Abstract
Background
Concomitant gallstones and common bile duct stones (CBDS) is a relatively frequent presentation. The optimal treatment remains controversial and the debate persists between two strategies. The one-stage approach: laparoscopic cholecystectomy with laparoscopic common bile duct exploration (LCBDE) has been shown to be equally safe and more cost-effective than the more traditional two-stage approach: endoscopic retrograde cholangiography followed by laparoscopic cholecystectomy (ERCP + LC). However, many surgeons worldwide still prefer the two-stage procedure. This survey evaluated contemporary management of CBDS in Spain and assessed the impact of surgeon and hospital factors on provision of LCBDE.
Methods
A 25-item, web-based anonymous survey was sent to general surgeons members of the Spanish Surgeons Association. Descriptive statistics were applied to summarize results.
Results
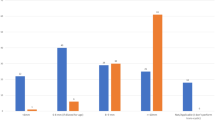
Responses from 305 surgeons across 173 Spanish hospitals were analyzed. ERCP is the initial approach for preoperatively suspected CBDS for 86% of surgeons. LCBDE is the preferred method for only 11% of surgeons and only 11% treat more than 10 cases per year. For CBDS discovered intraoperatively, 59% of respondents attempt extraction while 32% defer to a postoperative ERCP. The main reasons cited for not performing LCBDE were lack of equipment, training and timely availability of an ERCP proceduralist. Despite these barriers, most surgeons (84%) responded that LCBDE should be implemented in their departments.
Conclusions
ERCP was the preferred approach for CBDS for the majority of respondents. There remains limited use of LCBDE despite many surgeons indicating it should be implemented. Focused planning and resourcing of both training and operational demands are required to facilitate adoption of LCBDE as option for patients.

Similar content being viewed by others
References
Lammert F, Gurusamy K, Ko CW, Miquel JF, Méndez-Sánchez N, Portincasa P, Van Erpecum KJ, Van Laarhoven CJ, Wang DQH (2016) Gallstones. Nat Rev Dis Prim 2:16024. https://doi.org/10.1038/nrdp.2016.24
Everhart JE, Khare M, Hill M, Maurer KR (1999) Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology 117:632–639. https://doi.org/10.1016/s0016-5085(99)70456-7
Reshetnyak VI (2012) Concept of the pathogenesis and treatment of cholelithiasis. World J Hepatol 4:18–34. https://doi.org/10.4254/wjh.v4.i2.18
Shabanzadeh DM (2018) Incidence of gallstone disease and complications. Curr Opin Gastroenterol 34:81–89. https://doi.org/10.1097/MOG.0000000000000418
Ireland A, Fitzgerald E, Collins C, O’Sullivan GC, Maguire D (2003) A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy. Ann Surg 239:28–33. https://doi.org/10.1097/01.sla.0000103069.00170.9c
Cuschieri A, Lezoche E, Morino M, Croce E, Lacy A, Toouli J, Faggioni A, Ribeiro VM, Jakimowicz J, Visa J, Hanna GB (1999) E.A.E.S. multicenter prospective randomized trial comparing two-stage vs single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc 13:952–957. https://doi.org/10.1007/s004649901145
Jorba Martín R, Ramirez Maldonado E, Fabregat Prous J, Buisac González D, Banqué Navarro M, Gornals Soler J, Busquets Barenys J, Ramos Rubio E, Peláez Serra N, Lladó Garriga L, Rafecas Renau A (2012) Minimising hospital costs in the treatment of bile duct calculi: a comparison study. Cir Esp 90:310–317. https://doi.org/10.1016/j.ciresp.2012.02.003
Alexakis N, Connor S (2012) Meta-analysis of one- vs. two-stage laparoscopic/endoscopic management of common bile duct stones. HPB (Oxford) 14:254–259. https://doi.org/10.1111/j.1477-2574.2012.00439.x
Prasson P, Bai X, Zhang Q, Liang T (2016) One-stage laproendoscopic procedure versus two-stage procedure in the management for gallstone disease and biliary duct calculi: a systemic review and meta-analysis. Surg Endosc 30:3582–3590. https://doi.org/10.1007/s00464-015-4657-0
Clayton ESJ, Connor S, Alexakis N, Leandros E (2006) Meta-analysis of endoscopy and surgery versus surgery alone for common bile duct stones with the gallbladder in situ. Br J Surg 93:1185–1191. https://doi.org/10.1002/bjs.5568
Liu J, Wang Y, Shu G, Lou C, Zhang J, Du Z (2014) Laparoscopic versus endoscopic management of choledocholithiasis in patients undergoing laparoscopic cholecystectomy: a meta-analysis. J Laparoendosc Adv Surg Tech A 24:287–294. https://doi.org/10.1089/lap.2013.0546
Al-Temimi MH, Kim EG, Chandrasekaran B, Franz V, Trujillo CN, Mousa A, Tessier DJ, Johna SD, Santos DA (2017) Laparoscopic common bile duct exploration versus endoscopic retrograde cholangiopancreatography for choledocholithiasis found at time of laparoscopic cholecystectomy: analysis of a large integrated health care system database. Am J Surg 214:1075–1079. https://doi.org/10.1016/j.amjsurg.2017.08.030
Zhu H-Y, Xu M, Shen H-J, Yang C, Li F, Li K-W, Shi W-J, Ji F (2015) A meta-analysis of single-stage versus two-stage management for concomitant gallstones and common bile duct stones. Clin Res Hepatol Gastroenterol 39:584–593. https://doi.org/10.1016/j.clinre.2015.02.002
Pan L, Chen M, Ji L, Zheng L, Yan P, Fang J, Zhang B, Cai X (2018) The Safety and efficacy of laparoscopic common bile duct exploration combined with cholecystectomy for the management of cholecysto-choledocholithiasis: an up-to-date meta-analysis. Ann Surg 268:247–253. https://doi.org/10.1097/SLA.0000000000002731
Parra-Membrives P, Martínez-Baena D, Lorente-Herce JM, Jiménez-Vega J (2014) Laparoscopic common bile duct exploration in elderly patients: is there still a difference? Surg Laparosc Endosc Percutan Tech 24:e118–e122. https://doi.org/10.1097/SLE.0b013e31829012f6
Lee A, Min SK, Park JJ, Lee HK (2011) Laparoscopic common bile duct exploration for elderly patients: as a first treatment strategy for common bile duct stones. J Korean Surg Soc 81:128–133. https://doi.org/10.4174/jkss.2011.81.2.128
Wu X, Huang Z-J, Zhong J-Y, Ran Y-H, Ma M-L, Zhang H-W (2019) Laparoscopic common bile duct exploration with primary closure is safe for management of choledocholithiasis in elderly patients. Hepatobiliary Pancreat Dis Int 18:557–561. https://doi.org/10.1016/j.hbpd.2019.07.005
National Institute for Health and Care Excellence (2014) Gallstone disease: diagnosis and management - Clinical Guideline. https://www.nice.org.uk/guidance/cg188. Accessed 9 Mar 2020
Tazuma S, Kanno K, Kubota K, Tsuyuguchi T, Kamisawa T, Isayama H, Nakagohri T, Inui K, Academic Committee of the Japan Biliary Association (2015) Report on the 2013 national cholelithiasis survey in Japan. J Hepatobiliary Pancreat Sci 22:392–5. https://doi.org/10.1002/jhbp.206
Vannijvel M, Lesurtel M, Bouckaert W, Houben B, Knol J, Vangertruyden G, Sergeant G (2016) A survey of European-African surgeons’ management of common bile duct stones. HPB (Oxford) 18:959–964. https://doi.org/10.1016/j.hpb.2016.10.007
Dias MM, Martin CJ, Cox MR (2002) Pattern of management of common bile duct stones in the laparoscopic era: a NSW survey. ANZ J Surg 72:181–185. https://doi.org/10.1046/j.1445-2197.2002.02349.x
Bingener J, Schwesinger WH (2006) Management of common bile duct stones in a rural area of the United States: results of a survey. Surg Endosc Other Interv Tech 20:577–579. https://doi.org/10.1007/s00464-005-0322-3
Ministerio de Sanidad Consumo y Bienestar Social (2019) Catálogo Nacional de Hospitales 2019. https://www.mscbs.gob.es/ciudadanos/prestaciones/centrosServiciosSNS/hospitales/docs/CNH_2019.pdf. Accessed 9 Mar 2020
Costi R, Gnocchi A, Di Mario F, Sarli L (2014) Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy. World J Gastroenterol 20:13382–13401. https://doi.org/10.3748/wjg.v20.i37.13382
Baucom RB, Feurer ID, Shelton JS, Kummerow K, Holzman MD, Poulose BK (2016) Surgeons, ERCP, and laparoscopic common bile duct exploration: do we need a standard approach for common bile duct stones? Surg Endosc 30:414–423. https://doi.org/10.1007/s00464-015-4273-z
Gilsdorf D, Henrichsen J, Liljestrand K, Staheli A, Olsen G, Narayanan P, Ott M, Morris DS, Price R (2018) Laparoscopic common bile duct exploration for choledocholithiasis: analysis of practice patterns of Intermountain HealthCare. J Am Coll Surg 226:1160–1165. https://doi.org/10.1016/j.jamcollsurg.2018.02.008
Schwab B, Teitelbaum EN, Barsuk JH, Soper NJ, Hungness ES (2018) Single-stage laparoscopic management of choledocholithiasis: an analysis after implementation of a mastery learning resident curriculum. Surgery 163:503–508. https://doi.org/10.1016/j.surg.2017.10.006
Lu J, Cheng Y, Xiong X-Z, Lin Y-X, Wu S-J, Cheng N-S (2012) Two-stage vs single-stage management for concomitant gallstones and common bile duct stones. World J Gastroenterol 18:3156–3166. https://doi.org/10.3748/wjg.v18.i24.3156
Rogers SJ, Cello JP, Horn JK, Siperstein AE, Schecter WP, Campbell AR, Mackersie RC, Rodas A, Kreuwel HTC, Harris HW (2010) Prospective randomized trial of LC+LCBDE vs ERCP/S+LC for common bile duct stone disease. Arch Surg 145:28–33. https://doi.org/10.1001/archsurg.2009.226
Poh BR, Ho SPS, Sritharan M, Yeong CC, Swan MP, Devonshire DA, Cashin PA, Croagh DG (2016) Randomized clinical trial of intraoperative endoscopic retrograde cholangiopancreatography versus laparoscopic bile duct exploration in patients with choledocholithiasis. Br J Surg 103:1117–1124. https://doi.org/10.1002/bjs.10207
Bansal VK, Misra MC, Rajan K, Kilambi R, Kumar S, Krishna A, Kumar A, Pandav CS, Subramaniam R, Arora MK, Garg PK (2014) Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with concomitant gallbladder stones and common bile duct stones: a randomized controlled trial. Surg Endosc 28:875–885. https://doi.org/10.1007/s00464-013-3237-4
Dasari BVM, Tan CJ, Gurusamy KS, Martin DJ, Kirk G, Mckie L, Diamond T, Taylor MA (2013) Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD003327.pub4
Rhodes M, Sussman L, Cohen L, Lewis MP (1998) Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet (London, England) 351:159–161. https://doi.org/10.1016/s0140-6736(97)09175-7
Costamagna G, Tringali A, Shah SK, Mutignani M, Zuccalà G, Perri V (2002) Long-term follow-up of patients after endoscopic sphincterotomy for choledocholithiasis, and risk factors for recurrence. Endoscopy 34:273–279. https://doi.org/10.1055/s-2002-23632
Tranter SE, Thompson MH (2002) Comparison of endoscopic sphincterotomy and laparoscopic exploration of the common bile duct. Br J Surg 89:1495–1504. https://doi.org/10.1046/j.1365-2168.2002.02291.x
Topal B, Fieuws S, Tomczyk K, Aerts R, Van Steenbergen W, Verslype C, Penninckx F (2009) Clinical models are inaccurate in predicting bile duct stones in situ for patients with gallbladder. Surg Endosc 23:38–44. https://doi.org/10.1007/s00464-008-9868-1
Tanaka M, Takahata S, Konomi H, Matsunaga H, Yokohata K, Takeda T, Utsunomiya N, Ikeda S (1998) Long-term consequence of endoscopic sphincterotomy for bile duct stones. Gastrointest Endosc 48:465–469. https://doi.org/10.1016/S0016-5107(98)70086-0
Tranter SE, Thompson MH (2003) Spontaneous passage of bile duct stones: frequency of occurrence and relation to clinical presentation. Ann R Coll Surg Engl 85:174–177. https://doi.org/10.1308/003588403321661325
Nzenza TC, Al-Habbal Y, Guerra GR, Manolas S, Yong T, McQuillan T (2018) Recurrent common bile duct stones as a late complication of endoscopic sphincterotomy. BMC Gastroenterol 18:39. https://doi.org/10.1186/s12876-018-0765-3
Somasekar K, Chan DSY, Sreekumar NS, Anwer S (2018) Choledocholithiasis after bariatric surgery-more than a stone’s throw to reach? J Gastrointest Surg 22:529–537. https://doi.org/10.1007/s11605-017-3634-4
Cai J, S W, Li W, Chen C, Wen N (2013) A Meta Analysis on Curative Effects of LC+LCBDE Versus EST+LC for the Treatment of Secondary Common Bile Duct Stone. In: Med. J. Wuhan Univ. https://en.cnki.com.cn/Article_en/CJFDTOTAL-HBYK201301025.htm. Accessed 12 Mar 2020
Khan MA, Khan Z, Tombazzi CR, Gadiparthi C, Lee W, Wilcox CM (2018) Role of cholecystectomy after endoscopic sphincterotomy in the management of choledocholithiasis in high-risk patients: a systematic review and meta-analysis. J Clin Gastroenterol 52:579–589. https://doi.org/10.1097/MCG.0000000000001076
Singh AN, Kilambi R (2018) Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with gallbladder stones with common bile duct stones: systematic review and meta-analysis of randomized trials with trial sequential analysis. Surg Endosc 32:3763–3776. https://doi.org/10.1007/s00464-018-6170-8
Buxbaum JL, Abbas Fehmi SM, Sultan S, Fishman DS, Qumseya BJ, Cortessis VK, Schilperoort H, Kysh L, Matsuoka L, Yachimski P, Agrawal D, Gurudu SR, Jamil LH, Jue TL, Khashab MA, Law JK, Lee JK, Naveed M, Sawhney MS, Thosani N, Yang J, Wani SB (2019) ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc 89:1075–1105.e15. https://doi.org/10.1016/j.gie.2018.10.001
Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R, Webster G, Young T (2017) Updated guideline on the management of common bile duct stones (CBDS). Gut 66:765–782
Jorba R, Moreno Sanz C, Robles R (2015) Tratamiento de la Coledocolitiasis asociada a Colelitiasis en España. Resultados de una Encuesta Nacional. In: Cirugía Española - National Meeting of AEC. p 93(Espec Congr):108
Horwood J, Akbar F, Davis K, Morgan R (2010) Prospective evaluation of a selective approach to cholangiography for suspected common bile duct stones. Ann R Coll Surg Engl 92:206–210. https://doi.org/10.1308/003588410X12628812458293
Platt T, Smith K, Nixon M, Sinha S, Srinivas G, Andrews S (2018) Success of intraoperative imaging and management of suspected choledocholithiasis without pre-operative bile duct imaging—a case series. Ann Med Surg 36:173–177. https://doi.org/10.1016/j.amsu.2018.10.036
Ford JA, Soop M, Du J, Loveday BPT, Rodgers M (2012) Systematic review of intraoperative cholangiography in cholecystectomy. Br J Surg 99:160–167. https://doi.org/10.1002/bjs.7809
Pierce RA, Jonnalagadda S, Spitler JA, Tessier DJ, Liaw JM, Lall SC, Melman LM, Frisella MM, Todt LM, Brunt LM, Halpin VJ, Eagon JC, Edmundowicz SA, Matthews BD (2008) Incidence of residual choledocholithiasis detected by intraoperative cholangiography at the time of laparoscopic cholecystectomy in patients having undergone preoperative ERCP. Surg Endosc 22:2365–2372. https://doi.org/10.1007/s00464-008-9785-3
Dili A, Bertrand C (2017) Laparoscopic ultrasonography as an alternative to intraoperative cholangiography during laparoscopic cholecystectomy. World J Gastroenterol 23:5438–5450. https://doi.org/10.3748/wjg.v23.i29.5438
Reinders JSK, Gouma DJ, Ubbink DT, Van Ramshorst B, Boerma D (2014) Transcystic or transductal stone extraction during single-stage treatment of choledochocystolithiasis: a systematic review. World J Surg 38:2403–2411. https://doi.org/10.1007/s00268-014-2537-8
Navarro-Sánchez A, Ashrafian H, Segura-Sampedro JJ, Martrinez-Isla A (2017) LABEL procedure: Laser-Assisted Bile duct Exploration by Laparoendoscopy for choledocholithiasis: improving surgical outcomes and reducing technical failure. Surg Endosc 31:2103–2108. https://doi.org/10.1007/s00464-016-5206-1
Gurusamy KS, Koti R, Davidson BR (2013) T-tube drainage versus primary closure after open common bile duct exploration. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD005640.pub3
Gurusamy KS, Samraj K (2007) Primary closure versus T-tube drainage after open common bile duct exploration. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD005640.pub2
Stephens TJ, Bamber JR, Beckingham IJ, Duncan E, Quiney NF, Abercrombie JF, Martin G, Chole-QuIC collaborator group (2019) Understanding the influences on successful quality improvement in emergency general surgery: learning from the RCS Chole-QuIC Project. Implement Sci 14(1):84. https://doi.org/10.1186/s13012-019-0932-0
Statistical Portal Management Intelligence Area. Government of Spain. Ministry of health, consumption and social welfare. https://pestadistico.inteligenciadegestion.mscbs.es.
Memba R, González S, Coronado D, González V, Mata F, Rodríguez JA, Mühlenberg C, Sala J, Ribas R, Pueyo E, Mata A, O'Connor DB, Conlon KC, Jorba R (2019) Single-stage approach for the management of choledocolithiasis with concomitant cholelithiasis. Implementation of a protocol in a secondary hospital. Surgeon 17(6):351–359
Acknowledgements
The authors would like to express our deep gratitude to all the doctors who responded to the survey. Collaborators: Asociación Española de Cirujanos AEC.
Funding
The resources and the facilities available at the Department of Surgery, University Hospital of Tarragona Joan XXIII were used to conduct this study. No additional funding source was used.
Author information
Authors and Affiliations
Contributions
RJ and RM performed the survey and wrote the paper; MP, EDP-Z and EL contributed to the conception and design of the study, acquisition of data, analysis and interpretation of data. EN, JMB, LE, EJ, MA and DBO’ contributed to critical revision of the manuscript. All authors have participated in drafting the article or revising it critically for important intellectual content and all authors have given final approval of this version to be published.
Corresponding author
Ethics declarations
Disclosures
Jorba R, Pavel M, Llàcer E, Padilla-Zegarra ED, Nve E, Badia JM, Estalella L, Julià E, Achalandabaso M, O’Connor DB and Memba R have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jorba, R., Pavel, M.C., Llàcer-Millán, E. et al. Contemporary management of concomitant gallstones and common bile duct stones: a survey of Spanish surgeons. Surg Endosc 35, 5024–5033 (2021). https://doi.org/10.1007/s00464-020-07984-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07984-9