Abstract
Background
Primary vesicoureteral reflux (PVUR) is the most common malformation of the kidney and urinary tract, and reflux nephropathy is a major cause of chronic kidney disease in children. Recently, we reported mutations in the tenascin XB gene (TNXB) as a cause of PVUR with joint hypermobility.
Methods
To define the role of rare variants in tenascin genes in the etiology of PVUR, we screened a cohort of patients with familial PVUR (FPVUR) and non-familial PVUR (NFPVUR) for rare missense variants inTNXB and the tenascin C gene (TNC) after excluding mutations in ROBO2 and SOX17.
Results
The screening procedure identified 134 individuals from 112 families with PVUR; two families with mutations in ROBO2 were excluded from further analysis. Rare missense variants in TNXB were found in the remaining 110 families, of which 5/55 (9 %) families had FPVUR and 2/55 (4 %) had NFPVUR. There were no differences in high-grade reflux or renal parenchymal scarring between patients with and without TNXB variants. All patients with TNXB rare variants who were tested exhibited joint hypermobility. Overall we were able to identify causes of FPVUR in 7/57 (12 %) families (9 % in TNXB and 3 % in ROBO2).
Conclusions
In conclusion, the identification of a rare missense variant in TNXB in combination with a positive family history of VUR and joint hypermobility may represent a non-invasive method to diagnose PVUR and warrants further evaluation in other cohorts.


Similar content being viewed by others
References
Mak RH, Kuo HJ (2004) Primary ureteral reflux: emerging insights from molecular and genetic studies. Curr Opin Pediatr 15:181–185
Smellie JM, Normand IC (1975) Bacteriuria, reflux, and renal scarring. Arch Dis Child 50:581–585
Arant BS Jr (1991) Vesicoureteric reflux and renal injury. Am J Kidney Dis 17:491–511
North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS) (2010) NAPRTCS Annual Transplant Report. NAPRTCS Data Coordinating Center,The EMMES Corporation, Boston, MA. Available at: https://web.emmes.com/study/ped/annlrept/2010_Report.pdf
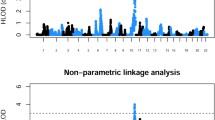
Kelly H, Molony CM, Darlow JM, Pirker ME, Yoneda A, Green AJ, Puri P, Barton DE (2007) A genome-wide scan for genes involved in primary vesicoureteric reflux. J Med Genet 44:710–717
Feather SA, Malcolm S, Woolf AS, Wright V, Blaydon D, Reid CJ, Flinter FA, Proesmans W, Devriendt K, Carter J, Warwicker P, Goodship TH, Goodship JA (2000) Primary, non-syndromic vesicoureteric reflux and its nephropathy is genetically heterogeneous, with a locus on chromosome 1. Am J Hum Genet 66:1420–1425
Weng PL, Sanna-Cherchi S, Hensle T, Shapiro E, Werzberger A, Caridi G, Izzi C, Konka A, Reese AC, Cheng R, Werzberger S, Schlussel RN, Burk RD, Lee JH, Ravazzolo R, Scolari F, Ghiggeri GM, Glassberg K, Gharavi AG (2009) A recessive gene for primary vesicoureteral reflux maps to chromosome 12p11-q13. J Am Soc Nephrol 20:1633–1640
Ashraf S, Hoskins BE, Chaib H, Hoefele J, Pasch A, Saisawat P, Trefz F, Hacker HW, Nuernberg G, Nuernberg P, Otto EA, Hildebrandt F (2010) Mapping of a new locus for congenital anomalies of the kidney and urinary tract on chromosome 8q24. Nephrol Dial Transplant 25:1496–1501
Gbadegesin RA, Brophy PD, Adeyemo A, Hall G, Gupta IR, Hains D, Bartkowiak B, Rabinovich CE, Chandrasekharappa S, Homstad A, Westreich K, Wu G, Liu Y, Holanda D, Clarke J, Lavin P, Selim A, Miller S, Wiener JS, Ross SS, Foreman J, Rotimi C, Winn MP (2013) TNXB mutations can cause vesicoureteral reflux. J Am Soc Nephrol 24:1313–1322
Zweers MC, Bristow J (2003) Haploinsufficiency of TNXB is associated with hypermobility type of Ehlers–Danlos syndrome. Am J Hum Genet 73:214–217
Schaller MD, Parsons JT (1994) Focal adhesion kinase and associated proteins. Curr Opin Cell Biol 6:705–710
Petersen JW, Douglas JY (2013) Tenascin-X, collagen, and Ehlers-Danlos syndrome: tenascin-X gene defects can protect against adverse cardiovascular events. Med Hypotheses 81:443–447
Chiquet-Ehrismann R, Tucker RP (2011) Tenascins and the importance of adhesion modulation. Cold Spring Harb Perspect Biol 3:11–19
Smits-Engelsman B, Klerks M, Kirby A (2011) Beighton score: a valid measure for generalized hypermobility in children. J Pediatr 158:119–123
Sunyaev S, Ramensky V, Koch I, Lathe W 3rd, Kondrashov AS, Bork P (2001) Prediction of deleterious human alleles. Hum Mol Genet 10:591–597
Kumar P, Henikoff S, Ng PC (2009) Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc 4:1073–1081
Lu W, van Eerde AM, Fan X, Quintero-Rivera F, Kulkarni S, Ferguson H, Kim HG, Fan Y, Xi Q, Li QG, Sanlaville D, Andrews W, Sundaresan V, Bi W, Yan J, Giltay JC, Wijmenga C, de Jong TP, Feather SA, Woolf AS, Rao Y, Lupski JR, Eccles MR, Quade BJ, Gusella JF, Morton CC, Maas RL (2007) Disruption of ROBO2 is associated with urinary tract anomalies and confers risk of vesicoureteral reflux. Am J Hum Genet 80:616–632
Bertoli-Avella AM, Conte ML, de Punzo F, Graaf BM, Lama G, La Manna A, Polito C, Grassia C, Nobili B, Rambaldi PF, Oostra BA, Perrotta S (2008) ROBO2 gene variants are associated with familial vesicoureteral reflux. J Am Soc Nephrol 19:825–831
Gimelli S, Caridi G, Beri S, McCracken K, Bocciardi R, Zordan P, Dagnino M, Fiorio P, Murer L, Benetti E, Zuffardi O, Giorda R, Wells JM, Gimelli G, Ghiggeri GM (2010) Mutations in SOX17 are associated with congenital anomalies of the kidney and the urinary tract. Hum Mutat 31:1352–1359
Combes P, Planche V, Eymard-Pierre E, Sarret C, Rodriguez D, Boespflug-Tanguy O, Vaurs-Barriere C (2012) Relevance of SOX17 variants for hypomyelinating leukodystrophies and congenital anomalies of the kidney and urinary tract (CAKUT). Ann Hum Genet 76:261–267
Hwang DY, Dworschak GC, Kohl S, Saisawat P, Vivante A, Hilger AC, Reutter HM, Soliman NA, Bogdanovic R, Kehinde EO, Tasic V, Hildebrandt F (2014) Mutations in 12 known dominant disease-causing genes clarify many congenital anomalies of the kidney and urinary tract. Kidney Int 85:1429–1433
Ichikawa I, Kuwayama F, Pope JC 4th, Stephens FD, Miyazaki Y (2002) Paradigm shift from classic anatomic theories to contemporary cell biological views of CAKUT. Kidney Int 61:889–898
Acknowledgments
This study was supported by the National Institutes of Health (NIH) and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant R21DK096200 and the Bayden Collins Pediatric Kidney Disease Research Fund, Duke University Medical Center. RG is the recipient of the Doris Duke Clinical Research Mentorship grant. We would like to thank the personnel of the genomic core of the Duke Molecular Physiology Institute (DMPI) and most importantly the participants in the study.
Conflict of interest
All the authors declared no competing interests.
Ethical disclosure
Institutional review board approval was obtained from Duke University Medical Center (Durham, NC). We obtained informed consent from parents and assent from children participating in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study is dedicated to the memory of Michelle P. Winn, MD for her seminal contribution to the field of nephrology and, most importantly, for being a great teacher and an outstanding mentor.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 697 kb)
Rights and permissions
About this article
Cite this article
Elahi, S., Homstad, A., Vaidya, H. et al. Rare variants in tenascin genes in a cohort of children with primary vesicoureteric reflux. Pediatr Nephrol 31, 247–253 (2016). https://doi.org/10.1007/s00467-015-3203-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-015-3203-6