Abstract
Background
Microscopic esophagitis (ME) is common in patients with non-erosive reflux disease (NERD), and dilation of intercellular spaces (DIS) has been regarded as the potential main mechanism of symptom generation. We aimed to compare these histological abnormalities in healthy volunteers (HVs) and patients with erosive esophagitis (EE), NERD, and functional heartburn (FH).
Methods
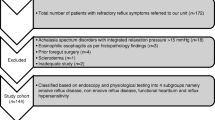
Consecutive patients with heartburn prospectively underwent upper endoscopy and impedance-pH off-therapy. Twenty EE patients and fifty-seven endoscopy-negative patients (NERD), subclassified as 22 with pH-POS (positive for abnormal acid exposure), 20 with hypersensitive esophagus (HE; normal acid/symptom association probability [SAP]+ or symptom index [SI]+), and 15 with FH (normal acid/SAP-/SI-/ proton pump inhibitor [PPI] test-), were enrolled. Twenty HVs were also included. In each patient/control, multiple specimens (n = 5) were taken from the distal esophagus and histological alterations were evaluated. ME was diagnosed when the global histological score was >0.35.
Results
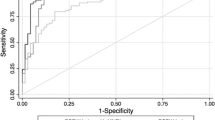
The prevalence of ME was higher (p < 0.0001) in EE (95 %), pH-POS (77 %), and HE (65 %) NERD patients than in FH patients (13 %) and HVs (15 %). Also, basal cell hyperplasia (p < 0.0023), DIS (p < 0.0001), and papillae elongation (p < 0.0002) showed similar rates of prevalence in the above populations (p < 0.0001). ME, including each histological lesion, had similar low frequencies in FH and HVs (p = 0.9990). Considering the histological abnormalities together, they permitted us to clearly differentiate EE and NERD from FH and HVs (p < 0.0001 and p < 0.0001, respectively).
Conclusions
The lack of ME in the esophageal distal biopsies of FH patients indicates a limited role of these histological abnormalities in symptom generation in them. ME can be considered as an accurate and reliable diagnostic marker for distinguishing FH patients from GERD patients and has the potential to be used to guide the correct therapy.






Similar content being viewed by others
Abbreviations
- ME:
-
Microscopic esophagitis
- DIS:
-
Dilation of intercellular spaces
- NERD:
-
Non-erosive reflux disease
- EE:
-
Erosive esophagitis
- HVs:
-
Healthy volunteers
- FH:
-
Functional heartburn
- HE:
-
Hypersensitive esophagus
- SAP:
-
Symptom association probability
- SI:
-
Symptom index
- PPI:
-
Proton pump inhibitor
- GERD:
-
Gastroesophageal reflux disease
- TEM:
-
Transmission electron microscopy
- LM:
-
Light microscopy
- SCJ:
-
Squamocolumnar junction
- BCH:
-
Basal cell hyperplasia
- PE:
-
Papillae elongation
- GS:
-
Global score
- AET:
-
Acid exposure time
- GEE:
-
Generalized estimating equations
- LES:
-
Lower esophageal sphincter
References
Dent J. Microscopic esophageal mucosal injury in nonerosive reflux disease. Clin Gastroenterol Hepatol. 2007;5:4–16.
Tobey NA, Carson JL, Alkiek RA, Orlando RC. Dilated intercellular spaces: a morphological feature of acid-reflux damaged human esophageal epithelium. Gastroenterology. 1996;111:1200–5.
Calabrese C, Fabbri A, Bortolotti M, Cenacchi G, Areni A, Scialpi C, et al. Dilated intercellular spaces as a marker of oesophageal damage: comparative results in gastro-esophageal reflux disease with or without bile reflux. Aliment Pharmacol Ther. 2003;18:525–32.
Caviglia R, Ribolsi M, Maggiano N, Gabbrielli AM, Emerenziani S, Guarino MP, et al. Dilated intercellular spaces of esophageal epithelium in non erosive reflux disease patients with physiological esophageal acid exposure. Am J Gastroenterol. 2005;100:543–8.
Villanacci V, Grigolato PG, Cestari R, Missale G, Cengia G, Klersy C, et al. Dilated intercellular spaces as marker of esophageal reflux: histology, semi-quantitative score and morphometry upon light microscopy. Digestion. 2001;64:1–8.
Zentilin P, Savarino V, Mastracci L, Spaggiari P, Dulbecco P, Ceppa P, et al. Reassessment of the diagnostic value of histology in patients with GERD, using multiple biopsy sites and an appropriate control group. Am J Gastroenterol. 2005;100:2299–306.
van Malestein H, Farrè R, Sifrim D. Esophageal dilated intercellular spaces (DIS) and nonerosive reflux disease. Am J Gastroenterol. 2007;102:1–8.
Savarino E, Zentilin P, Tutuian R, Pohl D, Casa DD, Frazzoni M, et al. The role of non-acid reflux in NERD: lessons learned from impedance-pH monitoring in 150 patients off therapy. Am J Gastroenterol. 2008;103:2685–93.
Galmiche JP, Clouse RE, Bàlint A, Cook IJ, Kahrilas PJ, Paterson WG, et al. Functional esophageal disorders. Gastroenterology. 2006;130:1459–65.
Frazzoni M, Conigliaro R, Mirante VG, Melotti G. The added value of quantitative analysis of on-therapy impedance-pH parameters in distinguishing refractory non-erosive reflux disease from functional heartburn. Neurogastroenterol Motil. 2011. doi:10.1111/j.1365-2982.2011.01800.x.
Savarino E, Pohl D, Zentilin P, Dulbecco P, Sammito G, Sconfienza L, et al. Functional heartburn has more in common with functional dyspepsia than with non-erosive reflux disease. Gut. 2009;58:1185–91.
Carlsson R, Dent J, Bolling-Sternevald E, Johnsson F, Junghard O, Lauritsen K, et al. The usefulness of a structured questionnaire in the assessment of symptomatic gastroesophageal reflux disease. Scand J Gastroenterol. 1998;33:1023–9.
Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–80.
Vakil N, van Zanten SV, Kahrilas P, Dent J. Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–20.
Yerian L, Fiocca R, Mastracci L, et al. Refinement and reproducibility of histologic criteria for the assessment of microscopic lesions in patients with gastroesophageal reflux disease: the Esohisto Project. Dig Dis Sci. 2011;56(9):2656–65.
Fiocca R, Mastracci L, Riddell R, et al. Development of consensus guidelines for the histologic recognition of microscopic esophagitis in patients with gastroesophageal reflux disease: the Esohisto project. Hum Pathol. 2010;41(2):223–31.
Mastracci L, Spaggiari P, Grillo F, Zentilin P, Dulbecco P, Ceppa P, et al. Microscopic esophagitis in gastroesophageal reflux disease: individual lesions, biopsy sampling, and clinical correlations. Virchows Arch. 2009;454:31–9.
Savarino E, Tutuian R, Zentilin P, Dulbecco P, Pohl D, Marabotto E, et al. Characteristics of reflux episodes and symptom association in patients with erosive esophagitis and nonerosive reflux disease: study using combined impedance-pH off therapy. Am J Gastroenterol. 2010;105:1053–61.
Zentilin P, Iiritano E, Dulbecco P, Bilardi C, Savarino E, De Conca S, et al. Normal values of 24-h ambulatory intraluminal impedance combined with pH-metry in subjects eating a Mediterranean diet. Dig Liver Dis. 2006;38:226–32.
Bredenoord AJ, Weusten BL, Smout AJ. Symptom association analysis in ambulatory gastro-oesophageal reflux monitoring. Gut. 2005;54:1810–7.
Vela MF, Camacho-Lobato L, Srinivasan R, Tutuian R, Katz PO, Castell DO. Simultaneous intraesophageal impedance and pH measurement of acid and non-acid gastroesophageal reflux : effect of omeprazole. Gastroenterology. 2001;120:1599–606.
Slaughter JC, Goutte M, Rymer JA, Oranu AC, Schneider JA, Garrett CG, et al. Caution about overinterpretation of symptom indexes in reflux monitoring for refractory gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2011;9(10):868–74.
Smout AJPM. Review article: the measurement of non-acid gastro-oesophageal reflux. Aliment Pharmacol Ther. 2007;26(Suppl 2):7–12.
Viazis N, Keyoglou A, Kanellopoulos AK, Karamanolis G, Vlachogiannakos J, Triantafyllou K, et al. Selective serotonin reuptake inhibitors for the treatment of hypersensitive esophagus: a randomized, double-blind, placebo-controlled study. Am J Gastroenterol. 2011 (Epub ahead of print).
Savarino E, Marabotto E, Zentilin P, Frazzoni M, Sammito G, Bonfanti D, et al. The added value of impedance-pH monitoring to Rome III criteria in distinguishing functional heartburn from non-erosive reflux disease. Dig Liver Dis. 2011;43(7):542–7.
Farré R, Fornari F, Blondeau K, Vieth M, De Vos R, Bisschops R, et al. Acid and weakly acidic solutions impair mucosal integrity of distal exposed and proximal non-exposed human oesophagus. Gut. 2010;59:164–9.
Farrè R, De Vos R, Geboes K, Vanden Berghe P, Depoortere I, Blondeau K, et al. Critical role of stress in increased oesophageal mucosa permeability and dilated intercellular spaces. Gut. 2007;56:1191–7.
Fiocca R, Mastracci L, Engström C, Attwood S, Ell C, Galmiche JP, et al. Long-term outcome of microscopic esophagitis in chronic GERD patients treated with esomeprazole or laparoscopic antireflux surgery in the LOTUS trial. Am J Gastroenterol. 2010;105:1015–23.
Vela MF, Craft BM, Sharma N, Freeman J, Hazen-Martin D. Refractory heartburn: comparison of intercellular space diameter in documented GERD vs functional heartburn. Am J Gastroenterol. 2011;106(5):844–50.
Savarino E, Zentilin P, Tutuian R, Pohl D, Gemignani L, Malesci A, et al. Impedance-pH reflux patterns can differentiate non-erosive reflux disease from functional heartburn patients. J Gastroenterol. 2012;47(2):159–68.
Calabrese C, Bortolotti M, Fabbri A, Areni A, Cenacchi G, Scialpi C, et al. Reversibility of GERD ultrastructural alterations and relief of symptoms after omeprazole treatment. Am J Gastroenterol. 2005;100:537–42.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Savarino, E., Zentilin, P., Mastracci, L. et al. Microscopic esophagitis distinguishes patients with non-erosive reflux disease from those with functional heartburn. J Gastroenterol 48, 473–482 (2013). https://doi.org/10.1007/s00535-012-0672-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-012-0672-2