Abstract
Background
Neurolytic celiac plexus block (NCPB) is a safe and effective method for reducing abdominal cancer pain. However, the analgesic efficacy of NCPB is not always guaranteed. The aim of this retrospective study was to identify predictors for the analgesic efficacy of NCPB in patients with unresectable pancreatic cancer.
Methods
Patients with unresectable pancreatic cancer who underwent NCPB from 2006 to 2015 were enrolled. Good analgesia after NCPB was defined as ≥ 50% reduction in pain score at day 30. Patient demographics, cancer characteristics, and pain-related factors were evaluated using a logistic regression analysis to identify predictors for good analgesia after NCPB. Additionally, survival outcomes were compared between patients with poor and good analgesia after NCPB.
Results
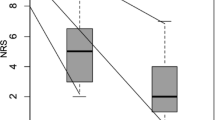
A total of 112 patients satisfied the study protocol requirements. Forty-seven patients (41.9%) showed good analgesia after NCPB. Better performance status, lower serum CA 19-9 level, shorter pain duration, and lower opioid dose were observed in patients with good analgesia after NCPB. Good performance status (ECOG performance status 1 vs. 2 or 3, OR = 2.737, 95% CI = 1.149 to 6.518, P = 0.023) and low daily opioid use (< 150 vs. ≥ 150 mg, OR = 2.813, 95% CI = 1.159 to 6.831, P = 0.022) before NCPB were independent predictors of good analgesia after NCPB. The median survival was significantly lower for patients with poor analgesia after NCPB (68 vs. 150 days, P < 0.001).
Conclusion
NCPB should be offered early to selected patients to improve its analgesic efficacy in advance of deterioration from disease and pain in this population.


Similar content being viewed by others
References
Kamisawa T, Wood LD, Itoi T, Takaori K (2016) Pancreatic cancer. Lancet 388(10039):73–85. https://doi.org/10.1016/S0140-6736(16)00141-0
Wyse JM, Carone M, Paquin SC, Usatii M, Sahai AV (2011) Randomized, double-blind, controlled trial of early endoscopic ultrasound-guided celiac plexus neurolysis to prevent pain progression in patients with newly diagnosed, painful, inoperable pancreatic cancer. J Clin Oncol 29(26):3541–3546. https://doi.org/10.1200/JCO.2010.32.2750
Yan BM, Myers RP (2007) Neurolytic celiac plexus block for pain control in unresectable pancreatic cancer. Am J Gastroenterol 102(2):430–438. https://doi.org/10.1111/j.1572-0241.2006.00967.x
Wong GY, Schroeder DR, Carns PE, Wilson JL, Martin DP, Kinney MO, Mantilla CB, Warner DO (2004) Effect of neurolytic celiac plexus block on pain relief, quality of life, and survival in patients with unresectable pancreatic cancer: a randomized controlled trial. JAMA 291(9):1092–1099. https://doi.org/10.1001/jama.291.9.1092
Bahn BM, Erdek MA (2013) Celiac plexus block and neurolysis for pancreatic cancer. Curr Pain Headache Rep 17(2):310. https://doi.org/10.1007/s11916-012-0310-y
Zhong W, Yu Z, Zeng JX, Lin Y, Yu T, Min XH, Yuan YH, Chen QK (2014) Celiac plexus block for treatment of pain associated with pancreatic cancer: a meta-analysis. Pain Pract 14(1):43–51. https://doi.org/10.1111/papr.12083
Eisenberg E, Carr DB, Chalmers TC (1995) Neurolytic celiac plexus block for treatment of cancer pain: a meta-analysis. Anesth Analg 80(2):290–295
Erdek MA, Halpert DE, Gonzalez Fernandez M, Cohen SP (2010) Assessment of celiac plexus block and neurolysis outcomes and technique in the management of refractory visceral cancer pain. Pain Med 11(1):92–100. https://doi.org/10.1111/j.1526-4637.2009.00756.x
Iwata K, Yasuda I, Enya M, Mukai T, Nakashima M, Doi S, Iwashita T, Tomita E, Moriwaki H (2011) Predictive factors for pain relief after endoscopic ultrasound-guided celiac plexus neurolysis. Dig Endosc 23(2):140–145. https://doi.org/10.1111/j.1443-1661.2010.01046.x
De Cicco M, Matovic M, Bortolussi R, Coran F, Fantin D, Fabiani F, Caserta M, Santantonio C, Fracasso A (2001) Celiac plexus block: injectate spread and pain relief in patients with regional anatomic distortions. Anesthesiology 94(4):561–565. https://doi.org/10.1097/00000542-200104000-00006
Rykowski JJ, Hilgier M (2000) Efficacy of neurolytic celiac plexus block in varying locations of pancreatic cancer: influence on pain relief. Anesthesiology 92(2):347–354. https://doi.org/10.1097/00000542-200002000-00014
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative STROBE (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370(9596):1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X
Bilimoria KY, Bentrem DJ, Ko CY, Ritchey J, Stewart AK, Winchester DP, Talamonti MS (2007) Validation of the 6th edition AJCC pancreatic cancer staging system: report from the National Cancer Database. Cancer 110(4):738–744. https://doi.org/10.1002/cncr.22852
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5(6):649–655. https://doi.org/10.1097/00000421-198212000-00014
Berdine HJ, Nesbit SA (2006) Equianalgesic dosing of opioids. J Pain Palliat Care Pharmacother 20(4):79–84. https://doi.org/10.1080/J354v20n04_16
Sørensen JB, Klee M, Palshof T, Hansen HH (1993) Performance status assessment in cancer patients. An inter-observer variability study. Br J Cancer 67(4):773–775. https://doi.org/10.1038/bjc.1993.140
Huang PI, Chao Y, Li CP, Lee RC, Chi KH, Shiau CY, Wang LW, Yen SH (2009) Efficacy and factors affecting outcome of gemcitabine concurrent chemoradiotherapy in patients with locally advanced pancreatic cancer. Int J Radiat Oncol Biol Phys 73(1):159–165. https://doi.org/10.1016/j.ijrobp.2008.04.012
Tas F, Sen F, Odabas H, Kılıc L, Keskın S, Yıldız I (2013) Performance status of patients is the major prognostic factor at all stages of pancreatic cancer. Int J Clin Oncol 18(5):839–846. https://doi.org/10.1007/s10147-012-0474-9
Lin CC, Lai YL, Ward SE (2003) Effect of cancer pain on performance status, mood states, and level of hope among Taiwanese cancer patients. J Pain Symptom Manag 25(1):29–37. https://doi.org/10.1016/S0885-3924(02)00542-0
Fujii-Lau LL, Bamlet WR, Eldrige JS, Chari ST, Gleeson FC, Abu Dayyeh BK, Clain JE, Pearson RK, Petersen BT, Rajan E, Topazian MD, Vege SS, Wang KK, Wiersema MJ, Levy MJ (2015) Impact of celiac neurolysis on survival in patients with pancreatic cancer. Gastrointest Endosc 82(1):46–56. https://doi.org/10.1016/j.gie.2014.12.036
Smith HS, Mohsin I (2013) Painful boney metastases. Korean J Pain 26(3):223–241. https://doi.org/10.3344/kjp.2013.26.3.223
Kim SH, Yoon DM, Choi KW, Yoon KB (2013) High-dose daily opioid administration and poor functional status intensify local anesthetic injection pain in cancer patients. Pain Physician 16(3):E247–E256
Tunks ER, Weir R, Crook J (2008) Epidemiologic perspective on chronic pain treatment. Can J Psychiatr 53(4):235–242. https://doi.org/10.1177/070674370805300404
Kurita GP, Lundorff L, Pimenta CA, Sjøgren P (2009) The cognitive effects of opioids in cancer: a systematic review. Support Care Cancer 17(1):11–21. https://doi.org/10.1007/s00520-008-0497-y
Nakai Y, Kawabe T, Isayama H, Sasaki T, Yagioka H, Yashima Y, Kogure H, Arizumi T, Togawa O, Ito Y, Matsubara S, Hirano K, Sasahira N, Tsujino T, Tada M, Omata M (2008) CA 19-9 response as an early indicator of the effectiveness of gemcitabine in patients with advanced pancreatic cancer. Oncology 75(1-2):120–126. https://doi.org/10.1159/000155213
Szkandera J, Stotz M, Absenger G, Stojakovic T, Samonigg H, Kornprat P, Schaberl-Moser R, AlZoughbi W, Lackner C, Ress AL, Seggewies FS, Gerger A, Hoefler G, Pichler M (2014) Validation of C-reactive protein levels as a prognostic indicator for survival in a large cohort of pancreatic cancer patients. Br J Cancer 110(1):183–188. https://doi.org/10.1038/bjc.2013.701
McGreevy K, Hurley RW, Erdek MA, Aner MM, Li S, Cohen SP (2013) The effectiveness of repeat celiac plexus neurolysis for pancreatic cancer: a pilot study. Pain Pract 13(2):89–95. https://doi.org/10.1111/j.1533-2500.2012.00557.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the institutional review board of Severance Hospital, Yonsei University Health System (IRB No. 4-2017-0285).
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Yoon, D.M., Yoon, K.B., Baek, I.C. et al. Predictors of analgesic efficacy of neurolytic celiac plexus block in patients with unresectable pancreatic cancer: the importance of timing. Support Care Cancer 26, 2023–2030 (2018). https://doi.org/10.1007/s00520-018-4043-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4043-2