Abstract
Background
This study aimed to compare the prevalence of sarcopenia according to the old and new Asian Working Group on Sarcopenia (AWGS) operational criteria and explore the effects of sarcopenia on adverse outcomes in older adults with type 2 diabetes (T2D).
Methods
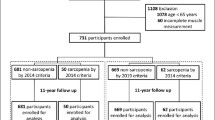
A total of 386 patients with T2D aged ≥ 60 years were recruited in retrospective cohort study. Sarcopenia was assessed with different versions of the AWGS consensus, including the AWGS2014, AWGS2019H (muscle mass adjusted for height), and AWGS2019B (muscle mass adjusted for body mass index). The median follow-up period was 47 months. The composite primary endpoint was the first occurrence of cardiovascular disease (CVD), fragility fracture, and all-cause mortality and the secondary outcomes included the three separate components of the primary outcome.
Results
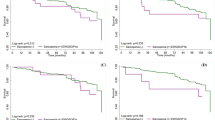
In this study, the prevalence of sarcopenia under different criteria was significantly different, with AWGS2019H having the highest prevalence of 31.3%. The agreement among sarcopenia criteria was unsatisfactory. By Cox regression analysis, all three AWGS definitions of sarcopenia were associated with the composite outcome of all-cause mortality, fracture and CVD (hazard ratio [HR], 2.69 vs. HR, 2.63; vs. HR, 2.23; model 3). Further exploratory analysis, sarcopenia defined by the AWGS2019H criteria was an independent risk factor for death, incident CVD, and fractures. While AWGS2014 criteria was an increased risk factor of death and CVD. The AWGS2019B criteria were only associated with incident fractures.
Conclusion
All three AWGS definitions of sarcopenia were associated the composite primary endpoint. Additionally, the AWGS2019H criteria may be a better independent risk factor for negative health outcomes.

Similar content being viewed by others
Data availability
Participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
References
Dal Canto E, Ceriello A, Rydén L et al (2019) Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol. https://doi.org/10.1177/2047487319878371
Sun H, Saeedi P, Karuranga S et al (2022) IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. https://doi.org/10.1016/j.diabres.2021.109119
American Diabetes Association (2019) 12 Older adults: standards of medical care in diabetes-2019. Diabetes Care. https://doi.org/10.2337/dc19-S012
Kirkman MS, Briscoe VJ, Clark N et al (2012) Diabetes in older adults. Diabetes Care 35:2650–2664. https://doi.org/10.2337/dc12-1801
Liccini A, Malmstrom TK (2016) Frailty and Sarcopenia as predictors of adverse health outcomes in persons with diabetes mellitus. J Am Med Dir Assoc 17:846–851. https://doi.org/10.1016/j.jamda.2016.07.007
Rosenberg IH (2011) Sarcopenia: origins and clinical relevance. Clin Geriatr Med 27:337–339. https://doi.org/10.1016/j.cger.2011.03.003
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European working group on Sarcopenia in older people. Age Ageing 39:412–423. https://doi.org/10.1093/ageing/afq034
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis [published correction appears in Age Ageing. Age Ageing 48:16–31. https://doi.org/10.1093/ageing/afy169
Chen LK, Liu LK, Woo J et al (2014) Sarcopenia in Asia: consensus report of the Asian working group for Sarcopenia. J Am Med Dir Assoc 15:95–101. https://doi.org/10.1016/j.jamda.2013.11.025
Fielding RA, Vellas B, Evans WJ et al (2011) Sarcopenia: an undiagnosed condition in older adults. Current consensus definition prevalence etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 12:249–256. https://doi.org/10.1016/j.jamda.2011.01.003
Zanker J, Scott D, Reijnierse EM et al (2019) Establishing an operational definition of sarcopenia in australia and new zealand: delphi method based consensus statement. J Nutr Health Aging 23:105–110. https://doi.org/10.1007/s12603-018-1113-6
Cruz-Jentoft AJ, Sayer AA (2019) Sarcopenia [published correction appears in Lancet. Lancet 393:2636–2646. https://doi.org/10.1016/S0140-6736(19)31138-9
Izzo A, Massimino E, Riccardi G et al (2021) A Narrative review on sarcopenia in type 2 diabetes mellitus: prevalence and associated factors. Nutrients. 13:183. https://doi.org/10.3390/nu13010183
Park S, Kim SH, Shin JY (2021) Combined association of skeletal muscle mass and grip strength with cardiovascular diseases in patients with type 2 diabetes. J Diabetes 13:1015–1024. https://doi.org/10.1111/1753-0407.13216
Hamasaki H, Kawashima Y, Katsuyama H et al (2017) Association of handgrip strength with hospitalization, cardiovascular events, and mortality in Japanese patients with type 2 diabetes. Sci Rep 7:7041. https://doi.org/10.1038/s41598-017-07438-8
Miyake H, Kanazawa I, Tanaka KI et al (2019) Low skeletal muscle mass is associated with the risk of all-cause mortality in patients with type 2 diabetes mellitus. Ther Adv Endocrinol Metab. https://doi.org/10.1177/2042018819842971
Liu P, Hao Q, Hai S et al (2017) Sarcopenia as a predictor of all-cause mortality among community-dwelling older people: A systematic review and meta-analysis. Maturitas 103:16–22. https://doi.org/10.1016/j.maturitas.2017.04.007
Kelley GA, Kelley KS (2017) Is sarcopenia associated with an increased risk of all-cause mortality and functional disability? Exp Gerontol 96:100–103. https://doi.org/10.1016/j.exger.2017.06.008
Beaudart C, Zaaria M, Pasleau F et al (2017) Health outcomes of Sarcopenia: a systematic review and meta-analysis. PLoS One. 12:e0169548. https://doi.org/10.1371/journal.pone.0169548
Safiri S, Ayubi E (2017) Sarcopenia based on the Asian working Group for Sarcopenia criteria and all-cause mortality risk in older Japanese adults: Methodological issues. Geriatr Gerontol Int 17:1759–1760. https://doi.org/10.1111/ggi.13092
Kim JH, Lim S, Choi SH et al (2014) Sarcopenia: an independent predictor of mortality in community-dwelling older Korean men. J Gerontol A Biol Sci Med Sci 69:1244–1252. https://doi.org/10.1093/gerona/glu050
Woo J, Leung J, Morley JE (2015) Defining sarcopenia in terms of incident adverse outcomes. J Am Med Dir Assoc 16:247–252. https://doi.org/10.1016/j.jamda.2014.11.013
Chen LK, Woo J, Assantachai P et al (2020) Asian working group for sarcopenia: 2019 consensus update on Sarcopenia diagnosis and treatment. J Am Med Dir Assoc 21:300-307.e2. https://doi.org/10.1016/j.jamda.2019.12.012
Sun L, Fu J, Mu Z et al (2023) Association between body fat and sarcopenia in older adults with type 2 diabetes mellitus: A cross-sectional study. Front Endocrinol (Lausanne). https://doi.org/10.3389/fendo.2023.1094075
Takahashi F, Hashimoto Y, Kaji A et al (2021) Sarcopenia is associated with a risk of mortality in people with type 2 diabetes mellitus. Front Endocrinol (Lausanne). https://doi.org/10.3389/fendo.2021.783363
Young BA, Lin E, Von Korff M et al (2008) Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care 14:15–23
McHugh ML (2012) Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 22:276–282
Xia L, Zhao R, Wan Q et al (2020) Sarcopenia and adverse health-related outcomes: an umbrella review of meta-analyses of observational studies. Cancer Med 9:7964–7978. https://doi.org/10.1002/cam4.3428
Huang P, Luo K, Xu J et al (2021) Sarcopenia as a risk factor for future hip fracture: a meta-analysis of prospective cohort studies. J Nutr Health Aging 25:183–188. https://doi.org/10.1007/s12603-020-1474-5
Xu J, Wan CS, Ktoris K et al (2022) Sarcopenia is associated with mortality in adults: a systematic review and meta-analysis. Gerontology 68:361–376. https://doi.org/10.1159/000517099
Chen X, Cao M, Liu M et al (2022) Association between sarcopenia and cognitive impairment in the older people: a meta-analysis. Eur Geriatr Med 13:771–787. https://doi.org/10.1007/s41999-022-00661-1
Petermann-Rocha F, Chen M, Gray SR et al (2020) New versus old guidelines for sarcopenia classification: what is the impact on prevalence and health outcomes? Age Ageing 49:300–304. https://doi.org/10.1093/ageing/afz126
Kitamura A, Seino S, Abe T et al (2021) Sarcopenia: prevalence, associated factors, and the risk of mortality and disability in Japanese older adults. J Cachexia Sarcopenia Muscle 12:30–38. https://doi.org/10.1002/jcsm.12651
Yu R, Leung J, Woo J (2014) Incremental predictive value of sarcopenia for incident fracture in an elderly Chinese cohort: results from the osteoporotic fractures in Men (MrOs) study. J Am Med Dir Assoc 15:551–558. https://doi.org/10.1016/j.jamda.2014.02.005
Wong BW, Thu WPP, Chan YH et al (2023) Association of sarcopenia with important health conditions among community-dwelling Asian women. PLoS One. https://doi.org/10.1371/journal.pone.0281144
Kinoshita K, Satake S, Matsui Y et al (2021) Quantifying muscle mass by adjusting for body mass index is the best for discriminating low strength and function in Japanese older outpatients. J Nutr Health Aging 25:501–506. https://doi.org/10.1007/s12603-020-1557-3
Moon JH, Kim KM, Kim JH et al (2016) Predictive values of the new Sarcopenia index by the foundation for the national institutes of health Sarcopenia project for mortality among older Korean adults. PLoS One. 11:e0166344. https://doi.org/10.1371/journal.pone.0166344
Studenski SA, Peters KW, Alley DE et al (2014) The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci 69:547–558. https://doi.org/10.1093/gerona/glu010
Motamed N, Ajdarkosh H, Darkahian M et al (2020) 10-year risk of cardiovascular disease and body mass index in association with the obesity paradox. ARYA Atheroscler 16:16–23. https://doi.org/10.22122/arya.v16i1.1581
Acknowledgements
We would like to thank the patients and the research team for their participation in this study.
Funding
No funding was received for this paper.
Author information
Authors and Affiliations
Contributions
BZ: designed the study, interpreted the data and critically revised the manuscript for important intellectual content. XY, FC, SK, and YL collected the data. WT, KL, MM, LG, and RL assisted with the data collection. XY and FC analysed the data and wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The study protocol conformed to the Declaration of Helsinki and was approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University (No. 2021–299).
Human and animal rights
The present study is an observational cohort study with human subjects. All methods in this study were conducted in accordance with the amended Declaration of Helsinki.
Informed consent
Informed consent was obtained from all participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ye, X., Chuan, F., Li, Y. et al. Comparing the prognostic value of the old and new sarcopenia criteria from the Asian Working Group on Sarcopenia in older adults with type 2 diabetes: Which set is more appropriate?. Aging Clin Exp Res 35, 1917–1926 (2023). https://doi.org/10.1007/s40520-023-02473-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02473-0