Abstract
Background
The influence of experience on the results of treatment with laparoscopic surgery is indisputable. The establishment of indications and contraindications is relative, and varies depending on the experience of the surgeon. Learning curves have been described for a number of laparoscopic interventions, in particular laparoscopic cholecystectomy. The current prospective multicenter study investigates, among other things, the interrelation between experience and the results of treatment using laparoscopic colorectal surgery. The study makes no pronouncements on the long-term results achieved in patients with colorectal carcinoma who underwent an operation with curative intent, although relevant data were indeed collected.
Results
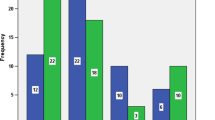
Between August 1, 1995 and February 1, 1999, a total of 1,658 patients were recruited to the prospective multicenter study initiated by the Laparoscopic Colorectal Surgery Study Group. To investigate the influence of surgical experience, two groups were formed. Group A comprised all the institutions and surgeons with experience of more than 100 laparoscopic colorectal operations. Group B contained institutions and surgeons with experience of fewer than 100 such interventions. The results of this study clearly show that in Group A, significantly more procedures involving the rectum were performed (26.7% vs 9.5%), and significantly more carcinomas were surgically managed (37.3% vs 17.3%). Despite this significantly higher level of technically difficult procedures in the patient population of group A, which was comparable in terms of age, gender, height, and weight with the patient in group B, the postoperative mortality and morbidity was, with the exception of urinary tract infections, identical between the two groups. Conversion to open surgery was significantly less frequent in group A (4.3% vs 6.9%), and, finally, the duration of the procedures performed by the more experienced surgeons of group A was appreciably shorter than in institutions with a smaller frequency of such operations.
Conclusions
Laparoscopic colorectal surgery is very demanding, and can be performed with low morbidity and mortality rates only by a surgeon with above-average experience with this type of surgery and a large caseload of laparoscopic colorectal procedures. The learning curve for such procedures is appreciably longer than for other laparoscopic operations. With increasing experience, technically more demanding operations, including radical oncologic rectal laparoscopic procedures, can be performed with appreciably reduced operating times and conversion rates, but with no increase in morbidity or mortality.
Similar content being viewed by others
References
Agachan F, Joo JS, Sher M, Weiss EG, Nogueras JJ, Wexner SD (1997) Laparoscopic colorectal surgery: do we get faster? Surg Endosc 11: 331–335 DOI: 10.1007/s004649900357
Agachan F, Joo JS, Weiss EG, Wexner SD (1996) Intraoperative laparoscopic complications: are we getting better? Dis Colon Rectum 39 (Suppl 10): 14–19
Bennett CL, Stryker SJ, Fereira MR, Adams J, Beart RW (1997) The learning curve for laparoscopic colorectal surgery: preliminary results from a prospective analysis of 1,194 laparoscopic-assisted colectomies. Arch Surg 132:41–44 discussion 45
Bruch H, Schiedeck Th, Schwandner O (1999) Laparoscopic colorectal surgery: a five-year experience. Dig Surg 16: 45–54
Cagir B, Rangraj M, Maffuci L, Herz BL (1994) The learning curve for laparoscopic cholecystectomy. J Laparoendosc Surg 4: 419–427
Christen D, Buchmann P (1996) Sources of hazards in laparoscopic colon surgery and how to avoid them. Swiss Surg 2: 203–207
Hunkeler R, Gerst P, Seifert M, Wehrli H (1997) Laparoscopic colon surgery in the regional hospital initial experiences after 65 interventions. Schweiz Med Wochenschr Suppl 89: 25–30
Köckerling F, Reymond MA, Schneider C, Wittekind C, Scheidbach H, Konradt J, Köhler L, Bärlehner E, Kuthe A, Bruch HP, Hohenberger W, Laparoscopic Colorectal Surgery Study Group (LCSSG) (1998) Prospective multicenter study of the quality of oncologic resections in patients undergoing laparoscopic colorectal surgery for cancer. Dis Colon Rectum 41: 963–970
Köckerling F, Rose J, Schneider C, Scheidbach H, Scheuerlein H, Reymond MA, Reck T, Konradt J, Bruch HP, Zornig C, Bärlehner E, Kuthe A, Szinicz G, Richter HA, Hohenberger W, Laparoscopic Colorectal Surgery Study Group (LCSSG) (1999) Laparoscopic colorectal anastomosis: risk of postoperative leakage: results of a multicenter study. Surg Endosc 13: 639–644 DOI: 10.1007/s004649900639
Köckerling F, Schneider C, Reymond MA, Scheidbach H, Konradt J, Bärlehner E, Bruch HP, Kuthe A, Troidl H, Hohenberger W, Laparoscopic Colorectal Surgery Study Group (LCSSG) (1998) Early results of a prospective multicenter study on 500 consecutive cases of laparoscopic colorectal surgery. Surg Endosc 12: 37–41 DOI: 10.1007/s004649900588
Köckerling F, Schneider C, Reymond MA, Scheidbach H, Scheuerlein H, Konradt J, Bruch HP, Zornig C, Köhler L, Kuthe A, Szinicz G, Richter HA, Hohenberger W, Laparoscopic Colorectal Surgery Study Group (LCSSG) (1999) Laparoscopic resection of sigmoid diverticulitis: results of a multicenter study. Surg Endosc 13: 567–571 DOI: 10.1007/s004649901042
Larach SW, Patankar SK, Ferrara A, Williamson PR, Perozo SE, Lord AS (1997) Complications of laparoscopic colorectal surgery: analysis and comparison of early vs later experience. Dis Colon Rectum 40: 592–596
Lekawa M, Shapiro SJ, Gordon LA, Rothbart J, Hiatt JR (1995) The laparoscopic learning curve. Surg Laparosc Endosc 5: 455–458
Liem MS, van Steensel CJ, Boelhouwer RU, Weidema WF, Clevers GJ, Meijer WS, Vente JP, de Vries LS, van Vroonhoven TJ (1996) The learning curve for totally extraperitoneal laparoscopic inguinal hernia repair. Am J Surg 171: 281–285
Lord SA, Larach SW, Ferrara A, Williamson PR, Lago CP, Lube MW (1996) Laparoscopic resections for colorectal carcinoma: a three-year experience. Dis Colon Rectum 39: 148–154
Marusch F, Koch A, Kube R, Gastinger I (1999) Laparoscopic creation of stomas: an ideal single indication in minimally invasive surgery. Chirurg 70: 785–788
Rege RV, Joehl RJ (1999) A learning curve for laparoscopic splenectomy at an academic institution. J Surg Res 81: 27–32
Reissman P, Cohen S, Weiss EG, Wexner SD (1996) Laparoscopic colorectal surgery: ascending the learning curve. World J Surg 20: 277–281 discussion 282
Sanabria JR, Gallinger S, Croxford R, Strasberg SM (1994) Risk factors in elective laparoscopic cholecystectomy for conversion to open cholecystectomy. J Am Coll Surg 179: 696–704
Schiedeck THK, Schwandner O, Bruch HP (1998) Laparoscopic sigmoid resection in diverticulitis. Chirurg 69: 846–853
Schirmer BD (1996) Laparoscopic colon resection. Surg Clin North Am 76: 571–583
Schwandner O, Schiedeck THK, Bruch HP (1999) The role of conversion in laparoscopic colorectal surgery: do predictive factors exist? Surg Endosc 13: 151–156 DOI: 10.1007/s004649900927
See WA, Cooper CS, Fisher JR (1993) Predictors of laparoscopic complications after formal training in laparoscopic surgery. JAMA 270: 2689–2692
Senagore AJ, Luchtefeld MA, Mackeigan JM (1995) What is the learning curve for laparoscopic colectomy? Am Surg 61: 681–685
Sher ME, Agachan F, Bortul M, Nogueras JJ, Weiss EG, Wexner SD (1997) Laparoscopic surgery for diverticulitis. Surg Endosc 11: 264–267 DOI: 10.1007/s004649900340
Sjodahl R, Nystrom PO (1998) Laparoscopic colorectal surgery in progress. Eur J Surg Suppl 582: 124–127
Slim K, Pezet D, Riff Y, Clark E, Chipponi J (1995). High morbidity rate after converted laparoscopic colorectal surgery. Br J Surg 82: 1406–1408
Watson DI, Baigrie RJ, Jamieson GG (1996). A learning curve for laparoscopic fundoplication: definable, avoidable, or waste of time? Ann Surg 224: 198–200
Wishner JD, Baker JW Jr, Hoffman GC, Hubbard GW II, Gould RJ, Wohlgemuth SD, Ruffin WK, Melick CF (1995) Laparoscopic-assisted colectomy: the learning curve. Surg Endosc 9: 1179–1183
Author information
Authors and Affiliations
Consortia
Additional information
Laparoscopic Colorectal Surgery Study Group (LCSSG)
Online publication: 12 December 2000
Supported by Ethicon Endosurgery, Norderstedt, Germany, and Takeda Pharma, Aachen, Germany
Rights and permissions
About this article
Cite this article
Marusch, F., Gastinger, I., Schneider, C. et al. Experience as a factor influencing the indications for laparoscopic colorectal surgery and the results. Surg Endosc 15, 116–120 (2001). https://doi.org/10.1007/s004640000340
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s004640000340