Abstract
Background
Acute kidney injury (AKI) significantly increases morbidity and mortality for hospitalized children, yet sociodemographic risk factors for pediatric AKI are poorly described. We examined sociodemographic differences in pediatric AKI amongst a national cohort of hospitalized children.
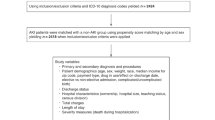
Methods
Secondary analysis of the most recent (2012) Kids’ Inpatient Database (KID) from the Agency for Healthcare Research and Quality. Study sample weights were used to obtain national estimates of AKI (defined by administrative data). KID is a nationally representative sample of pediatric discharges throughout the USA. Linear risk regression models were used to assess the relationship between our primary exposures (race/ethnicity, health insurance, household urbanization, gender, and age) and the diagnosis of AKI, adjusting for comorbidities.
Results
A total of 1,699,841 hospitalizations met our study criteria. In 2012, AKI occurred in approximately 12.3/1000 pediatric hospitalizations, which translates to almost 30,000 children nationally. Asian/Pacific Islander, African-American, and Hispanic children were at slightly increased risk for AKI compared to Caucasian children (adjusted risk difference (RD) 4.5 per 1000 hospitalizations, 95% confidence interval (CI) 2.9–6.0; 2.5/1000 hospitalizations, 95% CI 1.7–3.3; and 1.7/1000 hospitalizations, 95% CI 0.9–2.5, respectively). Uninsured children were more likely to suffer AKI compared to children with any health insurance (e.g., no insurance versus Medicaid: adjusted RD 14.4/1000 hospitalizations, 95% CI 12.7–16.2). Based on these national estimates, one episode of AKI might be prevented if 70 (95% CI 62–79) hospitalized children without insurance were provided with Medicaid.
Conclusions
Pediatric AKI occurs more frequently in racial minority and uninsured children, factors linked to lower socioeconomic status.




Similar content being viewed by others
References
Sutherland SM, Ji J, Sheikhi FH et al (2013) AKI in hospitalized children: epidemiology and clinical associations in a national cohort. Clin J Am Soc Nephrol. https://doi.org/10.2215/CJN.00270113
Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL (2017) Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med. https://doi.org/10.1056/NEJMoa1611391
McGregor TL, Jones DP, Wang L et al (2016) Acute kidney injury incidence in noncritically ill hospitalized children, adolescents, and young adults: a retrospective observational study. Am J Kidney Dis. https://doi.org/10.1053/j.ajkd.2015.07.019
Alkandari O, Eddington KA, Hyder A et al (2011) Acute kidney injury is an independent risk factor for pediatric intensive care unit mortality, longer length of stay and prolonged mechanical ventilation in critically ill children: a two-center retrospective cohort study. Crit Care. https://doi.org/10.1186/cc10269
Hessey E, Morissette G, Lacroix J et al (2018) Healthcare utilization after acute kidney injury in the pediatric intensive care unit. Clin J Am Soc Nephrol 13(5):685–692
Greenberg JH, Coca S, Parikh CR (2014) Long-term risk of chronic kidney disease and mortality in children after acute kidney injury: a systematic review. BMC Nephrol. https://doi.org/10.1186/1471-2369-15-184
Park S-K, Hur M, Kim E et al (2016) Risk factors for acute kidney injury after congenital cardiac surgery in infants and children: a retrospective observational study. PLoS One. https://doi.org/10.1371/journal.pone.0166328
Rheault MN, Zhang L, Selewski DT et al (2015) AKI in children hospitalized with nephrotic syndrome. Clin J Am Soc Nephrol. https://doi.org/10.2215/CJN.06620615
Nicholas SB, Kalantar-Zadeh K, Norris KC (2015) Socioeconomic disparities in chronic kidney disease. Adv Chronic Kidney Dis. https://doi.org/10.1053/j.ackd.2014.07.002
Shoham DA, Vupputuri S, Kaufman JS et al (2008) Kidney disease and the cumulative burden of life course socioeconomic conditions: the Atherosclerosis Risk in Communities (ARIC) study. Soc Sci Med. https://doi.org/10.1016/j.socscimed.2008.06.007
Vart P, Gansevoort RT, Joosten MM, Bültmann U, Reijneveld SA (2015) Socioeconomic disparities in chronic kidney disease: a systematic review and meta-analysis. Am J Prev Med. https://doi.org/10.1016/j.amepre.2014.11.004
HCUP Kids’ Inpatient Database (KID). Healthcare Cost and Utilization Project (HCUP). 2012. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/kidoverview.org. Published 2012. Accessed August 1, 2018
Mehta RL, Burdmann EA, Cerdá J et al (2016) Recognition and management of acute kidney injury in the International Society of Nephrology 0by25 global snapshot: a multinational cross-sectional study. Lancet. https://doi.org/10.1016/S0140-6736(16)30240-9
HCUP Chronic Condition Indicator (CCI). Healthcare Cost and Utilization Project (HCUP). 2012. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/toolssoftware/chronic/chronic.jsp. Published 2012. Accessed May 1, 2018
Hwang W, Weller W, Ireys H, Anderson G (2001) Out-of-pocket medical spending for care of chronic conditions. Health Aff. https://doi.org/10.1377/hlthaff.20.6.267
Staplin N, Herrington WG, Judge PK et al (2017) Use of causal diagrams to inform the design and interpretation of observational studies: an example from the study of heart and renal protection (SHARP). Clin J Am Soc Nephrol. https://doi.org/10.2215/CJN.02430316
Greenland S, Pearl J, Robins JM (1999) Causal diagrams for epidemiologic research. Epidemiology. https://doi.org/10.1097/00001648-199901000-00008
Hernán MA, Hernández-Díaz S, Robins JM (2004) A structural approach to selection bias. Epidemiology. https://doi.org/10.1097/01.ede.0000135174.63482.43
United States Census Bureau. Quick Facts United States. https://census.gov/quickfacts/fact/table/US/pst045218. Accessed December 2, 2019
National Center for Education Statistics. Estimates of resident population, by race/ethnicity and age group: selected years, 1980 through 2016. https://nces.ed.gov/programs/digest/d16/tables/dt16_101.20.asp?referer=raceindicators. Accessed December 2, 2019
Abdullah F, Zhang Y, Lardaro T et al (2010) Analysis of 23 million US hospitalizations: uninsured children have higher all-cause in-hospital mortality. J Public Health (Bangkok) 32(2):236–244. https://doi.org/10.1093/pubmed/fdp099
Office of Disease Prevention and Health Promotion. Social Determinants of Health | Healthy People 2020. Healthy People 2020 Topics and Objectives. https://www.healthypeople.gov. Published 2015
Centers for Medicare & Medicaid Services. Medicaid.gov. https://www.medicaid.gov. Published 2018. Accessed August 7, 2018
Centers for Medicare & Medicaid Services. Healthcare.gov. https://www.healthcare.gov/medicaid-chip/. Published 2018. Accessed August 7, 2018
Benefits.gov. State Children’s Health Insurance Program. https://benefits.gov/benefits/benefit-details/607. Published 2018. Accessed August 8, 2018
Hidalgo G, Ng DK, Moxey-Mims M et al (2013) Association of income level with kidney disease severity and progression among children and adolescents with CKD: a report from the chronic kidney disease in children (CKiD) study. Am J Kidney Dis. https://doi.org/10.1053/j.ajkd.2013.06.013
Shone LP, Dick AW, Brach C et al (2003) The role of race and ethnicity in the state Children’s health insurance program (SCHIP) in four states: are there baseline disparities, and what do they mean for SCHIP? Pediatrics. https://doi.org/10.1542/peds.112.6.SE1.521
Scott JW, Rose JA, Tsai TC et al (2016) Impact of ACA insurance coverage expansion on perforated appendix rates among young adults. Med Care. https://doi.org/10.1097/MLR.0000000000000586
Olabisi OA, Heneghan JF (2017) APOL1 nephrotoxicity: what does ion transport have to do with it? Semin Nephrol. https://doi.org/10.1016/j.semnephrol.2017.07.008
Ng DK, Robertson CC, Woroniecki RP et al (2017) APOL1-associated glomerular disease among African-American children: a collaboration of the chronic kidney disease in children (CKiD) and nephrotic syndrome study network (NEPTUNE) cohorts. Nephrol Dial Transplant. https://doi.org/10.1093/ndt/gfw061
Woroniecki RP, Ng DK, Limou S et al (2016) Renal and cardiovascular morbidities associated with APOL1 status among African-American and non-African-American children with focal segmental glomerulosclerosis. Front Pediatr. https://doi.org/10.3389/fped.2016.00122
Parsa A, Kao WHL, Xie D et al (2013) APOL1 risk variants, race, and progression of chronic kidney disease. N Engl J Med. https://doi.org/10.1056/NEJMoa1310345
Friedman DJ (2017) A brief history of APOL1: a gene evolving. Semin Nephrol. https://doi.org/10.1016/j.semnephrol.2017.07.003
Grams ME, Matsushita K, Sang Y et al (2014) Explaining the racial difference in AKI incidence. J Am Soc Nephrol. https://doi.org/10.1681/ASN.2013080867
Zhao B, Lu Q, Cheng Y et al (2017) A genome-wide association study to identify single-nucleotide polymorphisms for acute kidney injury. Am J Respir Crit Care Med. https://doi.org/10.1164/rccm.201603-0518OC
United States Renal Data System (2017) USRDS annual data report: epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda. https://doi.org/10.1053/j.ajkd.2017.01.020
Neugarten J, Golestaneh L (2018) Female sex reduces the risk of hospital-associated acute kidney injury: a meta-analysis. BMC Nephrol. https://doi.org/10.1186/s12882-018-1122-z
Grams ME, Waikar SS, MacMahon B, Whelton S, Ballew SH, Coresh J (2014) Performance and limitations of administrative data in the identification of AKI. Clin J Am Soc Nephrol. https://doi.org/10.2215/CJN.07650713
Ko S, Venkatesan S, Nand K, Levidiotis V, Nelson C, Janus E (2018) International statistical classification of diseases and related health problems coding underestimates the incidence and prevalence of acute kidney injury and chronic kidney disease in general medical patients. Intern Med J. https://doi.org/10.1111/imj.13729
Borzecki AM, Cevasco M, Chen Q, Shin M, Itani KMF, Rosen AK (2011) How valid is the AHRQ patient safety indicator postoperative physiologic and metabolic derangement? J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2011.01.001
Waikar SS, Wald R, Chertow GM et al (2006) Validity of international classification of diseases, ninth revision, clinical modification codes for acute renal failure. J Am Soc Nephrol 17(6):1688–1694. https://doi.org/10.1681/ASN.2006010073
Acknowledgments
We would like to acknowledge all the HCUP Data Partners that contribute to HCUP because without their contributions, our work would not have been possible. The full list of state organizations can be found at: https://www.hcup-us.ahrq.gov/db/hcupdatapartners.jsp.
Funding
ECB was supported by NIH/NIDDK T32-DK00775 Training Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The institutional review board at the University of North Carolina at Chapel Hill reviewed this secondary data analysis of de-identified data and classified this as non-human subjects research status.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bjornstad, E.C., Marshall, S.W., Mottl, A.K. et al. Racial and health insurance disparities in pediatric acute kidney injury in the USA. Pediatr Nephrol 35, 1085–1096 (2020). https://doi.org/10.1007/s00467-020-04470-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04470-1