Abstract
Introduction
Symptom association is important to distinguish non-erosive reflux disease [NERD; abnormal oesophageal acid exposure time (AET) and/or positive symptom association] from functional heartburn (FH; normal AET and negative symptom association). Asymptomatic patients during reflux monitoring are challenging as symptom association cannot be assessed.
Aim
To evaluate whether impedance-pH reflux patterns are useful to differentiate NERD from FH.
Methods
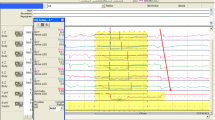
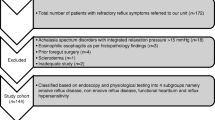
Endoscopy-negative reflux patients underwent impedance-pH off-therapy. Oesophageal AET, characteristics of reflux episodes and symptom association probability (SAP) were measured. Twenty patients asymptomatic during the first test repeated a second examination.
Results
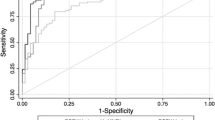
Of 329 patients, 130 (40%) were pH-POS, 120 (36%) pH-NEG/SAP+ (hypersensitive oesophagus = HO) and 79 (24%) pH-NEG/SAP− (FH). Total and acid reflux episodes were significantly higher (p < 0.01) in pH-POS compared to pH-NEG/SAP+, pH-NEG/SAP− and healthy volunteers (HVs). Patients pH-NEG/SAP+ had a significantly increased number of weakly acidic reflux episodes compared to pH-POS, pH-NEG/SAP− and HVs (p < 0.01). The rate of proximal reflux episodes in pH-POS (50%) and pH-NEG/SAP+ (47%) was higher (p < 0.01) than in pH-NEG/SAP− (33%) and HVs (33%). Measuring AET, number of reflux episodes and percentage of proximal reflux events permits to identify FH in 70% of cases and HO in 80% of cases who repeated the examination.
Conclusion
In patients with normal AET and SAP+, increased number of weakly acidic reflux and higher rate of proximal reflux are the main discriminant features. There is large overlap between FH and HVs. These differences can be of help in diagnosing patients with normal oesophageal acid exposure who fail to have symptoms during MII-pH testing.




Similar content being viewed by others
References
Dent J. Pathogenesis of gastro-oesophageal reflux disease and novel options for its therapy. Neurogastroenterol Motil. 2008;20(S1):91–102.
Fass R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol. 2007;41:131–7.
Savarino E, Zentilin P, Tutuian R, Pohl D, Casa DD, Frazzoni M, et al. The role of non-acid reflux in NERD—lessons learned from impedance-pH monitoring in 150 patients off therapy. Am J Gastroenterol. 2008;103:2685–93.
Savarino E, Pohl D, Zentilin P, Dulbecco P, Sammito G, Sconfienza L, et al. Functional heartburn has more in common with functional dyspepsia than with non-erosive reflux disease. Gut. 2009;58:1185–91.
Galmiche JP, Clouse RE, Balint A, Cook IJ, Kahrilas PJ, Paterson WG, et al. Functional esophageal disorders. Gastroenterology. 2006;130:1459–65.
Johnston BT, Lewis SA, Collins JSA, McFarland RJ, Love AH. Acid perception in gastro-oesophageal reflux disease is dependent on psychological factors. Scand J Gastroenterol. 1997;32:974–9.
Broeders JA, Draaisma WA, Bredenoord AJ, de Vries DR, Rijnhart-de Jong HG, Smout AJ, et al. Oesophageal acid hypersensitivity is not a contraindication to Nissen fundoplication. Br J Surg. 2009;96(9):1023–30.
Broeders JA, Bredenoord AJ, Hazebroek EJ, Broeders IA, Gooszen HG, Smout AJ. Effects of anti-reflux surgery on weakly acidic reflux and belching. Gut. 2011;60(4):435–41.
Pandolfino JE, Vela M. Esophageal-reflux monitoring. Gastrointest Endosc. 2009;69:917–30.
Emerenziani S, Sifrim D, Habib FI, Ribolsi M, Guarino MP, Rizzi M. Presence of gas in the refluxate enhances reflux perception in non-erosive patients with physiological acid exposure of the oesophagus. Gut. 2008;57:443–7.
Vakil N, Van Zanten SV, Kahrilas P, Dent J, Jones R, Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–20.
Zentilin P, Iiritano E, Dulbecco P, Bilardi C, Savarino E, De Conca S, et al. Normal values of 24-h ambulatory intraluminal impedance combined with pH-metry in subjects eating a Mediterranean diet. Dig Liver Dis. 2006;38:226–32.
Sifrim D, Castell D, Dent J, Kahrilas PJ. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut. 2004;53:1024–31.
Savarino E, Bazzica M, Zentilin P, Pohl D, Parodi A, Cittadini G, et al. Gastro-esophageal reflux and pulmonary fibrosis in scleroderma: a study using pH-impedance monitoring. Am J Respir Crit Care Med. 2009;179:408–13.
Bredenoord AJ, Weusten BL, Smout AJ. Symptom association analysis in ambulatory gastro-oesophageal reflux monitoring. Gut. 2005;54:1810–7.
Kahrilas PJ, Lin S, Chen J, Manka M. The effect of hiatus hernia on gastro-oesophageal junction pressure. Gut. 1999;44:476–82.
Jones MP, Sloan SS, Rabine JC, Ebert CC, Huang CF, Kahrilas PJ. Hiatal hernia size is the dominant determinant of esophagitis presence and severity in gastroesophageal reflux disease. Am J Gastroenterol. 2001;96:1711–7.
Frazzoni M, De Micheli E, Grisendi A, Savarino V. Hiatal hernia is the key factor in determining the lansoprazole dosage required for effective intra-oesophageal acid suppression. Aliment Pharmacol Ther. 2002;16:881–6.
de Vries DR, Van Herwaarden MA, Smout AJ, Samsom M. Gastroesophageal pressure gradients in gastroesophageal reflux disease: relations with hiatal hernia, body mass index and esophageal acid exposure. Am J Gastroenterol. 2008;103:1349–54.
Savarino E, Gemignani L, Pohl D, Zentilin P, Dulbecco P, Assandri L, et al. Oesophageal motility and bolus transit abnormalities increase in parallel with the severity of GORD. Aliment Pharmacol Ther. 2011;34(4):476–86.
Chen CL, Cook CH. Differences in oesophageal bolus transit between patients with and without erosive reflux disease. Dig Liver Dis. 2008;40:348–54.
Zentilin P, Savarino V, Mastracci L, Spaggiari P, Dulbecco P, Ceppa P, et al. Reassessment of the diagnostic value of histology in patients with GORD, using multiple biopsy sites and an appropriate control group. Am J Gastroenterol. 2005;100:2299–306.
Farré R, van Malenstein H, De Vos R, Geboes K, Depoortere I, Vanden Berghe P, et al. Short exposure of oesophageal mucosa to bile acids, both in acidic and weakly acidic conditions, can impair mucosal integrity and provoke dilated intercellular spaces. Gut. 2008;57:1366–74.
Farré R, Fornari F, Blondeau K, Vieth M, De Vos R, Bisschops R, et al. Acid and weakly acidic solutions impair mucosal integrity of distal exposed and proximal non-exposed human oesophagus. Gut. 2010;59:164–9.
Ribolsi M, Emerenziani S, Caviglia R, Guarino M, Cicala M. Short duration of acid exposure sensitizes the esophagus to perception of weakly acidic and mixed reflux in nonerosive reflux disease (NERD) patients. Gastroenterology. 2008;134(S1):A593.
Frazzoni M, Conigliaro R, Manta R, Melotti G. Weakly acidic reflux have a major role in the pathogenesis of proton pump inhibitor-resistant reflux oesophagitis. Aliment Pharmacol Ther. 2011;33:601–6.
Kanazawa Y, Isomoto H, Wen CY, Wang AP, Saenko VA, Ohtsuru A, et al. Impact of endoscopically minimal involvement on IL-8 mRNA expression in esophageal mucosa of patients with non-erosive reflux disease. World J Gastroenterol. 2003;9:2801–4.
Savarino E, Tutuian R, Zentilin P, Dulbecco P, Pohl D, Marabotto E, et al. Characteristics of reflux episodes and symptom association in patients with erosive esophagitis and nonerosive reflux disease: study using combined impedance-pH off therapy. Am J Gastroenterol. 2010;105:1053–61.
Remes-Troche JM, Carmona-Sanchez R, Gomez-Escudero O, González-Gutiérrez M, Martínez-Salgado J, Ramírez A. Symptom perception with minimal changes on esophageal pH in patients with non-erosive gastroesophageal reflux disease (NERD). Gastroenterology. 2004;126:A-325.
Fass R, Tougas G. Functional heartburn: the stimulus, the pain, and the brain. Gut. 2002;51:885–92.
Watson RGP, Tham TCK, Johnston BT, McDougall NI. Double blind cross-over placebo controlled study of omeprazole in the treatment of patients with reflux symptoms and physiological levels of acid reflux. The ‘sensitive oesophagus’. Gut. 1997;40:587–90.
Trimble KC, Pryde A, Heading RC. Lowered oesophageal sensory thresholds in patients with symptomatic but not excess gastro-oesophageal reflux: evidence for a spectrum of visceral sensitivity in GORD. Gut. 1995;37:7–12.
Bredenoord AJ, Weusten BLAM, Curvers WL, Timmer R, Smout AJ. Determinants of perception of heartburn and regurgitation. Gut. 2006;55:313–8.
Savarino E, Marabotto E, Zentilin P, Frazzoni M, Sammito G, Bonfanti D, et al. The added value of impedance-pH monitoring to Rome III criteria in distinguishing functional heartburn from nonerosive reflux disease. Dig Liver Dis. 2011;43:542–7.
Hershcovici T, Fass R. GERD—are functional heartburn and functional dyspepsia one disorder? Nat Rev Gastroenterol Hepatol. 2010;7(2):71–2.
Savarino E, Zentilin P, Frazzoni M, Cuoco DL, Pohl D, Dulbecco P, et al. Characteristics of gastro-esophageal reflux episodes in Barrett’s esophagus, erosive oesophagitis and healthy volunteers. Neurogastroenterol Motil. 2010;22:1061-e280.
Connor J, Richter J. Increasing yield also increases false positives and best serves to exclude GERD. Am J Gastroenterol. 2006;101:446–52.
Locke GR, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmstead County, Minnesota. Gastroenterology. 1997;112:1448–56.
Labenz J, Jaspersen J, Kulig M, Leodolter A, Lind T, Meyer-Sabellek W, et al. Risk factors for erosive esophagitis; a multivariate analysis based on the ProGERD study initiative. Am J Gastroenterol. 2004;99:1652–6.
Savarino E, Zentilin P, Marabotto E, Bonfanti D, Inferrera S, Assandri L et al. Overweight is a risk factor for both erosive and non-erosive reflux disease. Dig Liver Dis. 2011. doi:10.1016/j.dld.2011.07.014.
Flier SN, Rose S. Is functional dyspepsia of particular concern in women? A review of gender differences in epidemiology, pathophysiologic mechanisms, clinical presentation, and management. Am J Gastroenterol. 2006;101(Suppl 12):S644–53.
Welén K, Faresjö A, Faresjö T. Functional dyspepsia affects women more than men in daily life: a case–control study in primary care. Gend Med. 2008;5:62–73.
Sarnelli G, De Giorgi F, Efficie E, et al. Correlation between oesophageal acid exposure and dyspeptic symptoms in patients with nonerosive reflux disease. Eur J Gastroenterol Hepatol. 2008;20:264–8.
Conflict of interest
The authors declared no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Savarino, E., Zentilin, P., Tutuian, R. et al. Impedance-pH reflux patterns can differentiate non-erosive reflux disease from functional heartburn patients. J Gastroenterol 47, 159–168 (2012). https://doi.org/10.1007/s00535-011-0480-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-011-0480-0