Abstract
Background
Force feedback is a critical element for performing and learning surgical suturing skill. Force feedback is impoverished or not present at all in non-open surgery (i.e., in simulation, laparoscopic, and robotic-assisted surgery), but it can be augmented using different modalities. This rapid, systematic review examines how the modality of delivering force feedback influences the performance and learning of surgical suturing skills.
Methods
An electronic search was performed on PubMed/MEDLINE, Web of Science, and Embase databases to identify relevant articles. The results were synthesized using vote counting based on direction of effect.
Results
A total of nine studies of medium-to-low quality were included. The synthesis of results suggests that the visual modality could be more beneficial than the tactile and auditory modalities in improving force control and that auditory and tactile modalities could be more beneficial than the visual modality in improving suturing performance. Results are mixed and unclear with regards to how modality affects the reduction of force magnitude and unclear when unimodal was compared to multimodal feedback. The studies have a general low level of evidence.
Conclusion
The low number of studies with low methodological quality and low level of evidence (most were proof of concept) prevents us from drawing any meaningful conclusion and as such it is currently unknown whether and how force feedback modality influences surgical suturing skill. Speculatively, the visual modality may be more beneficial for improving the control of exerted force, while auditory and tactile modalities may be more effective in improving the overall suturing performance. We consider the issue of feedback modality to be highly relevant in this field, and we encourage future research to conduct further investigation integrating principles from learning psychology and neuroscience: identify feedback goal, context, and skill level and then design and compare feedback modalities accordingly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Force feedback is a critical element for performing and learning surgical suturing skill [1, 2]. The suturing skill consists of driving and inserting a needle through the operated tissue, pulling the suture to close the wound, and tightly tying a knot to secure the suture. In this skill, perceiving the force exerted on the operated tissue allows an operator (surgeon or student) to properly handle instrument and tissue to successfully carry out the suturing procedure, tying a knot without leaking and avoiding damage to the tissue. We refer to force feedback as the feedback provided by a device/instrument concerning the use of forces and torques [3]. While being readily available to an operator in open surgery (primarily through the haptic sense), force feedback is impoverished or not present at all in non-open surgery (i.e., in simulation, laparoscopic, and robotic-assisted surgery). It is largely reduced in laparoscopic suturing due to presence of friction between the moving components inside the instrument and friction between trocar valves and instrument shaft, and it is absent in most robotic-assisted suturing (see the Senhance® surgical laparoscopic system for an exception). The lack of force feedback represents a critical issue for the performance of non-open surgical suturing and for the design of training interventions for medical students [4]. Surgeons themselves acknowledge the need for augmenting force feedback [5].
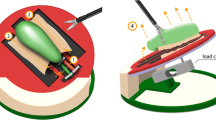
Recent technological developments allow for the provision of force feedback to an operator. Sensors placed on the instrument tip or below a tissue in simulation devices can capture the exerted force (e.g., see [6]). Force can then be delivered through augmented feedback and provide an operator with the sense of how much force they are applying on the suture and tissue. This in turn is expected to improve an operator’s control of force and consequently their suturing performance. Previous research has shown that augmenting force feedback is indeed effective in reducing the exerted force, improving an operator’s control of force, and there is some evidence that it can also improve suturing performance [3, 7, 8]. Importantly, force feedback can be delivered using different modalities: visual, auditory, tactile, and their combinations. For instance, pulling forces during knot tying can be delivered visually [9, 10], overlaying a force vector onto the laparoscopic video [11] or directly at the hand through tactile-based solutions [12]. Given the breadth of feedback modality options, the contexts in which feedback is needed (e.g., operating room or simulation-based training), and the goals for delivering feedback (i.e., assisting performance or promoting learning), it is highly relevant to examine the benefits and constraints of the different modalities of delivering force feedback.
The modality of delivering force feedback likely influences the performance and learning of surgical suturing skill. Considering that force in a suturing task is primarily controlled using tactile and kinesthetic sensory information [13, 14], one might think that the tactile modality is superior to the other modalities. However, the way a certain feedback modality influences learning and performance processes is complex and depends on its interaction with task complexity, a performer’s skill level, the goal of an intervention, and the environment in which feedback is expected to be used [15]. Research in motor skill learning provides evidence and some guidelines on how feedback modality operates in some specific situations. Importantly, skill performance and skill learning are two different constructs [16, 17] and a feedback modality may enhance performance but interfere with learning and vice versa. For example, the tactile modality has been shown to promote enhanced skill performance relative to the auditory modality in simple tasks and in novices, but the modality effect is reversed in complex tasks and in experts [18, 19]; auditory feedback is generally superior to visual in promoting learning, while visual might be better than auditory for performance, with different underlying neural activities [20, 21]. Furthermore, research in neuroscience and psychophysics is increasingly recognizing that feedback perception is a multimodal process, highlighting the benefits of multimodal over unimodal feedback [22, 23]. It is quite clear that choosing a feedback modality is a non-trivial and complex issue. Its effect cannot be generalized toward one modality or another (one size does not fit all), but modality effect has to be investigated in a specific skill (surgical suturing skill), population (students and surgeons), context (operating room and simulation-based training), and goal (assisting performance and promoting learning).
This review was conducted to examine how the modality of delivering force feedback influences the performance and learning of surgical suturing skills in laparoscopy. The results of this study can provide insights for the design of skill training interventions and assistance and can inform manufacturers of surgical-related instruments and trainers on the feedback modality to implement in their systems. For example, implementing haptics in a robotic simulator is expensive [24]. The results can inform whether such modality is essential and, if it is, it can justify the expense.
Methods
The guidelines proposed by the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020 [25]) and the guidelines from the Cochrane Rapid Reviews Methods Group [26] were followed. The research team, comprising experts in conducting systematic reviews (LO and SS) and surgery (FB), collectively designed the review process.
Eligibility criteria
Inclusion criteria were set using a PICOS statement:
P (population): humans (students and surgeons).
I (intervention): force exerted on instrument–tissue interaction (pushing or pulling) is augmented during a surgery suturing task.
C (comparator): two or more feedback modalities of delivering force feedback are compared.
O (outcome): force parameters (main outcome) and surgical performance parameters (secondary outcome).
S (study design): experimental, quasi-experimental, and cross-over.
Studies that compared variations within a single feedback modality (e.g., different types of visual feedback) were not included. Furthermore, only peer-reviewed studies published in English were included.
Information sources and search strategy
Three databases were searched to identify eligible studies: Pubmed, Web of Science, and Embase. The search was performed on the 14th of June 2022 and updated on the 4th of October 2022. Furthermore, the references of the studies included in the review were screened for identifying additional studies.
The search string comprised the following syntax: (force* OR kinesthe* OR pressure OR strength OR torque* OR tension) AND (feedback OR biofeedback OR substitution OR simulat* OR render* OR “virtual reality” OR “mixed reality” OR “augmented reality” OR “box trainer”) AND (haptic* OR tactile OR tactual OR vibro-tactile OR vibration OR audio OR auditory OR acoustic OR visual OR verbal OR modalit* OR type) AND (surgery OR surgic* OR laparoscop*) AND (sutur* OR knot-tying OR “knot tying” OR knot* OR “tissue manipulation” OR needle-driving OR “needle driving”).
Selection process
The records identified through the database search were exported into Endnote X9 software (Clarivate) and duplicates were removed automatically first and then manually. One author (LO) screened titles and abstracts first and then the full texts. A second reviewer (KG) checked the excluded records, and any discrepancy was resolved in a closed meeting. If consensus was not reached, a third author (FB) was consulted (Fig. 1).
Data collection process and data items
The following data were extracted from each study: general study information (author, year, study design), sample characteristics, study setting, suturing task and force parameter, feedback strategy, and outcome measures. One author (LO) extracted the data and a second author (KG) assessed data accuracy (Table 1).
Study risk of bias assessment
The Risk of Bias tools developed by the Cochrane group were used for the risk of bias assessment [27]. Considering the design of the included studies (one RCT and cross-over trials), the RoB 2.0 tool was used. This tool is primarily designed for RCTs and is composed of five bias domains: (1) randomization process, (2) deviations from the intended interventions, (3) missing outcome data, (4) measurement of the outcome, and (5) selection of the reported results. A modified version of the tool, which contains the five domains just described and an additional domain for bias arising from period and carryover effects, was used for cross-over trials. Signaling questions help the assessment of the potential bias in each domain. Each domain has three possible outcomes—low, some concerns, and high. An overall outcome, corresponding to the highest risk across domains was calculated for each study (i.e., if the risk was some concerns in one domain only but low in all other domains, the overall risk was some concerns). The results of the risk of bias assessment are presented using the traffic light system: green (low), yellow (some concerns), and red (high) (see Table 2). One author (LO) assessed the risk of bias using the excel spreadsheet available at https://www.riskofbias.info/welcome and a second author (KG) assessed data accuracy.
Synthesis methods
Due to inconsistency of the effect measures and data reported across studies, it was not possible to compute a meta-analysis, and we decided to synthesize results using vote counting based on direction of effect. Despite some limitations (i.e., does not provide an estimate of effect magnitude, does not account for different study sizes, and it is less powerful than combining p values), this synthesis is a valid method for estimating the overall direction of an effect [28]. The direction of effect was calculated in each study from descriptive statistics or graphs on the outcome of interest. In the context of comparing two feedback modalities, three direction outcomes were possible: in favor of one modality, in favor of the other modality in the comparison, or no change/mixed effects/conflicting findings [29]. An effect was classified in favor of one modality or the other when at least 70% of the analyzed outcomes reported a similar direction, while it was classified no change/mixed effects/conflicting findings if otherwise. Statistical significance was not considered for assessing the direction [30]. Studies were first grouped by the compared modality(ies) (Table 3) and then they were grouped by the examined task(s) (Table 4). It would have been highly relevant to group studies in learning-focused and performance-focused studies; however, only one study evaluated skill learning (see overview of study characteristics for more details) and it was not possible to perform such grouping. In both cases, participants with different skill levels were combined, as studies did not report any modality–skill level interaction effect. Some studies had different intervention conditions (e.g., compared unimodal and multimodal modalities) and appear in the synthesis multiple times with different results. The effect direction was synthesized using the sign test: nonparametric test computed to examine the probability of observing the obtained direction of effect if the null hypothesis (i.e., equal number in one direction and the other) were true [31]. The number of results in favor of one modality or another was counted, and the p-value was computed using the sign and binomial test on GraphPad website (https://www.graphpad.com/quickcalcs/binomial1/).
Results
Search
The search resulted in a total of 840 studies (234 in Pubmed, 242 in Web of Science, and 364 in Embase). After duplicates removal, 529 studies were screened and 502 were excluded based on their title or abstract. Twenty-seven full texts were then screened and 18 studies were excluded because did not meet the inclusion criteria. As such, a total of nine studies were included in the review (Fig. 1).
Overview of study characteristics
A detailed description of the studies is presented in Table 1. One study was a Randomized Controlled Trial (RCT) [32], while the other eight studies adopted a cross-over design, whereby each participant was exposed to different feedback conditions [33,34,35,36,37,38,39,40]. Only the RCT, comprised a learning phase and a post-test without feedback, evaluated the effect of feedback on skill learning, while the other studies evaluated the effect of feedback on skill performance. A total of 141 participants were recruited with a median sample size of 8. Three studies recruited novices only, two studies recruited participants with an intermediate skill level, and the other studies recruited a mix of novices, intermediates and experts. The number of practice trials performed in each experimental condition (or group) varied between 3 and 30, with a median of 5. One study used an entire surgical suturing task, while the other studies isolated the single components (i.e., inserting the needle, pulling the suture, and tying the knot). Except for two studies that adopted a laparoscopic or open simulator, robotics-assisted and tele-operated surgical systems were employed. With regards to the modality of delivering force feedback, all studies compared visual with either tactile or auditory modality, and most studies also compared unimodal (visual, tactile, auditory) with multimodal feedback (combination of visual with tactile or auditory). Lastly, outcome measures included force magnitude in all studies, force control, and suturing performance in some studies.
Study risk of bias
The methodological quality of the studies is predominantly low: two studies had ‘some concerns’ [32, 33], and the others had a high risk of bias [34,35,36,37,38,39,40]. The randomization procedure in most cases was poorly conducted or reported, and it was not reported whether the randomization of feedback conditions was counter-balanced in cross-over studies [33,34,35,36,37,38,39,40]. Furthermore, in some cases it was not reported whether all participants and outcomes were included in the analysis [34, 37,38,39,40], and how the analysis estimated the effect of assignment to intervention. Lastly, none of the studies reported how data analysis was planned before data collection and eventually adapted during/after data collection.
Synthesis of results
The effect direction plot of studies grouped by the examined modality is presented in Table 3.
Visual vs tactile or auditory
Reduction of force magnitude The direction of effect is mixed.
Improvement of force control The effect is in the direction of the visual modality (p = 0.13), with three studies out of three in favor of this modality.
Improvement of suturing performance The effect is in the direction of the modality other than the visual (p = 0.13). Two studies are in favor of the tactile modality, one in favor of the auditory modality, and none in favor of the visual modality.
Visual vs multimodal (visual + tactile or auditory)
Reduction of force magnitude The direction of effect is mixed.
Improvement of force control The direction of effect is mixed.
Improvement of suturing performance The effect of the only study included is in the direction of a multimodal strategy (visual + tactile).
Tactile vs multimodal (tactile + visual)
Reduction of force magnitude The direction of effect is mixed.
Improvement of force control The effect of the only study included is mixed/unclear.
Improvement of suturing performance The effect of the only study included is mixed/unclear.
The effect direction plot of studies grouped by the examined task is presented in Table 4.
Needle inserting task
Reduction of force magnitude The direction of effect is mixed both for unimodal and multimodal comparisons.
Improvement of suturing performance The direction of effect is mixed both for unimodal and multimodal comparisons.
Suture pulling task
Reduction of force magnitude The direction of effect is mixed both for unimodal and multimodal comparisons.
Improvement of force control The direction of effect is mixed both for unimodal and multimodal comparisons.
Knot-tying task
Reduction of force magnitude The direction of effect is mixed both for unimodal and multimodal comparisons.
Improvement of force control The direction of effect is in the direction of the visual modality in unimodal comparisons, and the direction is mixed in the multimodal comparisons.
Improvement of suturing performance The direction of effect is in the direction of the modality other than visual in the unimodal comparisons, and the direction is mixed in the multimodal comparisons.
Level of evidence
Overall, the level of evidence is low due to the predominant use of a study design (cross-over) with a lower level of evidence than RCTs and a predominant high risk of bias.
Discussion
This review examined how delivery modality influences the effect of force feedback on surgical suturing skills. In other words, what are the benefits and constraints of different force feedback modalities (e.g., visual and tactile) on suturing performance and learning? A limited number of studies (n = 9) with a relatively high risk of bias and low level of evidence were included in the review. The results of synthesis suggests that the visual modality could be more beneficial than the tactile and auditory modalities in improving force control and that auditory and tactile modalities could be more beneficial than the visual modality in improving suturing performance. Results are mixed and unclear with regards to how modality affects the reduction of force magnitude. Results show mixed and unclear effects across all the outcomes considered when unimodal (e.g., visual and tactile) was compared with multimodal (e.g., visual plus tactile) force feedback. Similarly, in the knot-tying task, the visual modality could be more beneficial than the other modalities in improving force control, and auditory and tactile modalities could be more beneficial than the visual modality in improving performance. Results across the other tasks and outcomes were mixed and unclear. These results were synthesized combining participants with different levels of expertise (e.g., novices and experts), as the design and analysis of the included studies did not allow to separate the effects according to skill level.
Considerable resources are increasingly invested in developing and refining interventions for training medical student’s surgical skills and for assisting surgeons’ performance in the operating room [41]. Force feedback is widely recognized as a key component of such interventions [1, 2]. Quite surprisingly, this review showed that a low number of studies with low methodological quality examined how force feedback modality influences learning and performance of surgical suturing skill. This can have two main underlying reasons: the feedback modality has no relevant effect on skill development or its potential effect is not known in this specific medical field. Considering that research in psychology and neuroscience indicates that different feedback modalities (e.g., visual and tactile) influence motor skills differently [15] with distinct neural pathways [20], we consider the second explanation to be the most plausible. In support of this, we can observe on a meta-level that the effect direction is mixed due to a diversity of study design with confounding variables—and not due to mixed, unclear direction in each study. This might suggest that indeed modality influences force feedback effectiveness (e.g., there was an overall trend for the visual modality to improve force control and visual and tactile modalities for improving task performance), but the studies’ low methodological quality and low level of evidence prevent us from drawing any meaningful conclusion. As such, rather than speculating on potential feedback modality effect using the weak collected evidence, we discuss how relevant would it be to properly conduct research on this issue. Starting from the limitations of the included studies, we provide a guideline for future research regarding this topic.
Impediments in previous studies and suggestions for future research
The studies included in this review present several limitations. Previous studies were often poorly designed from a methodological perspective. The sample size and consequently statistical power were low. None of the studies used a power analysis to inform the required sample size for testing the anticipated modality effect. Randomization of conditions was poorly conducted and reported, with potential order effect and unbalance across conditions. The plan for data analysis and the actual data analysis was poorly reported, e.g., it was not clear whether all outcome measures were analyzed in all participants. These are the main methodological limitations that future research should address and improve.
On a theoretical level, the influence and collaboration of learning psychology and neuroscience were either not noticeable or at least not discussed. The main limitation was the lack of a principled approach underlying the design and comparison of feedback modalities. Predominantly, feedback modalities were selected on convenience and technical considerations, as if modality effect could generalize to all tasks, contexts, and individuals. We suggest future research to consider these critical aspects of feedback design.
A study should define the goal of a feedback strategy, i.e., promoting students’ skill learning or assisting surgeons’ skill performance in the operating room. In the former, feedback dependency could represent an issue and feedback modality should be selected accordingly. Feedback dependency occurs when a learner regulates their movement on the feedback information—not on intrinsic information—and performance improvement vanishes when feedback is removed [42]. This clearly interferes with learning. On the other hand, feedback dependency is less of an issue in a strategy for assisting surgeons’ performance. If a feedback strategy is always present in the operating room, a surgeon can rely on this augmented information to regulate their movement. Feedback modality can then be designed accordingly. Previous research in motor learning has shown that the auditory modality is generally more beneficial for learning (reduced feedback dependency) and the visual modality for performance [19, 43]. Future research should examine whether this trend occurs also in surgical suturing skill. Furthermore, another promising research avenue—rarely investigated, but highly relevant for suturing skill—is the influence of tactile modality on feedback dependency. A good starting point for researching this issue is knowing the distinction between performance and learning [16, 17].
Another important aspect related to the goal of a feedback strategy is the context in which feedback is implemented or the context toward which a trained skill is intended to transfer. A feedback strategy should be designed considering the characteristics of the target task and environment. For example, visual and tactile modalities may be preferable to an auditory modality for assisting surgeons in laparoscopic surgery whereby environmental noise would prevent the perception of acoustic feedback. On the other hand, auditory feedback may be suitable for assisting surgeons in robotic-assisted surgery in a non-noisy, quite environment. Furthermore, future research should systematically examine how skill level interacts with feedback modality. The studies included in this review did recruit participants with different levels of expertise, but in a confused, non-systematic manner (e.g., different samples and inappropriate data analysis). It was also not stated the rationale for recruiting different skill levels and the impact their level may have on feedback modality effect. Previous research indicates that this is a highly relevant factor and warrants a more thoughtful approach [18, 19]. For example, a criticality for feedback effectiveness is a performer’s mapping of the provided feedback onto their movement, i.e., knowing what the feedback means and how to change movement accordingly. Novices tend to prefer the tactile or visual modality, while experts seem to benefit more from the auditory modality [15]. Another critical aspect to consider is the complexity of the task and movement involved in performing such task and the related complexity of information to provide to a learner/performer (for a detailed overview of this issue see [44, 45]). Tasks and movement with large degrees of freedom (e.g., knot tying) requires feedback that somewhat covers those degrees of freedom and the modality(ies) can play a significant role here. A combination of modalities may be used to provide different information or a single modality may be designed to cover different aspects of a movement. Lastly, the included studies did not control for feedback content as confounding factor [45]. Descriptive and prescriptive feedback have a differential effect on skill. The visual modality can be either descriptive or prescriptive, while auditory and tactile are primarily prescriptive. Auditory and tactile are provided in reference to a threshold (to activate or to smooth). The study design should keep feedback content consistent across modalities for a proper evaluation of modality effect.
This review presents some limitations worth mentioning. Studies were required to be published in English to be included, which may have excluded studies published in other languages. Further, evidence was synthesized using vote counting based on direction of effect, which is a valid method but less precise than a meta-analysis.
In summary, the studies included in this review presented a series of methodological and theoretical limitations, from a motor skill learning perspective. We have provided suggestions for overcoming these limitations. It is crucial for future research to consider the multifactorial interaction of feedback modality with a learner, task, and context. We encourage researchers to consider our suggestions and delineate a detailed plan when investigating the effect of feedback modality on surgical skill. Furthermore, researchers should specify which conditions (goal, context, and skill level) an observed effect can be generalized to. If these issues are not addressed, a study, at best, can be a proof of concept, without providing meaningful results on skill learning and performance. We acknowledge that the technical elements for a feedback modality strategy are complex and require technical expertise (engineers in various fields), but we also emphasize the necessity of including in the research team researchers with expertise in study design and human factors (learning psychology and neuroscience). In this context, an interdisciplinary team is highly recommended [46].
Conclusion
Augmenting force feedback is a key issue in surgical suturing skill, especially in non-open surgery (laparoscopy, robotics assisted, and teleoperation) whereby naturally occurring feedback is impoverished. Different modalities of providing force feedback exist, with potentially different effects on skill learning and performance. This review identified nine studies that examined this issue, comparing different modalities. The low number of studies with low methodological quality and low level of evidence (most were proof of concept) prevent us from drawing any meaningful conclusion and as such it is currently not known whether and how force feedback modality influences surgical suturing skill. We consider the issue of feedback modality to be highly relevant in this field, and we encourage future research to conduct further investigation integrating principles from learning psychology and neuroscience: identify feedback goal, context, and skill level and then design and compare feedback modality accordingly.
References
Panait L, Akkary E, Bell RL, Roberts KE, Dudrick SJ, Duffy AJ (2009) The role of haptic feedback in laparoscopic simulation training. J Surg Res 156:312–316
Zendejas B, Brydges R, Hamstra SJ, Cook DA (2013) State of the evidence on simulation-based training for laparoscopic surgery: a systematic review. Ann Surg 257:586–593
Overtoom EM, Horeman T, Jansen FW, Dankelman J, Schreuder HWR (2019) Haptic feedback, force feedback, and force-sensing in simulation training for laparoscopy: a systematic overview. J Surg Educ 76:242–261
Westebring-van der Putten EP, Goossens RH, Jakimowicz JJ, Dankelman J (2008) Haptics in minimally invasive surgery: a review. Minim Invasive Ther Allied Technol 17:3–16
Alleblas CC, Vleugels MP, Nieboer TE (2016) Ergonomics of laparoscopic graspers and the importance of haptic feedback: the surgeons’ perspective. Gynecol Surg 13:379–384
Horeman T, Rodrigues SP, Jansen F-W, Dankelman J, van den Dobbelsteen JJ (2010) Force measurement platform for training and assessment of laparoscopic skills. Surg Endosc 24:3102–3108
Horeman T, Blikkendaal MD, Feng D, van Dijke A, Jansen F, Dankelman J, van den Dobbelsteen JJ (2014) Visual force feedback improves knot-tying security. J Surg Educ 71:133–141
Horeman T, Rodrigues SP, Willem Jansen F, Dankelman J, van den Dobbelsteen JJ (2012) Force parameters for skills assessment in laparoscopy. IEEE Trans Haptics 5:312–322
Horeman T, Rodrigues SP, Van Den Dobbelsteen JJ, Jansen FW, Dankelman J (2012) Visual force feedback in laparoscopic training. Surg Endosc 26:242–248
Smit D, Spruit E, Dankelman J, Tuijthof G, Hamming J, Horeman T (2017) Improving training of laparoscopic tissue manipulation skills using various visual force feedback types. Surg Endosc 31:299–308
Horeman T, Van Delft F, Blikkendaal MD, Dankelman J, Van Den Dobbelsteen JJ, Jansen FW (2014) Learning from visual force feedback in box trainers: tissue manipulation in laparoscopic surgery. Surg Endosc 28:1961–1970
Amirabdollahian F, Livatino S, Vahedi B, Gudipati R, Sheen P, Gawrie-Mohan S, Vasdev N (2018) Prevalence of haptic feedback in robot-mediated surgery: a systematic review of literature. J Robot Surg 12:11–25
Johansson RS, Westling G (1987) Signals in tactile afferents from the fingers eliciting adaptive motor responses during precision grip. Exp Brain Res 66:141–154
El Rassi I, El Rassi JM (2020) A review of haptic feedback in tele-operated robotic surgery. J Med Eng Technol 44:247–254
Sigrist R, Rauter G, Riener R, Wolf P (2013) Augmented visual, auditory, haptic, and multimodal feedback in motor learning: a review. Psychon Bull Rev 20:21–53
Wulf G, Shea C, Lewthwaite R (2010) Motor skill learning and performance: a review of influential factors. Med Educ 44:75–84
Oppici L, Bobbe T, Lüneburg L, Nocke A, Schwendicke A, Winger H, Krzywinski J, Cherif C, Strufe T, Narciss S (2021) Internet of skills. In: Fitzek FHP, Li S, Speidel S, Strufe T, Simsek M, Reisslein M (eds) Tactile internet with human-in-the-loop. Academic Press, Cambridge, pp 75–99
Sigrist R, Rauter G, Riener R, Wolf P (2013) Terminal feedback outperforms concurrent visual, auditory, and haptic feedback in learning a complex rowing-type task. J Mot Behav 45:455–472
Oppici L, Grütters K, Garofolini A, Rosenkranz R, Narciss S (2021) Deliberate practice and motor learning principles to underpin the design of training interventions for improving lifting movement in the occupational sector: a perspective and a pilot study on the role of augmented feedback. Front Sports Act Living 3:746142
Ronsse R, Puttemans V, Coxon JP, Goble DJ, Wagemans J, Wenderoth N, Swinnen SP (2011) Motor learning with augmented feedback: modality-dependent behavioral and neural consequences. Cereb Cortex 21:1283–1294
Dyer JF, Stapleton P, Rodger M (2017) Mapping sonification for perception and action in motor skill learning. Front Neurosci 11:463
Calvert GA, Spence C, Stein BE (2004) The handbook of multisensory processes. MIT Press, Cambridge
Ferreira JF, Castelo-Branco M, Dias J (2012) A hierarchical Bayesian framework for multimodal active perception. Adapt Behav 20:172–190
Rangarajan K, Davis H, Pucher PH (2020) Systematic review of virtual haptics in surgical simulation: a valid educational tool? J Surg Educ 77:337–347
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Garritty C, Gartlehner G, Nussbaumer-Streit B, King VJ, Hamel C, Kamel C, Affengruber L, Stevens A (2021) Cochrane rapid reviews methods group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol 130:13–22
Higgins JPT, Savović J, Page MJ, Elbers RG, Sterne JAC (2020) Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) Cochrane handbook for systematic reviews of interventions. Wiley, Cochrane
McKenzie JE, Brennan SE (2020) Chapter 12: Synthesizing and presenting findings using other methods. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) Cochrane handbook for systematic reviews of interventions. Wiley, Cochrane
Thomson HJ, Thomas S (2013) The effect direction plot: visual display of non-standardised effects across multiple outcome domains. Res Synth Methods 4:95–101
Boon MH, Thomson H (2021) The effect direction plot revisited: application of the 2019 Cochrane handbook guidance on alternative synthesis methods. Res Synth Methods 12:29–33
Moore DS, McCabe GP (2002) Introduction to the practice of statistics. W. H. Freeman, New York
Al Fayyadh MJ, Hassan RA, Tran ZK, Kempenich JW, Bunegin L, Dent DL, Willis RE (2017) Immediate auditory feedback is superior to other types of feedback for basic surgical skills acquisition. J Surg Educ 74:e55–e61
Currie ME, Talasaz A, Rayman R, Chu MWA, Kiaii B, Peters T, Trejos AL, Patel R (2017) The role of visual and direct force feedback in robotics-assisted mitral valve annuloplasty. Int J Med Robot 13:e1787
Howard T, Szewczyk J (2016) Assisting control of forces in laparoscopy using tactile and visual sensory substitution. In: Wenger P, Chevallereau C, Pisla D, Bleuler H, Rodić A (eds) New trends in medical and service robots. Springer, Cham, pp 151–164
Kitagawa M, Dokko D, Okamura AM, Yuh DD (2005) Effect of sensory substitution on suture-manipulation forces for robotic surgical systems. J Thorac Cardiovasc Surg 129:151–158
Mikic M, Francis P, Looi T, Gerstle JT, Drake J (2019) Bone conduction headphones for force feedback in robotic surgery. Annu Int Conf IEEE Eng Med Biol Soc 2019:7128–7133
Talasaz A, Trejos AL, Patel RV (2012) Effect of force feedback on performance of robotics-assisted suturing. In: 4th IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics, pp 823–828
Talasaz A, Trejos AL, Patel RV (2017) The role of direct and visual force feedback in suturing using a 7-DOF dual-arm teleoperated system. IEEE Trans Haptics 10:276–287
Tavakoli M, Patel RV, Moallem M (2005) Haptic feedback and sensory substitution during telemanipulated suturing. In: First joint eurohaptics conference and symposium on haptic interfaces for virtual environment and teleoperator systems. World Haptics Conference, pp 543–544.
Tavakoli M, Patel RV, Moallem M (2005) Robotic suturing forces in the presence of haptic feedback and sensory substitution. In: Proceedings of 2005 IEEE conference on control applications. pp 1–6
Fritz T, Stachel N, Braun BJ (2019) Evidence in surgical training: a review. Innov Surg Sci 4:7–13
Salmoni AW, Schmidt RA, Walter CB (1984) Knowledge of results and motor learning: a review and critical reappraisal. Psychol Bull 95:355–386
Ghai S, Schmitz G, Hwang TH, Effenberg AO (2019) Training proprioception with sound: effects of real-time auditory feedback on intermodal learning. Ann N Y Acad Sci 1438:50–61
Fowler CA, Turvey MT (1978) Skill acquisition: an event approach with special reference to searching for the optimum of a function of several variables. In: Stelmach GE (ed) Information processing in motor control and learning. Academic Press, Cambridge, pp 1–40
Oppici L, Dix A, Narciss S (2021) When is knowledge of performance (KP) superior to knowledge of results (KR) in promoting motor skill learning? A systematic review. Int Rev Sport Exerc Psychol. https://doi.org/10.1080/1750984X.2021.1986849
Fitzek FHP, Li S, Speidel S, Strufe T, Simsek M, Reisslein M (2021) Tactile internet with human-in-the-loop. Academic Press, Cambridge
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was funded by the German Research Foundation (DFG, Deutsche Forschungsgemeinschaft) as part of Germany’s Excellence Strategy—EXC 2050/1—Project ID 390696704—Cluster of Excellence “Center for Tactile Internet with Human-in-the-Loop” (CeTI) of Technische Universität Dresden. The funding source had no involvement in this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Luca Oppici, Kim Grütters, Felix Bechtolsheim, and Stefanie Speidel have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oppici, L., Grütters, K., Bechtolsheim, F. et al. How does the modality of delivering force feedback influence the performance and learning of surgical suturing skills? We don’t know, but we better find out! A review. Surg Endosc 37, 2439–2452 (2023). https://doi.org/10.1007/s00464-022-09740-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09740-7