Abstract
Purpose
The aim of this study was to assess the association between sarcopenia and cardiovascular disease (CVD) risk in cancer survivors.
Methods
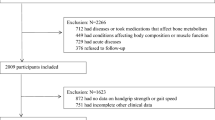
We analyzed a consecutive series of 683 cancer survivors from the Korean National Health and Nutritional Exam Survey (2008–2011 years). Sarcopenia was defined as the appendicular skeletal muscle mass divided by weight (Kg) < 1 standard deviation below the sex-specific healthy population aged 20–39 years. CVD risks were assessed using the Framingham Risk Score (FRS), which were divided by tertile. Predictors of higher shift of FRS tertile by sex were calculated by stratified ordinal logistic regression analyses.
Results
Proportions of sarcopenia were 24.2% in males and 22.5% in females. Sarcopenic survivors were more likely to have a higher body mass index, waist circumference, blood pressure and fasting glucose level, and a lower high-density lipoprotein compared to those without sarcopenia. Sarcopenia was associated with a higher shift of FRS tertile (common odds ratio, 2.67; 95% confidence interval, 1.18–6.52, P < 0.001) in males. However, this association was not significant in female survivors.
Conclusions
Sarcopenia was associated with an increased CVD risk in Korean male cancer survivors. Interventions to prevent sarcopenia may be necessary to improve cardiovascular burden in cancer survivors.

Similar content being viewed by others
References
Adams E, Boulton M, Horne A et al (2014) The effects of pelvic radiotherapy on cancer survivors: symptom profile, psychological morbidity and quality of life. Clin Oncol 26(1):10–17. https://doi.org/10.1016/j.clon.2013.08.003
Moser EC, Meunier F (2014) Cancer survivorship: a positive side-effect of more successful cancer treatment. EJC Suppl 12(1):1–4. https://doi.org/10.1016/j.ejcsup.2014.03.001
McCabe MS, Bhatia S, Oeffinger KC et al (2013) American Society of Clinical Oncology statement: achieving high-quality cancer survivorship care. J Clin Oncol 31(5):631–640. https://doi.org/10.1200/JCO.2012.46.6854
Rugbjerg K, Mellemkjær L, Boice JD, Køber L, Ewertz M, Olsen JH (2014) Cardiovascular disease in survivors of adolescent and young adult cancer: a Danish cohort study, 1943–2009. J Natl Cancer Inst 106(6). https://doi.org/10.1093/jnci/dju110
Gianni L, Herman EH, Lipshultz SE, Minotti G, Sarvazyan N, Sawyer DB (2008) Anthracycline cardiotoxicity: from bench to bedside. J Clin Oncol 26(22):3777–3784. https://doi.org/10.1200/JCO.2007.14.9401
Ewer SM, Ewer MS (2008) Cardiotoxicity profile of trastuzumab. Drug Saf 31(6):459–467. https://doi.org/10.2165/00002018-200831060-00002
Choueiri TK, Mayer EL, Je Y, Rosenberg JE, Nguyen PL, Azzi GR, Bellmunt J, Burstein HJ, Schutz FAB (2011) Congestive heart failure risk in patients with breast cancer treated with bevacizumab. J Clin Oncol 29(6):632–638. https://doi.org/10.1200/JCO.2010.31.9129
Okwuosa TM, Anzevino S, Rao R (2017) Cardiovascular disease in cancer survivors. Postgrad Med J 93(1096):82–90. https://doi.org/10.1136/postgradmedj-2016-134417
Mouridsen H, Keshaviah A, Coates AS, Rabaglio M, Castiglione-Gertsch M, Sun Z, Thürlimann B, Mauriac L, Forbes JF, Paridaens R, Gelber RD, Colleoni M, Smith I, Price KN, Goldhirsch A (2007) Cardiovascular adverse events during adjuvant endocrine therapy for early breast cancer using letrozole or tamoxifen: safety analysis of BIG 1-98 trial. J Clin Oncol 25(36):5715–5722. https://doi.org/10.1200/JCO.2007.12.1665
D’Agostino RB, Vasan RS, Pencina MJ et al (2008) General cardiovascular risk profile for use in primary care. Circulation 117(6):743–753. https://doi.org/10.1161/CIRCULATIONAHA.107.699579
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147(8):755–763. https://doi.org/10.1093/oxfordjournals.aje.a009520
Muscaritoli M, Anker S, Argiles J et al (2010) Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by special interest groups (SIG)“cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr 29(2):154–159. https://doi.org/10.1016/j.clnu.2009.12.004
Lee SJ, Kim NC (2017) Association between sarcopenia and metabolic syndrome in cancer survivors. Cancer Nurs 40(6):479–487. https://doi.org/10.1097/NCC.0000000000000454
Villaseñor A, Ballard-Barbash R, Baumgartner K, Baumgartner R, Bernstein L, McTiernan A, Neuhouser ML (2012) Prevalence and prognostic effect of sarcopenia in breast cancer survivors: the HEAL study. J Cancer Surviv 6(4):398–406. https://doi.org/10.1007/s11764-012-0234-x
Prado CM, Baracos VE, McCargar LJ et al (2009) Sarcopenia as a determinant of chemotherapy toxicity and time to tumor progression in metastatic breast cancer patients receiving capecitabine treatment. Clin Cancer Res 15(8):2920–2926. https://doi.org/10.1158/1078-0432.CCR-08-2242
Fukuda Y, Yamamoto K, Hirao M, Nishikawa K, Nagatsuma Y, Nakayama T, Tanikawa S, Maeda S, Uemura M, Miyake M, Hama N, Miyamoto A, Ikeda M, Nakamori S, Sekimoto M, Fujitani K, Tsujinaka T (2016) Sarcopenia is associated with severe postoperative complications in elderly gastric cancer patients undergoing gastrectomy. Gastric Cancer 19(3):986–993. https://doi.org/10.1007/s10120-015-0546-4
Lauretani F, Russo CR, Bandinelli S, Bartali B, Cavazzini C, di Iorio A, Corsi AM, Rantanen T, Guralnik JM, Ferrucci L (2003) Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol 95(5):1851–1860. https://doi.org/10.1152/japplphysiol.00246.2003
Srikanthan P, Karlamangla AS (2011) Relative muscle mass is inversely associated with insulin resistance and prediabetes. Findings from the third National Health and nutrition examination survey. J Clin Endocrinol Metab 96(9):2898–2903. https://doi.org/10.1210/jc.2011-0435
Karakelides H, Nair KS (2005) Sarcopenia of aging and its metabolic impact. Curr Top Dev Biol 68:123–148. https://doi.org/10.1016/S0070-2153(05)68005-2
Haskell WL, Lee I-M, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A, American College of Sports Medicine, American Heart Association (2007) Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 116(9):1081–1093. https://doi.org/10.1161/CIRCULATIONAHA.107.185649
Schoonen WM, Salinas CA, Kiemeney LA et al (2005) Alcohol consumption and risk of prostate cancer in middle-aged men. Int J Cancer 113(1):133–140. https://doi.org/10.1002/ijc.20528
Kim YS, Lee Y, Chung YS, Lee DJ, Joo NS, Hong D, Song G, Kim HJ, Choi YJ, Kim KM Prevalence of sarcopenia and sarcopenic obesity in the Korean population based on the fourth Korean National Health and nutritional examination surveys. J Gerontol A Biol Sci Med Sci 2012;67(10):1107–1113, DOI: https://doi.org/10.1093/gerona/gls071
Lim S, Kim JH, Yoon JW, Kang SM, Choi SH, Park YJ, Kim KW, Lim JY, Park KS, Jang HC (2010) Sarcopenic obesity: prevalence and association with metabolic syndrome in the Korean longitudinal study on health and aging (KLoSHA). Diabetes Care 33(7):1652–1654. https://doi.org/10.2337/dc10-0107
Ford ES, Giles WH, Mokdad AH (2004) The distribution of 10-year risk for coronary heart disease among US adults: findings from the National Health and Nutrition Examination Survey III. J Am Coll Cardiol 43(10):1791–1796. https://doi.org/10.1016/j.jacc.2003.11.061
Wannamethee SG, Shaper AG, Lennon L, Morris RW (2005) Metabolic syndrome vs Framingham risk score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Arch Intern Med 165(22):2644–2650. https://doi.org/10.1001/archinte.165.22.2644
Bu S, Ruan D, Yang Z, Xing X, Zhao W, Wang N, Xie L, Yang W (2015) Sex-specific prevalence of diabetes and cardiovascular risk factors in the middle-aged population of China: a subgroup analysis of the 2007–2008 China National Diabetes and metabolic disorders study. PLoS One 10(9):e0139039. https://doi.org/10.1371/journal.pone.0139039
Xue B, Johnson AK, Hay M (2013) Sex differences in angiotensin II-and aldosterone-induced hypertension: the central protective effects of estrogen. Am J Physiol Regul Integr Comp Physiol 305(5):R459–R463. https://doi.org/10.1152/ajpregu.00222.2013
Reckelhoff JF (2001) Gender differences in the regulation of blood pressure. Hypertension 37(5):1199–1208. https://doi.org/10.1161/01.HYP.37.5.1199
Kim H, Kim MH, Park YS, Shin JY, Song YM (2015) Factors that predict persistent smoking of cancer survivors. J Korean Med Sci 30(7):853–859. https://doi.org/10.3346/jkms.2015.30.7.853
Park SJ, Kim BC, Han HC, Kim SY, Gwak JI, Lee JK (2009) Effect of cancer diagnosis on smoking behavior. Korean J Fam Med 30(9):681–687. https://doi.org/10.4082/kjfm.2009.30.9.681
Ryan AM, Power DG, Daly L, Cushen SJ, Ní Bhuachalla Ē, Prado CM (2016) Cancer-associated malnutrition, cachexia and sarcopenia: the skeleton in the hospital closet 40 years later. Proc Nutr Soc 75(2):199–211. https://doi.org/10.1017/S002966511500419X
Florin TA, Fryer GE, Miyoshi T, Weitzman M, Mertens AC, Hudson MM, Sklar CA, Emmons K, Hinkle A, Whitton J, Stovall M, Robison LL, Oeffinger KC (2007) Physical inactivity in adult survivors of childhood acute lymphoblastic leukemia: a report from the childhood cancer survivor study. Cancer Epidemiol Biomark Prev 16(7):1356–1363. https://doi.org/10.1158/1055-9965.EPI-07-0048
Plata-Salamán CR, Oomura Y, Kai Y (1988) Tumor necrosis factor and interleukin-1β: suppression of food intake by direct action in the central nervous system. Brain Res 448(1):106–114. https://doi.org/10.1016/0006-8993(88)91106-7
Lang CH, Frost RA, Nairn AC, MacLean DA, Vary TC (2002) TNF-α impairs heart and skeletal muscle protein synthesis by altering translation initiation. Am J Physiol Endocrinol Metab 282(2):E336–E347. https://doi.org/10.1152/ajpendo.00366.2001
Janssen I, Heymsfield SB, Wang Z, Ross R (2000) Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J Appl Physiol 89(1):81–88. https://doi.org/10.1152/jappl.2000.89.1.81
Wallengren O, Iresjö B-M, Lundholm K, Bosaeus I (2015) Loss of muscle mass in the end of life in patients with advanced cancer. Support Care Cancer 23(1):79–86. https://doi.org/10.1007/s00520-014-2332-y
Walrand S, Guillet C, Salles J, Cano N, Boirie Y (2011) Physiopathological mechanism of sarcopenia. Clin Geriatr Med 27(3):365–385. https://doi.org/10.1016/j.cger.2011.03.005
Saidi O, Malouche D, O'Flaherty M, Ben Mansour N, A Skhiri H, Ben Romdhane H, Bezdah L (2016) Assessment of cardiovascular risk in Tunisia: applying the Framingham risk score to national survey data. BMJ Open 6(11):e009195. https://doi.org/10.1136/bmjopen-2015-009195
Kim YJ, Kim CH, Meta SSJ (2002) Analysis for the relation between Korean dietary factors and stomach cancer. J Korean Acad Fam Med 23(9):1098–1106
He J, Gu D, Chen J, Jaquish CE, Rao DC, Hixson JE, Chen JC, Duan X, Huang JF, Chen CS, Kelly TN, Bazzano LA, Whelton PK, GenSalt Collaborative Research Group (2009) Gender difference in blood pressure responses to dietary sodium intervention in the GenSalt study. J Hypertens 27(1):48–54. https://doi.org/10.1097/HJH.0b013e328316bb87
Sakuramoto S, Sasako M, Yamaguchi T, Kinoshita T, Fujii M, Nashimoto A, Furukawa H, Nakajima T, Ohashi Y, Imamura H, Higashino M, Yamamura Y, Kurita A, Arai K, ACTS-GC Group (2007) Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med 357(18):1810–1820. https://doi.org/10.1056/NEJMoa072252
Yu SC, Khow KS, Jadczak AD et al (2016) Clinical screening tools for sarcopenia and its management. Curr Gerontol Geriatr Res 2016:1–10. https://doi.org/10.1155/2016/5978523
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E, Vandewoude M, Zamboni M, European Working Group on Sarcopenia in Older People (2010) Sarcopenia: European consensus on definition and diagnosis report of the European working group on sarcopenia in older people. Age Ageing 39(4):412–423. https://doi.org/10.1093/ageing/afq034
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was conducted solely using a de-identified research dataset, with approval of exemption from review by the Institutional Board and Ethics Committee (IRB number 2017-23).
Informed consent
Informed consent was not required for this study, given the use of secondary data that contained no patient identifiers.
Rights and permissions
About this article
Cite this article
Lee, S.J., Park, Y.J. & Cartmell, K.B. Sarcopenia in cancer survivors is associated with increased cardiovascular disease risk. Support Care Cancer 26, 2313–2321 (2018). https://doi.org/10.1007/s00520-018-4083-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4083-7