Abstract
Purpose
The aim of this study was to describe the use of palliative sedation (PS) its indications and outcomes in patients followed up till death by an inpatient palliative care consult team (PCCT) at a tertiary cancer center.
Methods
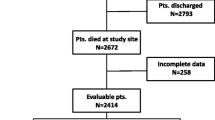
All patients referred for 5 years to the PCCT and followed up till death were eligible for the study. Both PCCT recordings and hospital charts were reviewed and a codified assessment was performed.
Results
Over a total of 2,033 consecutive consults, 129 patients died during admission and were eligible. Eighty-three had the indication to PS, 4% of all consults (95% confidence interval [95%CI], 3% to 5%) and 64% of eligible patients (95%CI, 56% to 73%). PS was more frequently indicated in males and in patients with recurrent dyspnea and recurrent agitation, while it was less frequently indicated in older people and in patients with cerebral metastases and recurrent drowsiness. The most frequent indications to PS were dyspnea (37%) and delirium (31%) alone or combined with other symptoms. PS was successfully achieved in 69 patients; the drugs most frequently used for PS were midazolam (46%), haloperidol (35%), and chlorpromazine (32%) and opioid dose escalation was higher in sedated patients (P < 0.01).
Conclusions
PS is an important intervention in the management of terminal disease by a consulting palliative care team. Improved collaboration and communication between the hospital staff and the PCCT should be offered to meet patients’ needs when PS is required.

Similar content being viewed by others
References
Maltoni M, Amadori D (2001) Palliative medicine and medical oncology. Ann Oncol 12:443–450
Cherny NI, Catane R, European Society of Medical Oncology Taskforce on Palliative and Supportive Care (2003) Attitudes of medical oncologists toward palliative care for patients with advanced and incurable cancer: report on a survey by the European Society of Medical Oncology Taskforce on Palliative and Supportive Care. Cancer 98:2502–2510
Meyers FJ, Linder J (2003) Simultaneous care: disease treatment and palliative care throughout illness. J Clin Oncol 21:1412–1415
Bruera E, Neumann CM (1999) Respective limits of palliative care and oncology in the supportive care of cancer patients. Support Care Cancer 7:321–327
Massarotto A, Carter H, MacLeod R, Donaldson N (2000) Hospital referrals to a hospice: timing of referrals, referrers' expectations, and the nature of referral information. J Palliat Care 16:22–29
Radbruch L, Nauck F, Fuchs M et al (2002) What is palliative care in Germany? Results from a representative survey. J Pain Symptom Manage 23:471–483
Pantilat SZ, Billings JA (2003) Prevalence and structure of palliative care services in California hospitals. Arch Intern Med 163:1084–1088
Hunt RW, Fazekas BS, Luke CG, Priest KR, Roder DM (2002) The coverage of cancer patients by designated palliative services: a population-based study, South Australia, 1999. Palliat Med 16:403–409
Homsi J, Walsh D, Nelson KA et al (2002) The impact of a palliative medicine consultation service in medical oncology. Support Care Cancer 10:337–342
Cherny NI, Portenoy RK (1994) Sedation in the management of refractory symptoms: guidelines for evaluation and treatment. J Palliat Care 10:31–38
Fainsinger RL (1998) Use of sedation by a hospital palliative care support team. J Palliat Care 14:51–54
Hallenbeck JL (2000) Terminal sedation: ethical implications in different situations. J Palliat Med 3:313–320
Morita T, Tsuneto S, Shima Y (2001) Proposed definitions for terminal sedation. Lancet 358:335–336
Porta i Sales J (2002) Palliative sedation: clinical aspects. In Gastman (ed) Between technology and humanity. Leuven University Press, Leuven, pp 30–37
Jackson WC (2002) Palliative sedation vs. terminal sedation: what's in a name? Am J Hosp Palliat Care 19:81–82
Morita T, Bito S, Kurihara Y, Uchitomi Y (2005) Development of a clinical guideline for palliative sedation therapy using the Delphi method. J Palliat Med 8:716–729
Cherny NI, Radbruch L, Board of the European Association for Palliative Care (2009) European Association for Palliative Care (EAPC) recommended framework for the use of sedation in palliative care. Palliat Med 23:581–593
Kirk TW, Mahon MM, Palliative Sedation Task Force of the National Hospice and Palliative Care Organization Ethics Committee (2010) National Hospice and Palliative Care Organization (NHPCO) position statement and commentary on the use of palliative sedation in imminently dying terminally ill patients. J Pain Symptom Manage 39:914–923
Verkerk M, van Wijlick E, Legemaate J, de Graeff A (2007) A national guideline for palliative sedation in the Netherlands. J Pain Symptom Manage 34:666–670
Chater S, Viola R, Paterson J, Jarvis V (1998) Sedation for intractable distress in the dying—a survey of experts. Palliat Med 12:255–269
Maltoni M, Pirovano M, Nanni O et al (1997) Biological indices predictive of survival in 519 Italian terminally ill cancer patients. Italian Multicenter Study Group on Palliative Care. J Pain Symptom Manage 13:1–9
Maltoni M, Nanni O, Pirovano M et al (1999) Successful validation of the palliative prognostic score in terminally ill cancer patients. Italian Multicenter Study Group on Palliative Care. J Pain Symptom Manage 17:240–247
Maltoni M, Caraceni A, Brunelli C et al (2005) Prognostic factors in advanced cancer patients: evidence-based clinical recommendations—a study by the Steering Committee of the European Association for Palliative Care. J Clin Oncol 23:6240–6248
De Conno F, Caraceni A (1996) Manual of cancer pain. Kluwer Academic Press, Dorchrecht
Mercadante S, Fulfaro F, Casuccio A, Barresi L (1999) Investigation of an opioid response categorization in advanced cancer patients. J Pain Symptom Manage 18:347–352
Carter H, Mckinlay E, Scott I, Wise D, MacLeod R (2002) Impact of a hospital palliative care service: perspective of the hospital staff. J Palliat Care 18:160–167
Sykes N, Thorns A (2003) The use of opioids and sedatives at the end of life. Lancet Oncol 4:312–318
Maltoni M, Pittureri C, Scarpi E et al (2009) Palliative sedation therapy does not hasten death: results from a prospective multicenter study. Ann Oncol 20:1163–1169
Fainsinger RL, Waller A, Bercovici M et al (2000) A multicentre international study of sedation for uncontrolled symptoms in terminally ill patients. Palliat Med 14:257–265
Chiu TY, Hu WY, Lue BH, Cheng SY, Chen CY (2001) Sedation for refractory symptoms of terminal cancer patients in Taiwan. J Pain Symptom Manage 21:467–472
Elsayem A, Curry Iii E, Boohene J et al (2009) Use of palliative sedation for intractable symptoms in the palliative care unit of a comprehensive cancer center. Support Care Cancer 17:53–59
Muller-Busch HC, Andres I, Jehser T (2003) Sedation in palliative care—a critical analysis of 7 years experience. BMC Palliat Care 2:2
Peruselli C, Di Giulio P, Toscani F et al (1999) Home palliative care for terminal cancer patients: a survey on the final week of life. Palliat Med 13:233–241
Stone P, Phillips C, Spruyt O, Waight C (1997) A comparison of the use of sedatives in a hospital support team and in a hospice. Palliat Med 11:140–144
Orentlicher D (1997) The Supreme Court and terminal sedation: rejecting assisted suicide, embracing euthanasia. Hastings Constit Law Q 24:947–968
Caraceni A, Nanni O, Maltoni M et al (2000) The impact of delirium on the short-term prognosis of advanced cancer patients. Cancer 89:1145–1148
Bruera E, Macmillan K, Pither J, MacDonald RN (1990) Effects of morphine on the dyspnea of terminal cancer patients. J Pain Symptom Manage 5:341–344
Ventafridda V, Spoldi E, De Conno F (1990) Control of dyspnea in advanced cancer patients. Chest 98:1544–1545
De Conno F, Spoldi E, Caraceni A, Ventafridda V (1991) Does pharmacological treatment affect the sensation of breathlessness in terminal cancer patients. Palliat Med 5:237–243
Caraceni A, Bosisio M, Ingham JM (2002) Confusion and delirium. In: Schiff D, Kasari S, Wen PY (eds) Cancer neurology in clinical practice, 2nd ed. Humana, Totowa, pp 65–90
Jacobi J, Fraser GL, Coursin DB et al (2002) Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 30:119–141
Brown EN, Lydic R, Schiff ND (2010) General anesthesia, sleep, and coma. N Engl J Med 363:2638–2650
Pace-Schott EF, Hobson JA (2002) Basic mechanisms of sleep new evidence on the neuroanatomy and neuromodulation of the NREM–REM cycle. In: Davis KL, Charney D, Coyle JT, Nemeroff C (eds) Neuropsychopharmacology: the fifth generation of progress. American College of Neuropsychopharmacology, Brentwood, pp 1859–1877
Lawlor PG, Bruera E (1998) Side-effects of opioids in chronic pain treatment. Curr Opin Anaesthesiol 11:539–545
Kohara H, Ueoka H, Takeyama H, Murakami T, Morita T (2005) Sedation for terminally ill patients with cancer with uncontrollable physical distress. J Palliat Med 8:20–25
Sykes N, Thorns A (2003) Sedative use in the last week of life and the implications for end-of-life decision making. Arch Intern Med 163:341–344
Acknowledgments
This work was partially funded by the Floriani Foundation of Milan and Associazione Italiana per la Ricerca sul Cancro, grant no. IG9347.
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Caraceni, A., Zecca, E., Martini, C. et al. Palliative sedation at the end of life at a tertiary cancer center. Support Care Cancer 20, 1299–1307 (2012). https://doi.org/10.1007/s00520-011-1217-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-011-1217-6