66.8% for GnP, being significantly higher for the latter (p = 0.006). By contrast, in ACC patients, FFX tended to lead to better ORR compared with GnP, approaching significance (61.5 vs. 23.5%, respectively, p = 0.06). In addition, DCR for FFX was elevated at 76.9%. ASC and ACP showed no noticeable differences in ORR and DCR between these two regimens.
Time to treatment failure
TTF of first-line FFX and GnP in each tumor group is shown in Fig. 5. In PDAC patients, the median TTF for FFX was 28.1 weeks (95%CI 25.0–30.9 weeks) vs. 28.0 weeks (95%CI 26.7–30.7 weeks) for GnP, resulting in very similar Kaplan–Meier curves (Fig. 5a). On the other hand, for patients with ACC, TTF was longer for FFX (median TTF, 42.3 weeks; 95%CI 15.7–189.9 weeks), whereas the median TTF for GnP was 21.0 weeks (95%CI 16.0–29.3 weeks, p = 0.004) (Fig. 5b). ASC patients showed a shorter median TTF on receiving both regimens without any differences; 16.0 weeks (95%CI 7.0–36.0 weeks) for FFX, and 18.1 weeks (95%CI 13.0–24.9 weeks) for GnP. In ACP patients, the median TTF for FFX was not reached (95%CI 40.4 weeks to not reached) and 22.1 weeks (95%CI 8.0–40.9 weeks) for GnP (Fig. 5c, d).
Kaplan–Meier curves of time to treatment failure (TTF) according to first-line FOLFIRINOX (FFX) versus gemcitabine plus nab-paclitaxel (GnP) therapy. Data are shown for a pancreatic ductal adenocarcinoma (PDAC), b acinar cell carcinoma (ACC), c adenosquamous carcinoma (ASC), and d anaplastic carcinoma of pancreas (ACP) patients
Patients with HRR genes have been reported to show a more favorable response to platinum-containing regimens [28, 29]. Thus, we examined TTF of FFX and GnP among ACC patients according to the presence or absence of HRR genes (regarding the five representative genes mentioned in Fig. 3d). Among ACC patients with HRR genes, FFX showed significantly longer TTF compared with GnP (126.3 vs. 25.7 weeks, respectively; p = 0.04, Supplemental Fig. 1a). However, there was also a trend toward longer TTF of FFX compared with GnP in patients without HRR genes, being close to significance (42.3 vs. 20.7 weeks, respectively; p = 0.05, Supplemental Fig. 1b). Furthermore, we evaluated the treatment response by prevalence of BRAF fusion or CTNNB1 mutation, characteristic variants of ACC. Patients with BRAF fusion genes showed a significantly shorter duration of successful chemotherapy compared with those without them (15.7 vs. 30.1 weeks, respectively; p = 0.04, Supplemental Fig. 2a). There was no notable difference in TTF of chemotherapy depending on the presence or absence of CTNNB1 mutation (36.9 vs. 28.1 weeks, respectively; p = 0.74, Supplemental Fig. 2b).
Discussion
Herein, using the Japanese Nationwide Comprehensive Genomic Profiling (CGP) database, we demonstrated the clinical and genomic characteristics of rare subtypes of pancreatic cancer on comparison with PDAC. Among the three rare subtypes, ASC and ACP exhibited relatively similar genomics to PDAC, whereas ACC harbored a clearly different genomic profile. Namely, KRAS, TP53, and CDKN2A, the most typical abnormalities in pancreatic cancer, were present at a low frequency, and other potentially targetable gene alterations, such as HRR genes and BRAF fusion, were more prevalent. This molecular difference may have contributed to the gap in treatment sensitivity between FFX and GnP therapy. Because of their rarity, there are no prospective trials for rare subtypes of pancreatic cancer, and possible effective regimens have only been described in a limited number of retrospective studies and case reports. There are also very few studies that have comprehensively evaluated their genomic profiles. To the best of our knowledge, this is the first report to provide data on the genomic features and clinical benefits of chemotherapy in rare subtypes of pancreatic cancer concurrently, while also exploring the differences from PDAC, based on a large real-world cohort. Another advantage of our study is that we analyzed genomic alterations that were interpreted based on public databases.
Recent studies revealed that ACC is a morphologically and immunohistochemically distinct tumor from PDAC. The low detectability of KRAS, TP53, and CDKN2A was consistent with previous reports, and interestingly, KRAS wild patients were enriched with several non-overlapping actionable genomic alterations [30,31,32]. Comparing these reports with our data, no clear differences in the frequency of genomic alterations among races were found. The high prevalence of ATM and BRCA2, HRR genes known to be markedly sensitive to platinum-containing regimens and PARP inhibitors [28, 29, 33], may explain the better treatment response to FFX compared with GnP in our study. However, contrary to our expectations, better outcomes with FFX were also noted in patients without HRR genes. Takahashi et al. reported that S-1 monotherapy was more effective than Gemcitabine therapy for ACC, indicating that ACC may be highly susceptible to fluoropyrimidine agents [34]. Moreover, consistent with previous reports, BRAF fusions, especially SND-BRAF fusion which activates the MAPK pathway, was highly prevalent and a distinctive alteration in ACC [31]. Based on our review of a small number of cases, these patients showed a poor response to chemotherapy. The MEK inhibitor trametinib may be a therapeutic candidate in this population, since activation of the MAPK pathway was abrogated by MEK inhibition in in vitro experiments. Alterations of CTNNB1, a WNT-β catenin pathway-related gene, were found in a subset of ACC [30, 35]. Although drugs targeting this pathway are still under development, they may become valuable in the future. Liu et al. reported that up to 14% of ACC harbored MSI/defective MMR, which was higher than in PDAC [36, 37]. In our study, MSI-H and TMB-high tumors were marginally more common than PDAC, raising expectations for immunotherapy in this setting, but further accumulation of evidence is warranted.
ASC has been reported to show a greater metastatic potential and be associated with a poorer prognosis compared with PDAC [38,39,40]. In the present study, consistent with these reports, the significantly higher number of liver metastases compared with PDAC was a peculiar finding in this subtype. Genomic involvement has been investigated in several studies to elucidate the clinical behavior of ASC. A recent study conducting genome analysis of clinical samples revealed that ASCs are likely to share the most common genomic mutations including KRAS, TP53, CDKN2A, and SMAD4, with PDACs, which supports the theory that these tumor types are derived from a common lineage [40]. Our data were in line with these reports, and as a side note, the breakdown of KRAS subtypes was also similar to PDAC, with the majority being G12D and G12V followed by G12R. A novel finding was that PTEN, one of the key suppressors of the PI3K/AKT/mTOR pathway, was significantly more altered than PDAC. While the molecular impact of PTEN abnormalities in ASC remains unclear, PI3K inhibitors may play a role in the anti-tumor effect in the future. Nonetheless, as a harsh reality, GnP and FFX therapy for ASC demonstrated comparable but also limited treatment efficacy in this study, which reinforces the results of previous studies [41, 42].
Even less evidence for ACP is available, based on sporadic case reports and a small number of case series. Histologically, ACP is composed of malignant epithelial and mesenchymal elements that do not exhibit specified differentiation [43]. Previous studies reported that, although morphologically distinct, ACP closely resembles PDAC at the molecular level. The possible mechanism of carcinogenesis is as follows: KRAS, TP53, CDKN2A, and SMAD4 mutations cause pancreatic intraepithelial neoplasia (PanIN), a precancerous lesion of PDAC, and epithelial-mesenchymal transition (EMT) occurs during the process of invasive growth of tumor cells, whereby pleiomorphic cells are formed, resulting in the development of ACP [43,44,45,46]. Indeed, our results were in agreement with this, showing a parallel pattern of genomic alterations with PDAC. Of note, there were no MSI-H/TMB-high cases in our ACP cohort. Since no previous reports on the MSI/TMB status exist in this tumor category, further investigation is required. Regarding studies on chemotherapy, Imaoka et al. demonstrated that paclitaxel-containing regimens such as GnP facilitate favorable outcomes in ACP patients [47]. From our results, disease control was also achieved by FFX therapy; however, due to the small number of cases, it is difficult to conclude which is preferable.
The limitations of our study are mainly attributed to the content of the nationwide C-CAT database and the nature of real-world data. First, the cohort was composed of relatively young patients with good PS, since patients who underwent CGP testing were included, which may have resulted in a selection bias. Second, although the study was based on a nationwide database, due to the rarity of the diseases, the numbers of patients with the rare subtypes were low. Third, due to incomplete data entries, the overall survival, the standard measure of the treatment response, was not available and TTF was used instead. Nonetheless, it should be stated that TTF has become increasingly accepted as a practical endpoint for real-world data and is used in various studies [48, 49]. Forth, we could not evaluate somatic and germline mutations separately, since most analyses were performed by F1CDx, which does not distinguish between them. Lastly, the details of treatment, such as drug withdrawal or dose reduction, were not available. However, we believe that our study is valuable in that we performed genomic analysis using common assays across tumor groups, and discussed it along with their clinical characteristics, within the same time period. Moreover, the comprehensiveness of the C-CAT database, which provides information on almost all patients who underwent CGP in Japan, is also a strength of this study.
In conclusion, each tumor category exhibited different clinical and genomic characteristics compared with PDAC, especially ACC, which showed a completely distinct genomic profile and response to chemotherapy. While rare subtypes of pancreatic cancer are usually excluded from clinical trials, the unique genomic alterations found in this study may encourage participation in basket trials. With the growing dissemination of precision medicine, we hope that our results provide some insights into how to treat rare cancers, which remains challenging.
Abbreviations
- PDAC:
-
Pancreatic ductal adenocarcinoma
- ACC:
-
Acinar cell carcinoma
- ASC:
-
Adenosquamous carcinoma
- ACP:
-
Anaplastic carcinoma of the pancreas
- FFX:
-
FOLFIRINOX
- GnP:
-
Gemcitabine plus nab-paclitaxel
- C-CAT:
-
Center for Cancer Genomics and Advanced Therapeutics
- HRR:
-
Homologous recombination repair
- NCC:
-
OncoGuide™ NCC Oncopanel System
- F1CDx:
-
FoundationOne® CDx
- F1L:
-
FoundationOne® Liquid CDx
- ECOG-PS:
-
Eastern Cooperative Oncology Group performance status
- ORR:
-
Overall response rate
- DCR:
-
Disease control rate
- TTF:
-
Time to treatment failure
- MSI:
-
Microsatellite instability
- TMB:
-
Tumor mutation burden
- MMR:
-
Mismatch repair
- CGP:
-
Comprehensive genomic profiling
References
Rawla P, Sunkara T, Gaduputi V. Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World J Oncol. 2019;10:10–27.
Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7–33.
Vincent A, Herman J, Schulick R, et al. Pancreatic cancer. Lancet. 2011;378:607–20.
Matsuno S, Egawa S, Fukuyama S, et al. Pancreatic Cancer Registry in Japan: 20 years of experience. Pancreas. 2004;28:219–30.
Schmidt CM, Matos JM, Bentrem DJ, et al. Acinar cell carcinoma of the pancreas in the United States: prognostic factors and comparison to ductal adenocarcinoma. J Gastrointest Surg. 2008;12:2078–86.
Glazer ES, Neill KG, Frakes JM, et al. Systematic review and case series report of acinar cell carcinoma of the pancreas. Cancer Control. 2016;23:446–54.
Madura JA, Jarman BT, Doherty MG, et al. Adenosquamous carcinoma of the pancreas. Arch Surg. 1999;134:599–603.
Borazanci E, Millis SZ, Korn R, et al. Adenosquamous carcinoma of the pancreas: Molecular characterization of 23 patients along with a literature review. World J Gastrointest Oncol. 2015;7:132–40.
Clark CJ, Graham RP, Arun JS, et al. Clinical outcomes for anaplastic pancreatic cancer: a population-based study. J Am Coll Surg. 2012;215:627–34.
Strobel O, Hartwig W, Bergmann F, et al. Anaplastic pancreatic cancer: presentation, surgical management, and outcome. Surgery. 2011;149:200–8.
Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364:1817–25.
Von Hoff DD, Ervin T, Arena FP, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369:1691–703.
Mukai Y, Ueno H. Establishment and implementation of Cancer Genomic Medicine in Japan. Cancer Sci. 2021;112:970–7.
Kohno T, Kato M, Kohsaka S, et al. C-CAT: The National Datacenter for Cancer Genomic Medicine in Japan. Cancer Discov. 2022;12:2509–15.
Ryan DP, Hong TS, Bardeesy N. Pancreatic adenocarcinoma. N Engl J Med. 2014;371:1039–49.
Rozenblum E, Schutte M, Goggins M, et al. Tumor-suppressive pathways in pancreatic carcinoma. Cancer Res. 1997;57:1731–4.
Pishvaian MJ, Bender RJ, Halverson D, et al. Molecular profiling of patients with pancreatic cancer: initial results from the know your tumor initiative. Clin Cancer Res. 2018;24:5018–27.
Aguirre AJ, Nowak JA, Camarda ND, et al. Real-time genomic characterization of advanced pancreatic cancer to enable precision medicine. Cancer Discov. 2018;8:1096–111.
Lowery MA, Jordan EJ, Basturk O, et al. Real-time genomic profiling of pancreatic ductal adenocarcinoma: potential actionability and correlation with clinical phenotype. Clin Cancer Res. 2017;23:6094–100.
Takeuchi S, Doi M, Ikari N, et al. Mutations in BRCA1, BRCA2, and PALB2, and a panel of 50 cancer-associated genes in pancreatic ductal adenocarcinoma. Sci Rep. 2018;8:8105.
Furukawa T, Sakamoto H, Takeuchi S, et al. Whole exome sequencing reveals recurrent mutations in BRCA2 and FAT genes in acinar cell carcinomas of the pancreas. Sci Rep. 2015;5:8829.
Kundra R, Zhang H, Sheridan R, et al. OncoTree: a cancer classification system for precision oncology. JCO Clin Cancer Inform. 2021;5:221–30.
Hong DS, Fakih MG, Strickler JH, et al. KRAS(G12C) inhibition with sotorasib in advanced solid tumors. N Engl J Med. 2020;383:1207–17.
Pishvaian MJ, Blais EM, Brody JR, et al. Outcomes in patients with pancreatic adenocarcinoma with genetic mutations in DNA damage response pathways: results from the know your tumor program. JCO Precis Oncol. 2019;3:1–10.
Kondo T, Kanai M, Kou T, et al. Association between homologous recombination repair gene mutations and response to oxaliplatin in pancreatic cancer. Oncotarget. 2018;9:19817–25.
Marabelle A, Le DT, Ascierto PA, et al. Efficacy of pembrolizumab in patients with noncolorectal high microsatellite instability/mismatch repair-deficient cancer: results from the phase II KEYNOTE-158 study. J Clin Oncol. 2020;38:1–10.
Sha D, Jin Z, Budczies J, et al. Tumor mutational burden as a predictive biomarker in solid tumors. Cancer Discov. 2020;10:1808–25.
Pokataev I, Fedyanin M, Polyanskaya E, et al. Efficacy of platinum-based chemotherapy and prognosis of patients with pancreatic cancer with homologous recombination deficiency: comparative analysis of published clinical studies. ESMO Open. 2020;5: e000578.
Yadav S, Kasi PM, Bamlet WR, et al. Effect of germline mutations in homologous recombination repair genes on overall survival of patients with pancreatic adenocarcinoma. Clin Cancer Res. 2020;26:6505–12.
Jiao Y, Yonescu R, Offerhaus GJ, et al. Whole-exome sequencing of pancreatic neoplasms with acinar differentiation. J Pathol. 2014;232:428–35.
Chmielecki J, Hutchinson KE, Frampton GM, et al. Comprehensive genomic profiling of pancreatic acinar cell carcinomas identifies recurrent RAF fusions and frequent inactivation of DNA repair genes. Cancer Discov. 2014;4:1398–405.
Jäkel C, Bergmann F, Toth R, et al. Genome-wide genetic and epigenetic analyses of pancreatic acinar cell carcinomas reveal aberrations in genome stability. Nat Commun. 2017;8:1323.
Javle M, Curtin NJ. The role of PARP in DNA repair and its therapeutic exploitation. Br J Cancer. 2011;105:1114–22.
Takahashi H, Ikeda M, Shiba S, et al. Multicenter retrospective analysis of chemotherapy for advanced pancreatic acinar cell carcinoma: potential efficacy of platinum- and irinotecan-containing regimens. Pancreas. 2021;50:77–82.
Abraham SC, Wu TT, Hruban RH, et al. Genetic and immunohistochemical analysis of pancreatic acinar cell carcinoma: frequent allelic loss on chromosome 11p and alterations in the APC/beta-catenin pathway. Am J Pathol. 2002;160:953–62.
Liu W, Shia J, Gönen M, et al. DNA mismatch repair abnormalities in acinar cell carcinoma of the pancreas: frequency and clinical significance. Pancreas. 2014;43:1264–70.
Hu ZI, Shia J, Stadler ZK, et al. Evaluating mismatch repair deficiency in pancreatic adenocarcinoma: challenges and recommendations. Clin Cancer Res. 2018;24:1326–36.
Boyd CA, Benarroch-Gampel J, Sheffield KM, et al. 415 patients with adenosquamous carcinoma of the pancreas: a population-based analysis of prognosis and survival. J Surg Res. 2012;174:12–9.
Moslim MA, Lefton MD, Ross EA, et al. Clinical and histological basis of adenosquamous carcinoma of the pancreas: a 30-year experience. J Surg Res. 2021;259:350–6.
Lenkiewicz E, Malasi S, Hogenson TL, et al. Genomic and epigenomic landscaping defines new therapeutic targets for adenosquamous carcinoma of the pancreas. Cancer Res. 2020;80:4324–34.
Yoshida Y, Kobayashi S, Ueno M, et al. Efficacy of chemotherapy for patients with metastatic or recurrent pancreatic adenosquamous carcinoma: a multicenter retrospective analysis. Pancreatology. 2022. https://doi.org/10.1016/j.pan.2022.09.236.
Brunetti O, Aprile G, Marchetti P, et al. Systemic chemotherapy for advanced rare pancreatic histotype tumors: a retrospective multicenter analysis. Pancreas. 2018;47:759–71.
Yonemasu H, Takashima M, Nishiyama KI, et al. Phenotypical characteristics of undifferentiated carcinoma of the pancreas: a comparison with pancreatic ductal adenocarcinoma and relevance of E-cadherin, alpha catenin and beta catenin expression. Oncol Rep. 2001;8:745–52.
Luchini C, Pea A, Lionheart G, et al. Pancreatic undifferentiated carcinoma with osteoclast-like giant cells is genetically similar to, but clinically distinct from, conventional ductal adenocarcinoma. J Pathol. 2017;243:148–54.
Iacobuzio-Donahue CA. Genetic evolution of pancreatic cancer: lessons learnt from the pancreatic cancer genome sequencing project. Gut. 2012;61:1085–94.
Mattiolo P, Fiadone G, Paolino G, et al. Epithelial-mesenchymal transition in undifferentiated carcinoma of the pancreas with and without osteoclast-like giant cells. Virchows Arch. 2021;478:319–26.
Imaoka H, Ikeda M, Maehara K, et al. Clinical outcomes of chemotherapy in patients with undifferentiated carcinoma of the pancreas: a retrospective multicenter cohort study. BMC Cancer. 2020;20:946.
Blumenthal GM, Gong Y, Kehl K, et al. Analysis of time-to-treatment discontinuation of targeted therapy, immunotherapy, and chemotherapy in clinical trials of patients with non-small-cell lung cancer. Ann Oncol. 2019;30:830–8.
MartínezChanzá N, Xie W, AsimBilen M, et al. Cabozantinib in advanced non-clear-cell renal cell carcinoma: a multicentre, retrospective, cohort study. Lancet Oncol. 2019;20:581–90.
Acknowledgements
The authors would like to thank the patients who participated in this study, and their families and caregivers. They would also like to thank C-CAT for the clinical and genomic data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sakakida, T., Ishikawa, T., Doi, T. et al. Genomic landscape and clinical features of rare subtypes of pancreatic cancer: analysis with the national database of Japan. J Gastroenterol 58, 575–585 (2023). https://doi.org/10.1007/s00535-023-01986-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-023-01986-9