Abstract
Background
There is wide variation in the frequency of reported use of palliative sedation (PS) to control intractable and refractory symptoms in terminally ill patients. The aim of this study was to determine the frequency and outcomes of PS use and examine patterns of practice after establishment of a policy for the administration of midazolam for PS in our palliative care unit (PCU).
Materials and methods
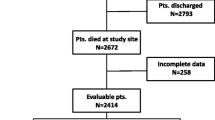
This retrospective study reviewed PCU admissions for 2004 and 2005 and pharmacy records to identify patients who received chlorpromazine, lorazepam, or midazolam for PS in the PCU. Data on indication for PS, drug used, and discharge outcome were assessed for each patient.
Results
During the period studied, there were 1,207 PCU admissions. Of these patients, 186 (15%) received PS; and 143 (41%) of the 352 patients who died in the PCU received PS. The median age of PS patients was 58 (range, 20–84) years, and 106 (57%) were male. The most common indications for PS were delirium, 153 cases (82%); dyspnea, 11 (6%); and multiple indications, 12 (6%). Midazolam was used in 18 PS cases (10%). Six (55%) of 11 patients with dyspnea received midazolam for PS, compared with 12 (7%) of 175 patients with other indications for PS (p < 0.001). Forty-three (23%) of 186 PS patients were discharged alive, compared with 812 (80%) of 1,021 patients who did not receive PS (p < 0.001).
Conclusions
PS was required in 15% of PCU admissions, and 23% of PS patients were discharged alive. Our findings suggest a potential for significant underreporting of overall PS. If our institution’s policy on midazolam use for PS were less restrictive, midazolam use might increase. More research is needed to define the optimal agent for inducing rapid, effective, and easily reversible PS.


Similar content being viewed by others
References
American Academy of Hospice and Palliative Medicine. Statement on Palliative Sedation, Sept. 2006. www.aahpm.org/position
Breitbart W, Gibson C, Tremblay A (2002) The delirium experience: delirium recall and delirium-related distress in hospitalized patients with cancer, their spouses/caregivers, and their nurses. Psychosomatics 43:183–194
Breitbart W, Marotta R, Platt MM et al (1996) Double-blind trial of haloperidol, chlorpromazine, and lorazepam in the treatment of delirium in hospitalized AIDS patients. Am J Psychiatry 153:231–237
Bruera E, Kuehn N, Miller MJ et al (1991) The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care 7:6–9
Bruera E, Neumann CM (1998) The uses of psychotropics in symptom management in advanced cancer. Psychooncology 7:346–358
Cameron D, Bridge D, Blitz-Lindeque J, Bruera E (2004) Use of sedation to relieve refractory symptoms in dying patients. S Afr Med J 94:445–449
Chater S, Viola R, Paterson J, Jarvis V (1998) Sedation for intractable distress in the dying—a survey of experts. Palliat Med 12:255–269
Cheng C, Roemer-Becuwe C, Pereira J (2002) When midazolam fails. J Pain Symptom Manage 23:256–265
Cherny NI, Portenoy RK (1994) Sedation in the management of refractory symptoms: guidelines for evaluation and treatment. J Palliat Care 1010:31–38
Cowan J, Walsh D (2001) Terminal sedation in palliative medicine: definition and review of the literature. Support Care Cancer 9:403–407
de Graeff A, Strasser F. Indications and conditions for palliative sedation. EAPC Forum from the 9th Congress of EAPC, April 2005. www.eapcnet.org/forum
Del Fabbro E, Dalal S, Bruera E (2006) Symptom control in palliative care-Part III: dyspnea and delirium. J Palliat Med 9:422–436
Del Fabbro E, Reddy SG, Walker P, Bruera E (2007) Palliative sedation: when the family and consulting service see no alternative. J Palliat Med 10(2):488–492, Apr
Drummond SH, Peterson GM, Galloway JG, Keefe PA (1996) National survey of drug use in palliative care. Palliat Med 10:119–124
Elsayem A, Swint K, Fisch MJ et al (2004) Palliative care inpatient service in a comprehensive cancer center: clinical and financial outcomes. J Clin Oncol 22:2008–2014
Engstrom J, Bruno E, Holm B, Hellzen O (2006) Palliative sedation at end of life—a systematic literature review. Eur J Oncol Nurs 11(1):26–35
Fainsinger RL, Waller A, Bercovici M et al (2000) A multi-center international study of sedation for uncontrolled symptoms in terminally ill patients. Palliat Med 14:257–265
Foy A, O’Connell D, Henry D, Kelly J, Cocking S, Halliday J (1995) Benzodiazepine use as a cause of cognitive impairment in elderly hospital inpatients. J Gerontol A Biol Sci Med Sci 50(2):99–106
Gaudreau JD, Gagnon P, Harel F, Roy MA, Tremblay A (2005) Psychoactive medications and risk of delirium in hospitalized cancer patients. J Clin Oncol 23(27):6712–6718
Gaudreau JD, Gagnon P, Roy MA, Harel F, Tremblay A (2007) Opioid medications and longitudinal risk of delirium in hospitalized cancer patients. Cancer 109(11):2365–2373
Graeff AD, Dean M (2007) Palliative sedation therapy in the last weeks of life: a literature review and recommendations for standards. Palliat Med 10:67–85
Lawlor PG, Bruera ED (2002) Delirium in patients with advanced cancer. Hematol Oncol Clin North Am 16:701–714
Lawlor PG, Gagnon B, Mancini IL et al (2000) Occurrence, causes, and outcome of delirium in patients with advanced cancer: a prospective study. Arch Intern Med 160(6):786–794
Levy MH, Cohen SD (2005) Sedation for the relief of refractory symptoms in the imminently dying: a fine intentional line. Semin Oncol 32(2):237–246
Lo B, Rubenfeld G (2005) Palliative sedation in dying patients: “we turn to it when everything else hasn’t worked”. JAMA 294:1810–1816
Lundstrom S, Zachrisson U, Furst CJ (2005) When nothing helps: propofol as sedative and antiemetic in palliative cancer care. J Pain Symptom Manage 30:570–577
Mclver B, Walsh D, Nelson K (1994) The use of chlorpromazine for symptom control in dying cancer patients. J Pain Symptom Manage 9:341–345
Morita T, Bito S, Kurihara Y, Uchitomi Y (2005) Development of clinical guideline for palliative sedation therapy using the Delphi method. J Palliat Med 8:716–729
Pecking M, Montestruc F, Marquet P, Wodey E, Homery M, Dostert P (2002) Absolute bioavailability of midazolam after subcutaneous administration to healthy volunteers. Br J Clin Pharmacol 54:357–362
Pereira J, Hanson J, Bruera E (1997) The frequency and clinical course of cognitive impairment in patients with terminal cancer. Cancer 79:835–842
Reves JG, Fragen J, Vinik H, Greenblatt J (1985) Midazolam: pharmacology and uses. Anesthesiology 62:310–324
Rousseau PC (2006) Palliative sedation and the fear of legal ramifications. J Palliat Med 9:246–247
Sales J (2001) Sedation and terminal care. Eur J Palliat Care 8:97–100
Stevanovic P (2006) Midazolam (dormicump)—clinical practice guidelines. Med Pregl 59:89–94
Stone P, Phillips C, Spruyt O, Waight C (1997) A comparison of the use of sedatives in a hospital support team and in a hospice. Palliat Med 11:140–144
Sykes N, Thorns A (2003) Sedative use in the last week of life and the implications for end-of-life decision-making. Arch Intern Med 163:341–344
Thomas JR, von Gunten CF (2003) Management of dyspnea. J Support Oncol 1:23–32
Acknowledgment
The authors would like to thank Melissa Burkett of the Department of Scientific Publications for her help in preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
These data were presented in part at the Annual meeting of the American Society of Clinical Oncology; Atlanta, GA, 2006.
Rights and permissions
About this article
Cite this article
Elsayem, A., Curry III, E., Boohene, J. et al. Use of palliative sedation for intractable symptoms in the palliative care unit of a comprehensive cancer center. Support Care Cancer 17, 53–59 (2009). https://doi.org/10.1007/s00520-008-0459-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-008-0459-4