Summary
Background
Despite evidence for a bidirectional relationship between obesity and stress-related mental disorders, the general relationship between psychological stress and metabolism is still controversial. Only few studies have addressed this relationship in morbidly obese individuals.
Methods
The present study investigated the relationship between psychological distress, health-related quality of life (HRQL), eating behavior, negative emotions and body mass index (BMI), body composition and biomedical parameters of metabolism in an adult sample of 123 (94 females) morbidly obese individuals.
Results
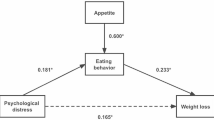
No significant relationship was found between psychological distress and BMI, body composition or any of the parameters of metabolism; however, there was a strong and robust association between HRQL in the physical domain and BMI, body composition and several biomedical parameters of sugar and fat metabolism. The results also showed an interesting dissociation in the relationship between BMI and HRQL in the physical and psychology domains. Only little evidence was found for a relationship between eating behavior (e.g. restraint) or negative emotions (e.g. anger) and BMI, body composition and parameters of metabolism. There was, however, a significant gender difference in restraint eating. Other commonly reported gender differences in BMI, body composition, fat metabolism and liver values were also observed in this sample of morbidly obese individuals.
Conclusion
Results from the present study highlight the relationship between HRQL in the physical domain and metabolism. Implications of these findings for weight loss treatment are discussed, emphasizing HRQL as an important treatment goal and the need for long-term psychological monitoring.

Similar content being viewed by others
Notes
Results from independent samples T-test
t=T-test value(df=degrees of freedom)
References
Gallus S, et al. Overweight and obesity in 16 European countries. European J Nutrition. 2015;54(5):679–89.
Rust P, Hasenegger V, König J. Österreichischer Ernährungsbericht 2017. Wien: Universität Wien und Bundesministerium für Gesundheit und Frauen; 2017.
Ng M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81.
Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. Int J Obes. 2013;37(6):889–91.
Finkelstein EA, et al. Obesity and Severe Obesity Forecasts Through 2030. Am J Prev Med. 2012;42(6):563–70.
Guh DP, et al. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. Bmc Public Health. 2009;9(1):88.
Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017;5(7):161–161.
LeBlanc ES, et al. Behavioral and pharmacotherapy weight loss interventions to prevent obesity-related morbidity and mortality in adults: Updated evidence report and systematic review for the us preventive services task force. JAMA. 2018;320(11):1172–91.
Albuquerque D, et al. Current review of genetics of human obesity: from molecular mechanisms to an evolutionary perspective. Mol Genet Genomics. 2015;290(4):1191–221.
Heymsfield SB, Wadden TA. Mechanisms, Pathophysiology, and Management of Obesity. N Engl J Med. 2017;376(3):254–66.
Paeratakul S, et al. The relation of gender, race and socioeconomic status to obesity and obesity comorbidities in a sample of US adults. Int J Obes. 2002;26:1205.
Drewnowski A, et al. Food environment and socioeconomic status influence obesity rates in Seattle and in Paris. Int J Obes. 2014;38(2):306–14.
Schwartz MW, et al. Obesity pathogenesis: an endocrine society scientific statement. Endocr Rev. 2017;38(4):267–96.
Bouter KE, et al. Role of the gut Microbiome in the pathogenesis of obesity and obesity-related metabolic dysfunction. Gastroenterology. 2017;152(7):1671–8.
Scott KM, et al. Obesity and mental disorders in the general population: results from the world mental health surveys. Int J Obes. 2008;32(1):192–200.
de Wit L, et al. Depression and obesity: a meta-analysis of community-based studies. Psychiatry Res. 2010;178(2):230–5.
Gariepy G, Nitka D, Schmitz N. The association between obesity and anxiety disorders in the population: a systematic review and meta-analysis. Int J Obes. 2009;34:407.
Cortese S, et al. Association between ADHD and obesity: a systematic review and meta-analysis. Am J Psychiatry. 2015;173(1):34–43.
Darby A, et al. The rising prevalence of comorbid obesity and eating disorder behaviors from 1995 to 2005. Int J Eat Disord. 2009;42(2):104–8.
Gerlach G, Loeber S, Herpertz S. Personality disorders and obesity: a systematic review. Obes Rev. 2016;17(8):691–723.
Yamamoto K, Okazaki A, Ohmori S. The relationship between psychosocial stress, age, BMI, CRP, lifestyle, and the metabolic syndrome in apparently healthy subjects. J Physiol Anthropol. 2011;30(1):15–22.
Chen Y, Qian L. Association between lifetime stress and obesity in Canadians. Prev Med. 2012;55(5):464–7.
Istvan J, Zavela K, Weidner G. Body weight and psychological distress in NHANES I. Int J Obes Relat Metab Disord. 1992;16(12):999–1003.
Dallman MF. Stress-induced obesity and the emotional nervous system. Trends Endocrinol Metab. 2010;21(3):159–65.
Hamer M, Stamatakis E. U‑shaped association between body mass index and psychological distress in a population sample of 114,218 British adults. Mayo Clin Proc. 2017;92(12):1865–6.
Petroni ML, et al. Psychological distress in morbid obesity in relation to weight history. Obes Surg. 2007;17(3):391–9.
Mannucci E, et al. Clinical and psychological correlates of health-related quality of life in obese patients. Health Qual Life Outcomes. 2010;8(1):90.
Fontaine KR, Barofsky I. Obesity and health-related quality of life. Obes Rev. 2001;2(3):173–82.
Katz DA, McHorney CA, Atkinson RL. Impact of obesity on health-related quality of life in patients with chronic illness. J Gen Intern Med. 2000;15(11):789–96.
Kolotkin RL, Crosby RD, Williams GR. Health-related quality of life varies among obese subgroups. Obes Res. 2002;10(8):748–56.
Kolotkin RL, Andersen JR. A systematic review of reviews: exploring the relationship between obesity, weight loss and health-related quality of life. Clin Obes. 2017;7(5):273–89.
Nigatu YT, et al. The combined effects of obesity, abdominal obesity and major depression/anxiety on health-related quality of life: the lifelines cohort study. Plos One. 2016;11(2):e148871.
Karlsson J, et al. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. Int J Obes. 2000;24:1715.
Provencher V, et al. Eating behaviors and indexes of body composition in men and women from the Québec Family Study. Obes Res. 2003;11(6):783–92.
Cappelleri JC, et al. Psychometric analysis of the Three-Factor Eating Questionnaire-R21: results from a large diverse sample of obese and non-obese participants. Int J Obes. 2009;33:611.
de Lauzon-Guillain B, et al. Is restrained eating a risk factor for weight gain in a general population? Am J Clin Nutr. 2006;83(1):132–8.
Waller G, et al. Anger and core beliefs in the eating disorders. Int J Eat Disord. 2003;34(1):118–24.
Fassino S, et al. Mood, eating attitudes, and anger in obese women with and without Binge Eating Disorder. J Psychosom Res. 2003;54(6):559–66.
Appelhans BM, et al. Response style and vulnerability to anger-induced eating in obese adults. Eat Behav. 2011;12(1):9–14.
Schneider KL, et al. Trait anxiety, but not trait anger, predisposes obese individuals to emotional eating. Appetite. 2010;55(3):701–6.
Gnauer S, et al. Behandlungsprogramm für hochgradige Adipositas und psychische Komorbiditäten. JATROS Neurol Psychiatr. 2015;23(5):50–1.
Gnauer S, et al. Adipositas-Therapie im Psychosomatischen Zentrum Waldviertel – Lebensstilprogramm „Schwerelos“. In: Riffer F, et al., editor. Die Vielgestaltigkeit der Psychosomatik. Psychosomatik im Zentrum. Berlin, Heidelberg: Springer; 2017. pp. 109–19.
Franke GH, Derogatis LR. Die Symptom-Checkliste von Derogatis-Deutsche Version. Göttingen: Beltz; 1995.
Bullinger M, Kirchberger I, Ware J. Der deutsche SF-36 Health Survey. Übersetzung und psychometrische Testung eines krankheitsübergreifenden Instruments zur Erfassung der gesundheitsbezogenen Lebensqualität. Z Gesundheitswiss. 1995;3(1):21.
Pudel V, Westenhoefer J. Fragebogen zum Essverhalten. Three-Factor Eating Questionnaire-German Version. Göttingen: Hogrefe; 1989.
Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29(1):71–83.
Schwenkmezger P, Hodapp V, Spielberger C. Das State-Trait-Ärgerausdrucks-Inventar (STAXI). Mannheim: Huber; 1992.
Flegal KM, et al. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82.
Heneghan HM, et al. Weighing the evidence for an association between obesity and suicide risk. Surg Obes Relat Dis. 2012;8(1):98–107.
Peterhänsel C, et al. Risk of completed suicide after bariatric surgery: a systematic review. Obes Rev. 2013;14(5):369–82.
Rader S, et al. Effects of a web-based follow-up intervention on self-efficacy in obesity treatment for women. Wien Klin Wochenschr. 2017;129(13):472–81.
Zillikens MC, et al. Sex-specific genetic effects influence variation in body composition. Diabetologia. 2008;51(12):2233–41.
Power ML, Schulkin J. Sex differences in fat storage, fat metabolism, and the health risks from obesity: possible evolutionary origins. Br J Nutr. 2008;99(5):931–40.
Zlotnik A, et al. Determination of factors affecting glutamate concentrations in the whole blood of healthy human volunteers. J Neurosurg Anesthesiol. 2011;23(1):45–9.
Kautzky-Willer A, et al. Geschlechtsspezifische Aspekte für die klinische Praxis bei Prädiabetes und Diabetes mellitus. Wien Klin Wochenschr. 2016;128(2):151–8.
Foster JA, McVey Neufeld K‑A. Gut–brain axis: How the microbiome influences anxiety and depression. Trends Neurosci. 2013;36(5):305–12.
Schachter J, et al. Effects of obesity on depression: a role for inflammation and the gut microbiota. Brain Behav Immun. 2018;69:1–8.
Capuron L, Lasselin J, Castanon N. Role of adiposity-driven inflammation in depressive morbidity. Neuropsychopharmacology. 2017;42(1):115–28.
Castanon N, Luheshi G, Laye S. Role of neuroinflammation in the emotional and cognitive alterations displayed by animal models of obesity. Front Neurosci. 2015;9:229.
Burkert NT, et al. Self-perceived health, quality of life, and health-related behavior in obesity: Is social status a mediator? Wien Klin Wochenschr. 2012;124(7):271–5.
Ciarrochi J, Deane FP, Anderson S. Emotional intelligence moderates the relationship between stress and mental health. Pers Individ Dif. 2002;32(2):197–209.
Altamura M, et al. Alexithymia Predicts Attrition and Outcome in Weight-Loss Obesity Treatment. Front Psychol. 2018;9:2432.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F. Riffer, M. Sprung, H. Münch, E. Kaiser, L. Streibl, K. Heneis, and A. Kautzky-Willer declare that they have no competing interests.
Ethical standards
The present study was a retrospective analysis of data collected as part of routine clinical care and outcome evaluation, therefore approval by an ethics committee was not required; however, all procedures followed were in accordance with the ethical standards of the Helsinki Declaration of 1975 as revised in 2008. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
F. Riffer and M. Sprung contributed equally to this work.
Rights and permissions
About this article
Cite this article
Riffer, F., Sprung, M., Münch, H. et al. Relationship between psychological stress and metabolism in morbidly obese individuals. Wien Klin Wochenschr 132, 139–149 (2020). https://doi.org/10.1007/s00508-019-01583-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-019-01583-y