Abstract
Introduction
Our aim was to determine long-term survival and quality of life of patients admitted to a surgical intensive care unit (ICU) because of sepsis or trauma.
Methods
This was an observational study conducted in an 11-bed, closed surgical ICU at a 860-bed teaching general hospital over a 1-year period (January 2003 to December 2003). Patients were divided into two groups according to admission diagnoses: group 1 included patients with sepsis; and group 2 included patients with trauma (polytrauma, multiple trauma, head injury, or spinal injury). Quality of life was assessed after 2 years following ICU admission using the EuroQol 5D questionnaire.
Results
A total of 164 patients (98 trauma patients and 66 patients with sepsis) were included in the study. Trauma patients were younger than patients with sepsis (53 ± 21 years versus 64 ± 13 years; P ≤ 0.001). There was no significant difference between groups in Acute Physiology and Chronic Health Evaluation II score or length of stay in the surgical SICU. Trauma patients stayed longer on the general ward (35 ± 44 days versus 17 ± 24 days; P < 001). Surgical ICU survival, in-hospital survival, and post-hospital and cumulative 2-year survival were lower in the sepsis group than in the trauma group (surgical ICU survival: 60% versus 74%; in-hospital survival: 42% versus 62%; post-hospital survival: 78% versus 92%; cumulative 2-year survival: 33% versus 57%; P < 0.05). There was no significant difference in quality of life in all five dimensions of the EuroQol 5D between groups: 60% of patients had signs of depression, almost 60% had problems in usual activities and 56% had pain.
Conclusion
Patients with sepsis treated in a surgical ICU have higher short-term and long-term mortality than do trauma patients. However, quality of life is reduced to the same level in both groups.
Similar content being viewed by others
Introduction
Intensive care units (ICUs) serve patients with acute physiological derangement and organ failure but who have potentially reversible disease. They also provide a service for those who can benefit from more comprehensive observation and complex treatment than is available on standard hospital wards [1–3].
Critical illness is associated with a wide array of serious and troublesome long-term sequelae that may interfere with achieving optimal patient-centred outcomes. Although traditional short-term outcomes, such as hospital mortality, remain extremely important, they are unlikely to be adequate surrogates for subsequent patient-centred outcomes. As such, it is important to focus specifically on how critical illness and intensive care can affect long-term health and well being [4].
Critical care patients differ with respect to the reason for their admission to the ICU, and these differences are likely to result in different expectations regarding their health. Therefore, when measuring outcomes in intensive care patients, we should take into account the possibility that outcomes will vary by admission diagnostic category [5]. The aim of the present study was to compare the long-term survival and quality of life of patients treated in a surgical ICU because of sepsis or trauma.
Materials and methods
In an observational study we included patients admitted to the surgical ICU over a 1-year period (January 2003 to December 2003). The surgical ICU at our 860-bed teaching general hospital is an adult, 11-bed, closed unit. Permission to perform the study was granted by the national ethics committee.
Patients were divided into two groups according to admission diagnoses: group 1 included patients with sepsis (severe sepsis and septic shock) and group 2 included those with trauma (polytrauma, multiple trauma, head injury, or spinal injury). Sepsis was defined as clinical signs suggesting the presence of systemic inflammatory response syndrome together with definite evidence of infection. Systemic inflammatory response syndrome was defined as any two of the following [6–8]: temperature >38°C or <36°C; heart rate >90 beats/min; respiratory rate >20 breaths/min or arterial carbon dioxide tension <32 mmHg; and white blood cell count >12,000 cells/mm3 or <4000 cells/mm3, or with >10% immature (band) forms. Sepsis was considered severe when it was associated with organ dysfunction, hypoperfusion, or hypotension [7]. Septic shock was defined as sepsis with hypotension despite adequate fluid resuscitation, combined with perfusion abnormalities that may include lactic acidosis, oliguria, or an acute alteration in mental status [7]. Polytrauma was defined as injury to several physical regions or organ systems, where at least one injury or a combination of several injuries was life threatening, with the severity of injury being 16 or greater on the Injury Severity Score [9]. Multiple trauma was defined as physical insults or injuries occurring simultaneously in several parts of the body, and it was differentiated from polytrauma because multiple trauma was not life threatening [9, 10].
Patient demographic characteristics, length of stay (LOS) in the surgical ICU, severity of illness (risk for hospital mortality, as indicated by Acute Physiology and Chronic Health Evaluation [APACHE] II score) and LOS in the general ward were all recorded, as were surgical ICU and hospital outcome. When patients were readmitted to the surgical ICU, data from their last admission were used. The hospital patient's registry was used to obtain information on patients who had died in the hospital. Survival data for patients 2 years after ICU treatment were collected from the Central Register of Inhabitants for the Republic of Slovenia.
Quality of life was assesed after 2 years following ICU admission for surviving patients using EuroQol 5D questionnaire and a telephone interview. EuroQoL 5D [11–13] is a generic health status measure that consists of three parts: a descriptive system, a visual-analogue scale, and an EuroQol 5D Index. The descriptive system measures health in five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Patients mark one of three levels of severity (1 = no problems, 2 = some/moderate problems and 3 = severe/extreme problems) in each dimension. Combinations of these categories define a total of 243 different health states. The EuroQol 5D Index [14], based on the five dimensions and ranging from -0.11 ('worse than death') to 1 ('perfect health'), was also calculated. In the present study we used only the descriptive system and the EuroQol 5D Index.
Patients or family members of patients who were discharged alive were contacted by phone to determine their willingness to participate in the study and were asked to complete the questionnaire. In the case of severe disability of patients, we used proxy assessment of health-related quality of life (HR-QOL) [4, 15].
Statistical analysis
The characteristics of the study population were assessed using the two-way Student's t-test for continuous and nonparametric Mann-Whitney U-test for noncontinuous variables. Results are presented as mean ± standard deviation (range).
The survival of patients is displayed graphically using Kaplan-Meier curves, and any differences between curves were explored using log-rank or Tarone-Ware tests. For correction of age between two groups of patients (patients with sepsis and patients with trauma), Cox survival analysis was used.
For assessing differences in baseline characteristics between responders and nonresponders to the EuroQol 5D questionnaire, we used independent samples t-test. Analysis of variance was used to test for mean difference in EuroQol 5D profile between patients with sepsis and patients with trauma. P < 0.05 was considered statistically significant.
A statistical computer program (SPSS, version 13; SPSS Inc., Chicago, IL, USA) was employed to conduct data analysis.
Results
Between January 2003 and December 2003, a total of 164 patients were included in the study. Sixty-six of the patients were admitted because of sepsis (severe sepsis and septic shock), and 98 of the patients were admitted after trauma (polytrauma, multiple trauma, head injury, or spinal injury). Gastrointestinal surgery (complications of gastrointestinal surgery, emergency gastrointestinal surgery and pancreatitis) accounted for 76% of all patients in the sepsis group.
The demographic characteristics of the patients, stratified by admission diagnosis, are shown in Table 1. The two groups of patients differed in some respects. Trauma patients were younger than patients with sepsis (53 ± 21 years versus 64 ± 13 years; P < 0.001). There were significantly more men in the trauma than in the sepsis group (71% versus 49%; P = 0.006). There was no significant difference between groups in APACHE II score or surgical ICU LOS. Trauma patients stayed longer on the general ward (35 ± 44 days versus 17 ± 24 days; P < 0.001).
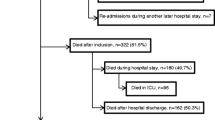
Mortality analysis was separated into short-term mortality (surgical ICU and in-hospital mortality) and long-term mortality (post-hospital mortality). Surgical ICU mortality in the sepsis group was higher than that in the trauma group (40% versus 26%; P = 0.036; Figure 1). In-hospital mortality of patients with sepsis was also higher than that of patients with trauma (58% versus 38%; P = 0.002; Figure 2). Patients with sepsis were older than trauma patients (Table 1). To evaluate the independent effects of age and admission diagnosis (sepsis or trauma) on mortality, we conducted a Cox survival analysis. After controlling for age, we found that admission diagnosis had a significant effect on in-hospital survival (hazard ratio 1.73; P = 0.02; Figure 3).
The long-term outcomes of patients with sepsis and trauma were also significantly different. Not only did the patients with sepsis suffer a higher surgical ICU and in-hospital mortality, but these patients also had poorer long-term outcomes. Figure 4 illustrates the survival of patients after hospital discharge. Post-hospital mortality of patients with sepsis was higher than that of patients with trauma (22% versus 8%; P = 0.049; Figure 4). Finally, cumulative 2-year mortality was higher in the sepsis group than in the trauma group (67% versus 43%; P = 0.002; Figure 5).
Of the 89 patients who were discharged from hospital, 11 (12%) died during the 2-year follow-up period. Quality of life was assessed in 39 patients (50%) of the 78 surviving patients 2 years after ICU admission. In all, 48% (10/21) patients with sepsis and 51% (29/57) patients with trauma participated in the HR-QOL assessment. In addition, baseline characteristics of responders and nonresponders to EuroQol 5D are summarized in Table 2. There was no significant difference in age, sex, LOS in the surgical ICU and hospital between the two groups (Table 2). Only APACHE II score was higher in nonresponders (13.7 ± 5.9 versus 11.0 ± 4.3; P < 0.02; Table 2).
Mean (± standard deviation) EuroQol 5D Index was 0.72 ± 0.24 and did not differ between patients with sepsis and those with trauma. One trauma patient described her functional status as being worse than death (EuroQol 5D Index = -0.11). Eighty-two per cent of patients reported having a problem (moderate or extreme) in at least one dimension of EuroQol 5D. There was no significant difference in quality of life in all five dimensions of EuroQol 5D between groups (Figure 6). Almost 60% of patients reported having problems in usual activities, 56% had pain and 56% had mobility problems; in contrast, most of patients (74%) reported having no problems in self-care. Depression and anxiety were more often detected in trauma patients, but the difference relative to the sepsis group was not significant (P = 0.1).
Discussion
Two main findings of the present study may be identified. First, patients with sepsis treated in the surgical ICU have higher short-term (surgical ICU and in-hospital) and long-term (post-hospital) mortality than do trauma patients. Not surprisingly, cumulative 2-year mortality was higher in the sepsis group than in the trauma group. Severe sepsis is a life-threatening complication of infection. Becaue of the associated organ failure, treatment in the ICU is usually necessary. Several studies have shown that sepsis is the leading cause of mortality for patients admitted to ICUs [16–19]. The observation that sepsis reduces long-term survival when compared with trauma is also consistent with observations from other studies.
Davidson and colleagues [20] compared two specific groups of patients with adult respiratory distress syndrome (ARDS) and demonstrated that sepsis-ARDS patients had a sixfold higher late (post-hospital) mortality rate than did trauma-ARDS patients.
There were some differences in baseline characteristics between the two groups of patients in our study. Patients with sepsis were older than the trauma patients. Sepsis is highly correlated with age and comorbidities, and it may be difficult to separate their independent effects on mortality [21]. Davidson and coworkers [20] also argued that critical care outcome could only be measured in patients who were selected for admission to the ICU, and therefore only reflected the outcome of a subset of elderly patients. As shown in Figure 3, even after controlling for age, sepsis as the admission diagnosis had a significant effect on in-hospital mortality in our study.
The second main finding of our study is that, although patients with sepsis had higher long-term mortality and were older then the trauma patients, there was no significant difference in quality of life after 2 years following intensive treatment. Patients with trauma even had a tendency toward greater anxiety and depression compared with patients who had sepsis. Therefore, quality of life was reduced to the same level in both groups, and 82% of patients reported a problem (moderate or extreme) in at least one dimension of EuroQol 5D, but most patients (74%) reported no problems in self-care.
Critical care patients differ with respect to the cause of their admission to the ICU. We may presume that most patients with trauma were previously healthy individuals who suffered a severe injury and were admitted to the surgical ICU as a result of acute, life-threatening insults. Badia and coworkers [15] reported that trauma patients experienced considerable worsening in their quality of life, because the price of their survival was a deterioration in their HR-QOL as a result of the injuries sustained. On the other hand, patients with sepsis are usually more chronically ill and consequently have diminished HR-QOL, and are admitted to the surgical ICU because of exacerbation of pre-existing chronic pathologies or for surgical interventions aimed at improving their HR-QOL. We must emphasize that our study was conducted in a surgical ICU, and the patients with sepsis (76%) were mostly admitted after major abdominal surgery and had abdominal sepsis. Haraldsen and Andersson [22] retrospectively evaluated long-term outcomes in patients treated in a surgical ICU for abdominal sepsis. They reported that most patients who had survived after treatment of abdominal sepsis in the surgical ICU regained good health and restored functional status.
Granja and coworkers [23] also compared the HR-QOL of survivors from severe sepsis and septic shock with HR-QOL in others who had survived critical illness not involving sepsis using EuroQol 5D. They reported that survivors from severe sepsis and septic shock had similar HR-QOL to that of survivors from critical illness admitted without sepsis. In contrast to those studies, Davidson and colleagues [24] compared HR-QOL in ARDS survivors who had sepsis as their primary risk factor for ARDS with HR-QOL in ARDS survivors with trauma as their primary risk factor for ARDS. They concluded that sepsis-ARDS patients had worse HR-QOL than did trauma-ARDS patients.
The present study has limitations. No patients were lost to follow up for the assessment of survival, but 50% were lost to follow up for the assessment of quality of life at 2 years. Why did we lose so many patients? In our assessment of quality of life we used telephone interview, and for the most part those patients who were lost to follow up had no telephone or had changed their telephone number so we could not contact them. In addition, patients or relatives who refused to cooperate in the study were also lost to follow up. We believe that although we lost so many patients, our population of patients who underwent HR-QOL assessment was representative; in our comparison of responders with nonresponders to the EuroQol 5D questionnaire, we identified no differences in baseline demographics (age or sex) or in surgical ICU or hospital LOS between the two groups of patients.
A further potential limitation of this study was its inability to assess baseline HR-QOL of patients before surgical ICU admission. We assessed quality of life in surviving patients 2 years after ICU admission; this is quite a long period, and recollection of baseline HR-QOL before surgical ICU admission after such an interval may not be accurate. Grady [25] suggested that researchers should be cautious, emphasizing that recall of status at an earlier time point could be influenced by the current situation.
EuroQol 5D was the instrument of choice because it is a simple and short questionnaire that is easily understood and answered by the patients. It is a generic HR-QOL instrument that, apart from permitting estimation of an overall quality of life index, specifically measures a range of physical and nonphysical dimensions [5, 11–13]. Its usefulness and construct validity have been tested in patients in several studies [15, 26–32]. In addition, it is an appropriate method for measuring HR-QOL in critically ill patients [4]. Telephone assessment of EuroQol 5D has the advantage of avoiding the need to recall patients to the hospital; telephone assessment of EuroQol 5D was also validated in several studies [4, 30, 31]. Badia and coworkers [15] also reported that proxy responses could be reliably used with the EuroQol 5D when measuring change in HR-QOL.
Conclusion
In summary, two main conclusions may be drawn from the study. Patients with sepsis treated in the surgical ICU have higher in-hospital and post-hospital mortality than do trauma patients, but quality of life is reduced to the same level in both groups. This means that survival and quality of life after critical illness are independent; when evaluating outcome after intensive care, it is necessary to incorporate assessments of both quality of life and survival.
Key messages
-
We studied long-term outcomes in patients with the two most frequent admission diagnoses admitted to the surgical ICU: sepsis and trauma.
-
Patients with sepsis had higher in-hospital and post-hospital mortality than did trauma patients.
-
Quality of life, as measured using the EuroQol 5D questionnaire, was reduced to the same level in both groups, and 82% of patients reported a problem in at least one dimension of the EuroQol 5D.
Abbreviations
- APACHE:
-
APACHE = Acute Physiologic and Chronic Health Evaluation
- ARDS:
-
ARDS = adult respiratory distress syndrome
- HR-QOL:
-
HR-QOL = health-related quality of life
- ICU:
-
ICU = intensive care unit
- LOS:
-
LOS = length of stay.
References
Chang SY, Multz AS, Hall JB: Critical care organization. Crit Care Clin 2005, 21: 43-53.
Ferdinande P: Recommendations on minimal requirements for intensive care departments. Intensive Care Med 1997, 23: 226-232. 10.1007/s001340050321
Fisher M: Critical care-the worldwide perspective. Ann Acad Med Singapore 1998, 27: 376-380.
Angus DC, Carlet J, on behalf of the 2002 Brussels Roundtable Participants: Surviving Intensive Care: a report from the 2002 Brussels Roundtable. Intensive Care Med 2003, 29: 368-377.
Needham DM, Dowdy DW, Mendez-Tellez PA, Herridge MS, Pronovost PJ: Studying outcomes of intensive care unit survivors: measuring exposures and outcomes. Intensive Care Med 2005, 31: 1153-1160. 10.1007/s00134-005-2656-7
American College of Chest Physicians/Society of Critical Care Medicine: Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 1992, 20: 864-874.
Balk RA: Severe sepsis and septic shock. Definitions, epidemiology, and clinical manifestations. Crit Care Clin 2000, 16: 179-192. 10.1016/S0749-0704(05)70106-8
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G, SCCM/ESICM/ACCP/ATS/SIS: 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 2003, 31: 1250-1256. 10.1097/01.CCM.0000050454.01978.3B
Recommended Guidelines for Diagnostics and Therapy in Trauma Surgery[http://www.uni-duesseldorf.de/AWMF/ll/012-019e.htm]
Multiple trauma (Biology-Online.org)[http://www.biology-online.org/dictionary/Multiple_Trauma]
The EuroQol Group: EuroQol: a new facility for the measurement of health-related quality of life. Health Policy 1990, 16: 199-208. 10.1016/0168-8510(90)90421-9
Rabin R, de Charro F: EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001, 33: 337-343.
EQ-5D: an instrument to describe and value health[http://www.euroqol.org]
Calculating the U.S. population-based EQ-5D Index score[http://www.ahrq.gov/rice/EQ5Dscore.htm]
Badia X, Diaz-Prieto A, Gorriz MT, Herdman M, Torrado H, Farrero E, Cavanilles JM: Using the EuroQol-5D to measure changes in quality of life 12 months after discharge from an intensive care unit. Intensive Care Med 2001, 27: 1901-1907. 10.1007/s00134-001-1137-x
Marshall JC, Vincent JL, Guyatt G, Angus DC, Abraham E, Bernard G, Bombardier C, Calandra T, Jorgensen HS, Sylvester R, et al.: Outcome measures for clinical research in sepsis: a report of the 2nd Cambridge Colloquium of the International Sepsis Forum. Crit Care Med 2005, 33: 1708-1716. 10.1097/01.CCM.0000174478.70338.03
Wright JC, Plenderleith L, Ridley SA: Long-term survival following intensive care: Subgroup analysis and comparison with the general population. Anaesthesia 2003, 58: 637-642. 10.1046/j.1365-2044.2003.03205.x
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, Payen D, Sepsis Occurrence in Acutely Ill Patients investigatiors: Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 2006, 34: 344-353. 10.1097/01.CCM.0000194725.48928.3A
Vincent JL, Abraham E: The last 100 years of sepsis. Am J Respir Crit Care Med 2006, 173: 256-263. 10.1164/rccm.200510-1604OE
Davidson TA, Rubenfeld GD, Caldwell ES, Hudson LD, Steinberg KP: The effect of acute respiratory distress syndrome on long-term survival. Am J Respir Crit Care Med 1999, 160: 1838-1842.
Martin GS, Mannino DM, Eaton S, Moss M: The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 2003, 348: 1546-1554. 10.1056/NEJMoa022139
Haraldsen P, Andersson R: Quality of life, morbidity, and mortality after surgical intensive care: a follow-up study of patients treated for abdominal sepsis in the surgical intensive care unit. Eur J Surg Supp 2003, (588):23-27.
Granja C, Dias C, Costa-Pereira A, Sarmento A: Quality of life of survivors from severe sepsis and septic shock may be similar to that of others who survive critical illness. Critical Care 2004, 8: R91-R98. 10.1186/cc2818
Davidson TA, Caldwell ES, Curtis JR, Hudson LD, Steinberg KP: Reduced quality of life in survivors of acute respiratory distress syndrome compared with critically ill control patients. JAMA 1999, 281: 354-360. 10.1001/jama.281.4.354
Grady KL: Beyond morbidity and mortality: quality of life outcomes in critical care patients. Crit Care Med 2001, 29: 1844-1846. 10.1097/00003246-200109000-00036
Badia X, Schiaffino A, Alonso J, Herdman M: Using the EuroQol 5-D in the Catalan general population: feasibility and construct validity. Qual Life Res 1998, 7: 311-322.
Kind P, Dolan P, Gudex C, Williams A: Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ 1998, 316: 736-741.
Sznajder M, Aegerter P, Launois R, Merliere Y, Guidet B, CubRea : A cost-effectiveness analysis of stays in intensive care units. Intensive Care Med 2001, 27: 146-153. 10.1007/s001340000760
Herridge MS: Long-term outcomes after clinical illness. Curr Opin Crit Care 2002, 8: 331-336. 10.1097/00075198-200208000-00010
Cuthbertson BH, Scott J, Strachan M, Kilonzo M, Vale L: Quality of life before and after intensive care. Anaesthesia 2005, 60: 332-339. 10.1111/j.1365-2044.2004.04109.x
Granja C, Teixeira-Pinto A, Costa-Pereira A: Quality of life after intensive care- evaluation with EQ-5D questionnaire. Intensive Care Med 2002, 28: 898-907. 10.1007/s00134-002-1345-z
Bouillon B, Kreder HJ, Eypasch E, Holbrook TL, Mayou R, Nast-Kolb D, Pirente N, Schelling G, Tiling T, Yates D: Quality of life in patients with multiple injuries-basic issues, assessment, and recommendations. Restor Neurol Neurosci 2002, 20: 125-134.
Acknowledgements
We should like to acknowledge the staff and patients of the surgical ICU in the General Hospital Celje for their help and support with this study. There were no special sources of funding for the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
HKJ was involved in the design of the study; in the acquisition, analysis and interpretation of data; and drafted the manuscript. KJ helped to draft the manuscript. MP participated in the design of the study, helped to perform statistical analysis and revised the manuscript critically. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Korošec Jagodič, H., Jagodič, K. & Podbregar, M. Long-term outcome and quality of life of patients treated in surgical intensive care: a comparison between sepsis and trauma. Crit Care 10, R134 (2006). https://doi.org/10.1186/cc5047
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc5047