Abstract
Although celiac plexus block (CPB) is a well known technique that has been performed for years, only in the last 30 years controlled studies, demonstrated its efficacy and safety. A historical pathway of literature regarding CPB and a critical analysis may help understand some points which remain still controversial, for a better interpretation of data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Celiac plexus block is an effective and safe technique forpatients with pancreatic cancer pain. However, there are still some controversies about duration, right, survival, and quality of life. |
Stabilizing patients may allow to homogenize the sample undergoing the block. |
Patients on opioid therapy with an acceptable performance status could be candidate. The analgesic effect and duration will depend on the local evolution of cancer which could invade somatic structures not coved by the sympathetic block. |
Survival and quality of life are unlikely to depend on the block Pain is a major cause of distress among patients with cancer. |
Pancreatic cancer is one of the most frequent cancers [1, 2], characterized by a poor prognosis and a painful condition. Celiac plexus block (CPB) is a technique performed for many years that has become with an effective procedure among palliative care or pain physicians. There is high quality evidence of the analgesic efficacy of CPB in patients with pancreatic cancer pain. For this reason a strong recommendation has been suggested to perform the procedure [3]. Complications are rare, especially with modern imaging-guides. This observation has been reported in a sufficient number of patients in randomized controlled studies [4,5,6,7,8,9,10,11,12,13,14,15,16]. Only one paper did not show any difference [13]. Despite CPB is an old technique, only in the last 30 years various controlled studies, using different approaches and modalities, demonstrated the efficacy and safety of CPB. An historical pathway of literature regarding CPB and a critical analysis may help understand some points which remain still controversial, for a better interpretation of data.
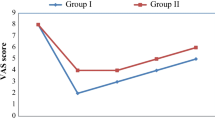
The first controlled studies enrolled low number of patients (10–12 patients for each comparison group). Starting from the beginning, in the first study, patients were first stabilized with analgesics for a week and then were randomized to receive CPB and analgesics or analgesics only [4]. A decrease in opioid consumption and less adverse effects were found in CPB + analgesic group. However, no differences in pain intensity were reported. In a subsequent study with a similar protocol, a significant decrease either in pain intensity and morphine consumption patients was observed in patients who underwent CPB in comparison with patients receiving pharmacological therapy with analgesics. Moreover, deterioration of quality of life was less marked in the CPB group [5]. In a further study patients treated with CPB were compared with patients receiving a standard analgesic therapy [6]. The former group reported a better pain relief with adverse effects compared with the group of patients treated with analgesics. However, long-term results did not differ.
In a double-blind study intraoperative splanchnicetomy or saline injection were compared in patients with pancreatic cancer, even in those not reporting pain [7]. The block provided a significant decrease of pain intensity or delayed the onset of pain in patients who did not experience pre-existing pain. Unexpectedly, a longer survival was found in patients receiving the block. Of interest, patients with pain had a shorter survival. In another analysis, the procedure was found to improve pain and mood, and reduced pain interference with activity [8]. In a controlled study patients were randomly assigned to an early CPB or a pharmacological treatment with analgesics. CPB determined a better pain relief at 1–3 months intervals. No differences in morphine consumption were reported, as well on quality of life or survival [9]. In another study performed in a small number of patients, intraoperative CPB was compared with a pharmacological therapy. Patients were receiving in most cases just anti-inflammatory drugs. No differences in analgesic consumption were found after one week. In the subsequent weeks analgesic consumption decreased in CPB group. Pain intensity, however, was not reported. Even in this case, a longer survival was found in CPB group [10]. In a large randomized-controlled double blind study CPB produced a better pain relief, without affecting quality of life or survival in comparison with a sham procedure with local anaesthetics [11].
In a controlled study CPB was compared with a conventional analgesic treatment. The effect on pain intensity were limited in time, and no differences in pain scores were found after two weeks. Opioid consumption decreased and side effects were lower in CPB group. No differences in quality of life were observed [12]. CPB or thoracoscopic splanchnicectomy were compared with the use of analgesics. While a good pain control was achieved in 50% of patients two months after the procedures, no differences between the groups in pain intensity, opioid consumption, and side effects were found [13].
In a study with a different design, patients were randomly assigned to perform an early CPB or to be first treated with analgesics and then with CPB when pain intensity was controlled. When analgesics were given prior to CPB a significant reduction of pain intensity and a better quality of life was reported after 30–60 days. Moreover, morphine consumption and adverse effects were lower [14]. Finally, a further large randomized controlled study showed that the block provided good analgesia with less opioid consumption in patients with pancreatic cancer pain, with a reduction in the analgesic effect by half in the first two months after treatment [15].
Thus, no doubt exists about the benefit of this procedure. However, palliative care physicians are relatively reluctant in using or proposing such a technique. Some controversies still remain, particularly regarding the most appropriate timing for performing CPB and which patients could have the best benefit. All this mass of data should be interpreted to provide a panorama regarding the issue of a technique that has been demonstrated to be efficacious and and to suggest insights for future research.
Methods
In the first controlled study, at baseline all patients were first treated by opioid therapy until they achieved acceptable pain control. Subsequently, one group underwent a celiac plexus block, integrated by pharmacological therapy according to the clinical needs, while the second group received pharmacological therapy only [4]. This approach may reduce the overall severity at baseline pain with poor individual variations in pain seen in the most recent study [15], in which the standard deviations at baseline were relatively higher [1.3–1.2], meaning that some patients had high pain levels and some other just moderate pain levels. These variations possibly influenced the data reported in subgroup analysis, as stated by the some authors. Indeed, differences of 0.7, although significant, are irrelevant from a clinical point of view. On the other hand the use of an integrated score including pain intensity and analgesic consumption may help understanding a balanced differences between groups [4].
Early Intervention
There are suggestions of some authors for an early performance of CPB, being more efficacious than later, just before the tumor invades other structures beyond the visceral innervation or because of local anatomic distortions [6, 8]. While this observation is meaningful from a technical point of view, it does not take into account some other aspects. Pain evolution is unpredictable and not necessarily patients will develop severe pain along the trajectory of disease to justify a pre-emptive block in patients who receive no opioids or very low opioid doses [16]. On the other hand, if tumor involves other areas of pain innervation, for example somatic structures such as diaphragm or peritoneum, the block will be less effective, as the procedure aims to block the sympathetic pathways for visceral pain only. Thus, even though this procedure is performed earlier when pain is exclusively visceral in nature, pain could then worsen because of the subsequent involvement of neural and somatic structures, independently from an early performance of the block. Of interest, in these papers favorable to an early intervention, the block was often performed in patients receiving just anti-inflammatory drugs or very low doses of opioids, or even in patients with no pain. One study compared different sympathetic blocks to patients who were receiving low or high dose of opioids. However, the level of opioid consumption does not reflect necessarily the stage of disease. Of interest, in the paper where CPB was associated with prolonged survival in patients with and without pain, no patients with pain were long term survivors. This is consistent with the hypothesis that local invasion enough to cause pain is a grave condition in pancreas cancer patients with pain.
The effect of controlling severe pain with medications before performing the CPB, for example, was more effective than an early block, performed at beginning and followed by pharmacotherapy [4, 11]. While the neurolysis is effective and allows the reduction of opioid doses for a variable period of time, the decision on the right time should be based on a clear information about benefits and disadvantages in individuals, expectations, different stages of disease, and individual clinical circumstances.
Survival
Another critical point regards the survival. Some studies reported that CPB shortened or prolonged survival, in contrast with observations of other studies [7,8,9,10,11]. Again, there are no reasons to explain these extreme positions existing in literature, prolonging or shortening survival, probability due to the variability of population. Indeed, it is likely that the block simply does not influence the survival. The fact that patients with no pain undergoing to CPB have a longer survival may simply reflect an early stage of disease in comparison with patients with pain.
Duration of CPB
Some observations can further contribute to a better understanding regarding the use of this procedure. Studies, including the last large trial [13], report that neurolysis generated a quicker pain reduction at the beginning of treatment which then declined, but did not provide any explanation for that. The reason to explain this finding could be that the block loses its efficacy because other pain mechanisms, non mediated by the sympathetic system, develop due to the progression of disease involving somatic structures. Disease progression is individual and unpredictable, when a patient is assessed for a possible CPB. Of interest, the use of an integrated score, for example, has shown that the half-life of the block (that is that when the effect is reduced of 50% after the quickest effect, immediately after the block) is about one month [4].
Quality of Life
Data on quality of life is controversial in literature, and it could not be otherwise, independently from the type of assessment. In patients with advanced cancer who have often a multitude of symptoms, it is unlikely that a procedure, even able to decrease pain intensity or opioid consumption, can improve quality of life, that is affected by a huge number of factors other than pain.
In conclusion there is a good quality of evidence of the analgesic efficacy of CPB. Complications are rare, especially with modern imaging-guides. However, the decision to perform a CPB relies on an individual evaluation of each patient, balancing the possible advantages and disadvantages in each specific clinical situation and timing along the course of disease. Probably the best time to intervene could be after an initial treatment with opioids to assess the individual response. If patients have low levels of pain intensity or no pain or are responsive to low doses of opioids or non-opioid analgesics, there is no reason to perform the procedure. Indeed, when celiac area is distorted by the tumor invasion, the effects of a CPB are expected to be reduced. In other words, not too early, not too late.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by the author.
References
Rawla P, Sunkara T, Gaduputi V. Epidemiology of pancreatic cancer: Global trends, etiology and risk factors. World J Oncol. 2019;10:10–27.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Mercadante S, Klepstad P, Kurita GP, Sjøgren P, Giarratano A. Sympathetic blocks for visceral cancer pain management: A systematic review and EAPC recommendations. European Palliative Care Research Collaborative (EPCRC). Crit Rev Oncol Hematol. 2015;96:577–83.
Mercadante S. Celiac plexus block versus analgesics in pancreatic cancer pain. Pain. 1993;52:187–92.
Kawamata M, Ishitani K, Ishikawa K, Sasaki H, Ota K, Omote K, Namiki A. Comparison between celiac plexus block and morphine treatment on quality of life in patients with pancreatic cancer pain. Pain. 1996;64:597–602.
Polati E, Finco G, Gottin L, Bassi C, Pederzoli P, Ischia S. Prospective randomized double-blind trial of neurolytic celiac plexux block in patients with pancreatic cancer. Br J Cancer. 1998;85:199–201.
Lillemoe K, Cameron JL, Kaufman HS, Yeo C, Pitt H, Sauter PK. Chemical splanchnicectomy in patients with unresectable pancreatic cancer. A prospective randomized trial. Ann Surg. 1993;217:447–57.
Staats PS, Hekmat H, Sauter P, Lillemoe K. The effects of alcohol celiac plexus block, pain, and mood on longevity in patients with unresectable pancreatic cancer: a double-blind, randomized, placebo-controlled study. Pain Med. 2001;2:28–34.
Wyse JM, Carone M, Paquin SC, Usatii M, Sahai AV. Randomized, double-blind, controlled trial of early endoscopic ultrasound-guided celiac plexus neurolysis to prevent pain progression in patients with newly diagnosed, painful, inoperable pancreatic cancer. J Clin Oncol. 2001;26:3541–6.
Okuyama M, Shibata T, Morita T, Kitada M, Tukahara Y, Fukushima Y, Ikeda K, Fuzita J, Shimano T. A comparison of intraoperative celiac plexus block with pharmacological therapy as a treatment for pain of unresectable pancreatic cancer. J Hepatobiliary Pancreat Surg. 2002;9:372–5.
Wong GY, Schroeder DR, Carns PE, Wilson JL, Martin DP, Kinney MO, Mantilla CB, Warner DO. Effect of neurolytic celiac plexus block on pain relief, quality of life, and survival in patients with unresectable pancreatic cancer. A randomized controlled trial. JAMA. 2004;291:1092–9.
Zhang C, Zhang T, Guo Y, Yang L, He M, Shi J, Ni J. Effect of neurolytic celiac plexus block guided by computerized tomography on pancreatic cancer pain. Dig Dis Sci. 2008;53:856–60.
Johnson CD, Berry DP, Harris S, Pickering RM, Davis C, George S, Imrie CW, Neoptolemos JP, Sutton R. An open randomized comparison of clinical effectiveness of protocol-driven opioid analgesia, celiac plexus block or thoracoscopic splanchnicectomy for pain management in patients with pancreatic and other abdominal malignancies. Pancreatology. 2009;9(6):755–63.
Amr Y, Makharita MY. Comparative study between 2 protocols formanagement of severe pain in patients with unresectable pancreatic pain oneyear follow-up. Clin J Pain. 2013;29:807–13.
Dong D, Zhag M. Zhang Z. Huang M, Wang Y, Qi L,Wan CF, Yu X, Song T. Neurolytic splanchnic nerve block and pain relief, survival, and quality of life in unresectable pancreatic cancer: a randomized controlled trial. Anesthesiology 2021;135:686–698.
Mercadante S, Fulfaro F. Casuccio A Pain mechanisms involved and outcome in advanced cancer patients with possible indications for celiac plexus block and superior hypogastric plexus block. Tumori. 2002;88:243–5.
Acknowledgements
Funding
No funding was received for this study or the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
S.M was responsible for the information included in the text.
Disclosures
Sebastiano Mercadante has nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by the author.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Mercadante, S. Commentary: Interpreting Data of Celiac Plexus Block in Patients with Pancreatic Pain: Timing, Patients, Survival. Pain Ther 11, 747–751 (2022). https://doi.org/10.1007/s40122-022-00396-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-022-00396-8