Abstract
Background
Bariatric surgery on patients with body mass index (BMI) ≥ 50 kg/m2, historically known as superobesity, is technically challenging and carries a higher risk of complications. Bridging interventions have been introduced for weight loss before bariatric surgery in this population. This systematic review and meta-analysis aims to assess the efficacy and safety of bridging interventions before bariatric surgery in patients with BMI ≥ 50 kg/m2.
Methods
MEDLINE, EMBASE, Web of Science, and Scopus were searched from database inception to September 2018. Studies were eligible for inclusion if they conducted any bridging intervention for weight loss in patients with BMI greater than 50 kg/m2 prior to bariatric surgery. Primary outcome was the change in BMI before and after bridging intervention. Secondary outcomes included comorbidity status after bridging interventions and resulting complications. Pooled mean differences (MD) were calculated using random effects meta-analysis.
Results
13 studies including 550 patients met inclusion criteria (mean baseline BMI of 61.26 kg/m2). Bridging interventions included first-step laparoscopic sleeve gastrectomy (LSG), intragastric balloon (IGB), and liquid low-calorie diet program (LLCD). There was a reduction of BMI by 12.8 kg/m2 after a bridging intervention (MD 12.8, 95% CI 9.49–16.1, P < 0.0001). Specifically, LSG demonstrated a BMI reduction of 15.2 kg/m2 (95% CI 12.9–17.5, P < 0.0001) and preoperative LLCD by 9.8 kg/m2 (95% CI 9.82–15.4, P = 0.0006). IGB did not demonstrate significant weight loss prior to bariatric surgery. There was remission or improvement of type 2 diabetes, hypertension, and sleep apnea in 62.8%, 74.6%, and 74.6% of patients, respectively.
Conclusions
First-step LSG and LLCD are both safe and appropriate bridging interventions which can allow for effective weight loss prior to bariatric surgery in patients with BMI greater than 50 kg/m2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The global population’s mean body mass index (BMI) has been increasing steadily since 1980 [1]. Between 2000 and 2005, the prevalence of patients with BMI ≥ 50 kg/m2, historically known as superobesity, increased by 75% within the United States [2]. Along with this trend, the incidence of bariatric procedures within North America has been steeply rising for decades [3,4,5]. Within the cohort of patients with BMI ≥ 50.0–59.9 kg/m2 and BMI ≥ 60 kg/m2 (super-superobesity) who elect for bariatric surgery, there exists an increased rate of complications compared to patients with a lower BMI [6, 7]. It has been speculated that this is a result of the greater technical challenge associated with surgery in the presence of increased liver size, visceral fat, and thicker abdominal wall [8]. Furthermore, conventional bariatric procedures have been demonstrated to be significantly less effective for patients with BMI ≥ 50 kg/m2 [9,10,11]. This represents a serious concern for the patients and surgeons undertaking such procedures. As a result, various bridging options and two-step operations have been developed to make complex malabsorptive bariatric procedures less technically challenging [8].
Currently, there are several bridging and two-step procedures being utilized to ensure the success of bariatric procedures [6, 12,13,14,15,16,17,18,19,20,21,22]. These include preoperative intragastric balloon (IGB) insertion [12,13,14], liquid low-calorie diets (LLCD) [15, 16], first-step restrictive bariatric procedures such as laparoscopic sleeve gastrectomy (LSG), or medical therapies (e.g., liraglutide, naltrexone) prior to malabsorptive surgery [17,18,19,20,21,22]. This initial step can vary widely between surgeons’ and institutions’ preferences with no clear consensus regarding the best option. Although evidence suggests bridging programs make the following bariatric surgery less technically challenging, particularly through a reduction in liver volume [23,24,25], there is a lack of evidence comparing the effects of various bridging therapies. Furthermore, there is a lack of knowledge regarding the long-term effectiveness of bariatric surgery with and without the use of bridging. Considering the current gaps within the literature, it is difficult to make generalizable clinical recommendations regarding an ideal first step for patients with BMI ≥ 50 kg/m2.
Based on the increasing number of patients with BMI ≥ 50 kg/m2, a synthesis of available evidence on bridging interventions before bariatric surgery is warranted. Our objective is to comprehensively review and meta-analyze the current literature regarding bridging interventions used for patients with BMI ≥ 50 kg/m2 prior to their final bariatric procedure.
Methods
Search strategy
We searched the following databases covering the period from database inception through September 2018: MEDLINE, EMBASE, Web of Science, and Scopus. Search strategy included keywords such as “superobesity,” “super-superobesity,” “bariatric surgery,” “BMI > 50,” and similar phrases (complete search strategy is available on Online Appendix 1). We also searched the references of published studies and searched gray literature manually to ensure that relevant articles were not missed. We did not discriminate full texts by language. This systematic review and meta-analysis was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Outcomes
The primary outcome was preoperative BMI loss from the bridging intervention. Secondary outcomes included (1) complications related to the bridging intervention and (2) resolution or improvement of obesity-related comorbidities such as diabetes, hypertension, and obstructive sleep apnea (OSA).
Eligibility criteria and data abstraction
Articles were eligible for inclusion if they implemented any intervention (e.g., including first-step bariatric surgery) to reduce preoperative weight prior to receiving bariatric surgery in patients with superobesity. Historically, superobesity was defined as a baseline BMI ≥ 50 kg/m2 and super–super obesity as a BMI ≥ 60 kg/m2. Exclusion criteria were (1) patients with a BMI < 50 kg/m2, (2) patients who did not receive any preoperative weight loss intervention before bariatric surgery, (3) case-series/reports, expert opinions, basic science, and review articles, and (4) studies including less than 5 patients.
Two reviewers independently screened the searched titles, abstracts, and full texts following inclusion and exclusion criteria. Discrepancies that occurred at the title and abstract screening stages were resolved by automatic inclusion to ensure that all relevant papers were not missed. Discrepancies at the full-text stage were resolved by consensus between two reviewers and if disagreement persisted, a third reviewer was consulted. Two reviewers independently conducted data abstraction onto a standardized spreadsheet designed a priori. The following data were abstracted from included studies: study characteristics (author, country, year of publication, study design, follow-up time), patient demographics (pre-bridging intervention BMI, post-bridging intervention BMI, post-bariatric surgery BMI), bridging procedure characteristics (type, procedure time, complications), and outcomes. Disagreement between reviewers was resolved by a consensus or by a third reviewer.
Risk of bias assessment
Methodological Index for Non-Randomized Studies (MINORS) tool was used to assess the risk of bias for individual studies included in the study [26].
Statistical analysis
All meta-analysis performed was conducted using the DerSimonian and Laird random effects model for continuous variables. The level of significance was set at P < 0.05. Pooled effect estimates were obtained by calculating the mean difference (MD) in outcomes along with their respective 95% confidence intervals (CI) to confirm the effect size estimation. Studies that did not report mean and standard deviations (SD) were estimated using reported median and interquartile ranges through Wan et al’s estimation method [27]. Moreover, when original data only provided the mean, we used the largest standard deviation (SD) in the group of studies in the analysis [28]. Assessment of heterogeneity was completed using the inconsistency (I2) statistic. I2 value greater than 50% was considered to have a high degree of heterogeneity. Subgroup analysis was conducted based on the type of bridging interventions. All statistical analysis and meta-analysis were performed on Cochrane’s Review Manager 5.3 software (London, United Kingdom).
Results
Study characteristics
From 5832 potentially relevant citations identified, a total of 13 studies were included (6 prospective cohorts, 7 retrospective cohorts) representing a total of 550 patients (Fig. 1). All studies were non-comparative in design. Bridging interventions included first-step LSG (9 studies, total n = 453), IGB (2 studies, total n = 62), and LLCD programs (2 studies, total n = 35). Preoperative LLCD programs consisted of a < 800–900 kcal/day diet until bariatric surgery. The exact duration of preoperative LLCD that patients were on before surgery was not specified in either of the studies. Insertion of IGB consisted of inflation of the balloon with saline and methylene blue to 600 ml with removal in approximately 5 months [13] or removal no sooner than 6 months [14]. The studies included had homogenous indications for bridging interventions, which included BMI > 50.0–59.9 kg/m2 or BMI > 60 kg/m2. Included studies were conducted between 2003 and 2018 with a median follow-up period of 12 months (range 6 months to 84 months) across all outcome measurements. When a study reported more than one follow-up time point, we chose to analyze the time point closest to 12 months. The weighted mean age of the patients at the time of surgery was 46.3 years. The weighted mean BMI at baseline was 61.3 kg/m2 and 47.5 kg/m2 after bridging intervention, with a mean percentage total weight loss of 22.4% after the bridging intervention. The weighted mean BMI after bariatric surgery was 39.0 kg/m2, with mean absolute percent reduction of 36.4% from baseline to bariatric surgery. Bariatric procedures conducted after the bridging intervention included Roux-en-Y gastric bypass (RYGB (7 studies), LSG (1 study), and biliopancreatic diversion and duodenal switch (BPD-DS; 5 studies). The characteristics of included studies in this systematic review are reported in detail in Table 1.
Primary outcome
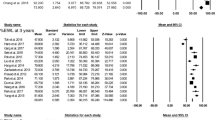
All studies reported mean BMI before and after bridging. Pooled change in mean BMI demonstrated a significant reduction by 12.8 kg/m2 after the bridging intervention (95% CI 9.49 to 16.1, P < 0.0001) (Fig. 2). Subgroup analysis by the type of bridging intervention demonstrated a significant change in BMI in patients who underwent first-step LSG (MD 15.2 kg/m2, 95% CI 12.9 to 17.5, P < 0.0001) or preoperative LLCD (MD 9.8 kg/m2, 95% CI 9.82 to 15.4, P = 0.0006). Insertion of IGB did not demonstrate any significant change in BMI (MD 10.8, 95% CI − 1.5 to 23.1, P = 0.08).
To examine whether bridging therapy allowed for successful weight loss after bariatric surgery, we conducted a meta-analysis of mean BMI after bridging therapy and BMI after bariatric surgery. There was a significant decrease in BMI by 6.71 kg/m2 (95% CI 1.22 to 12.2, P = 0.02) after bariatric surgery (Fig. 3). Heterogeneity was high across all outcomes (range of I2 from 52% to 99%).
Secondary outcomes
Comorbidities such as diabetes, hypertension, and OSA were reported in the included studies. In studies that reported comorbidity prevalence, remission, or improvement of diabetes occurred in 62.8% (48/62) of patients, 74.6% (50/67) with hypertension, and 80.0% (28/35) with OSA after bridging intervention alone (Table 3).
There were complications associated with bridging interventions. Patients who received LSG (n = 396) had complications such as leakage (n = 5; 1.3%), bleeding (n = 10; 2.5%), conversion to laparotomy (n = 3; 0.8%), pulmonary embolism (n = 2; 0.5%), fistula (n = 1; 0.3%), splenic injury (n = 1; 0.3%), incisional hernia (n = 1; 0.3%), and death (n = 2; 0.5%). In patients who received IGB (n = 62) two complications were reported, those being an unplanned intensive care unit (ICU) admission (n = 1; 1.6%) and conversion to laparotomy (n = 1; 1.6%). There were no complications reported for LLCD (n = 35) (Table 2). In total, patients that received LSG, IGB, and LLCD as a bridging intervention had 6.3%, 3.2%, and 0% rates of complications, respectively (Table 3).
Risk of bias
The mean MINORS score of included studies was 12.7 (SD 0.85), which indicates a fair quality of evidence for non-randomized studies [26]. A comprehensive list of MINORS for included studies is available in Table 2. In brief, all 13 studies had a clearly stated objective with unbiased assessment of study endpoint. Most of the studies included consecutive patients (12/13 studies) with prospective collection of data (10/13), had an established protocol prior to the study (11/13 studies), and had less than 5 to 10% of loss to follow-up (6/13 studies). The mean follow-up was longer than 12 months in 10/13 studies. However, most studies lacked a prospective calculation of study size (2/13 studies) and none of the studies had blinding of their outcome assessments (Table 4).
Discussion
This systematic review and meta-analysis demonstrated that bridging interventions such as first-step LSG and preoperative LLCD resulted in a significant reduction (P < 0.0001) of BMI prior to bariatric surgery for patients with BMI greater or equal to 50. However, IGB has no significant effect in reducing preoperative BMI. After these bridging interventions, planned bariatric surgery also results in a significant decrease in BMI after surgery. Moreover, our review also reveals that bridging interventions alone are helpful in remission or improvement of obesity-related comorbidities such as diabetes, hypertension, and OSA.
To our knowledge, this is the first meta-analysis to explore the effectiveness and safety of bridging interventions for patients with BMI ≥ 50 kg/m2. Although none of the included studies directly compared the outcomes between bridging interventions, there are several studies in the literature that investigated these interventions as a primary procedure for weight loss. In a retrospective study comparing LSG versus IGB on patients with BMI ≥ 50 kg/m2, LSG resulted in significantly greater weight loss as well as lower complication rate than IGB after 6 months [29]. Hence, this study supports our review’s finding of LSG being a useful first-step bridging intervention for patients with BMI ≥ 50 kg/m2. In a study by Coffin et al., patients with BMI greater than 45 kg/m2 were randomized to IGB insertion as a bridging intervention versus standard medical care prior to RYGB [30], which revealed that IGB resulted in a significantly higher weight loss than standard medical care after 6 months. Similarly, in a meta-analysis of by Moura et al., the effectiveness of IGB was compared to a sham/diet in an overweight population [31]. They found that there was a small, but statistically significant BMI decrease in the IGB group compared to the sham/diet group [31]. These studies could not be included in our review due to a lower BMI cut-off, but the result from this study contradicts the present review which determined no statistically significant reduction in BMI from IGB. However, this could be due to the fact that the study population did not consist of patients with BMI ≥ 50 kg/m2, for which IGB may be less effective to achieve weight loss [31]. In a systematic review and meta-analysis by Brethauer et al., they found that LSG is a safe and effective intervention when used as the first stage to a more complex bariatric procedure and also found that LSG resulted in an improvement or remission of type 2 diabetes in 70% of cases, along with significant improvements in hypertension and OSA [32]. Overall, the work of Brethauer et al. serves to reinforce the present review’s determination that bridging interventions such as first-step LSG can be an effective tool in the treatment of patients with BMI ≥ 50 kg/m2.
Currently, there are no specific guidelines or recommendations on preoperative planning and management of patients with BMI ≥ 50 kg/m2 who are undergoing bariatric surgery. Therefore, the present study provides an overview of which bridging interventions could be utilized to ensure good surgical outcomes in patients with BMI ≥ 50 kg/m2. Patients with BMI ≥ 50 kg/m2 often have larger liver volume, intraperitoneal fat, or increased intra-abdominal pressure which makes laparoscopic bariatric procedures technically challenging. Depending on the surgeon or the volume of the center, patients with BMI ≥ 50 kg/m2 are sometimes considered to be non-surgical candidates. In a multicenter randomized study by Van Nieuwenhowe et al., prescribing a 14-day very low-calorie diet regimen before RYGB leads to a significantly lower perceived difficulty of the procedure as well as postoperative complication rates than the control group in patients with obesity [33]. Therefore, a reduction of BMI using bridging interventions would help mitigate these intraoperative barriers and make bariatric surgery less difficult in patients with BMI ≥ 50 kg/m2. Moreover, long-term weight regain or failure to achieve primary weight loss goals is prevalent in patients with BMI ≥ 50 kg/m2 [34,35,36]. Therefore, using LSG as a first-step surgery or giving patients LLCD prior to malabsorptive bariatric surgery may lead to better weight loss outcomes. Increased BMI has been associated with a greater number of complications (wound infection, sepsis, pneumonia, pulmonary embolism, etc.) preceding bariatric surgery [37]. Decreasing patient BMI prior to bariatric procedures can decrease surgical complications for patients with BMI ≥ 50 kg/m2. Moreover, patients with BMI ≥ 50 kg/m2 suffer comorbidities such as type 2 diabetes, OSA, hypertension, and hyperlipidemia to a greater degree than patients with obesity [38]. The findings of this review demonstrate that bridging interventions such as LSG and LLCD alone can resolve or improve these comorbidities prior to receiving the intended bariatric surgery. However, despite its effectiveness, some patients may be hesitant to pursue more than one surgery. Furthermore, patients may be deterrent of the cost and compliance of preoperative LLCD as an average 12-week LLCD programs can range from $108 USD to $2120 USD [39]. Therefore, first-step LSG is a surgical option or preoperative LLCD is a medical bridging option that clinicians could discuss with patients with BMI ≥ 50 kg/m2 when choosing for a bridging intervention prior to undergoing definitive bariatric surgery.
Our review findings should be interpreted in light of the following limitations. Firstly, our review had very few patients undergoing bridging with IGB or LLCD, meaning the results may be underpowered in the analysis. Third, due to this study including both BMI ≥ 50.0–59.9 kg/m2 (superobesity) and BMI ≥ 60 kg/m2 (super-superobesity), there was a wide range of variability in the initial BMI of patients (range of 54.0 kg/m2 to 69.3 kg/m2). Furthermore, the two IGB studies in this review included BMI ≥ 60 kg/m2 populations only, and thus we cannot predict what the effectiveness of IGB would be specific to patients with BMI ≥ 50.0–59.9 kg/m2. Fourth, high heterogeneity was present for the IGB and LLCD analysis. This can be attributed to the varying initial BMI, differences in study design, and different bridging interventions used between trials. Finally, the present review only examines each bridging intervention individually as there are no studies in the current literature comparing one bridging intervention to another. As a result, no direct comparison or conclusions can be made regarding which bridging intervention would be the most effective for patients with BMI ≥ 50 kg/m2. Future research studies could examine the effect of more than one bridging interventions (e.g., prescribing preoperative LLCD along with first-step LSG) for patients with BMI ≥ 50 kg/m2. Furthermore, upcoming research may examine the use of novel bridging interventions, such as medical therapies, prior to bariatric surgery in patients with BMI ≥ 50 kg/m2. Currently, the use of substances such as liraglutide and naltrexone have been used proceeding bariatric surgery to induce additional weight loss, but it may be an area of interest to investigate its role in preoperative weight loss before bariatric surgery [40].
Conclusion
First-step LSG or preoperative LLCD are both safe and efficacious bridging intervention prior to bariatric surgery in patients with BMI ≥ 50 kg/m2. However, there are no comparative studies to suggest which intervention is superior. Our review also suggests that IGB was ineffective for preoperative weight loss in patients with BMI ≥ 60 kg/m2. Future comparative studies or adequately powered randomized controlled trials are warranted to identify which bridging interventions may be most beneficial in patients with BMI ≥ 50 kg/m2.
Abbreviations
- BMI:
-
Body mass index
- LSG:
-
Laparoscopic sleeve gastrectomy
- IGB:
-
Intragastric balloon
- LLCD:
-
Liquid low-calorie diets
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- MINORS:
-
Methodological index for non-randomized studies
- MD:
-
Mean difference
- CI:
-
Confidence intervals
- I2 :
-
Inconsistency
- RYGB:
-
Roux-en-Y gastric bypass
- BPD-DS:
-
Biliopancreatic diversion and duodenal switch
- OSA:
-
Obstructive sleep apnea
- ICU:
-
Intensive care unit
- RCT:
-
Randomized controlled trial
- EWL:
-
Excess weight loss
References
Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN, Farzadfar F, Riley LM, Ezzati M, Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index) (2011) National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet 377:557–567. https://doi.org/10.1016/s0140-6736(10)62037-5
Sturm R (2007) Increases in morbid obesity in the USA: 2000-2005. Public Health 121:492–496. https://doi.org/10.1016/j.puhe.2007.01.006
Canadian Institute for Health Information (2014) Bariatric surgery in Canada. Canadian Institute for Health Information, Ottawa
American Society for Metabolic and Bariatric Surgery (2018) Estimate of bariatric surgery numbers, 2011–2017. American Society for Metabolic and Bariatric Surgery, Gainesville
Ponce J, DeMaria EJ, Nguyen NT, Hutter M, Sudan R, Morton JM (2016) American Society for Metabolic and Bariatric Surgery estimation of bariatric surgery procedures in 2015 and surgeon workforce in the United States. Surg Obes Relat Dis 12:1637–1639. https://doi.org/10.1016/j.soard.2016.08.488
Tarnoff M, Kaplan LM, Shikora S (2008) An evidenced-based assessment of preoperative weight loss in bariatric surgery. Obes Surg 18(9):1059–1061. https://doi.org/10.1007/s11695-008-9603-y
Schwartz ML, Drew RL, Chazin-Caldie M (2004) Factors determining conversion from laparoscopic to open Roux-en-Y gastric bypass. Obes Surg 14:1193–1197. https://doi.org/10.1381/0960892042386887
Lim RB, Blackburn GL, Jones DB (2010) Benchmarking best practices in weight loss surgery. Curr Probl Surg 47:79–174. https://doi.org/10.1067/j.cpsurg.2009.11.003
Skrekas G, Lapatsanis D, Stafyla V, Papalambros A (2008) One year after laparoscopic “Tight” sleeve gastrectomy: technique and outcome. Obes Surg 18:810–813. https://doi.org/10.1007/s11695-008-9440-z
Magro DO, Geloneze B, Delfini R, Pareja BC, Callejas F, Pareja JC (2008) Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg 18:648–651. https://doi.org/10.1007/s11695-007-9265-1
Inge TH, Jenkins TM, Zeller M, Dolan L, Daniels SR, Garcia VF, Brandt ML, Bean J, Gamm K, Xanthakos SA (2010) Baseline BMI is a strong predictor of nadir BMI after adolescent gastric bypass. J Pediatr 156:103–108. https://doi.org/10.1016/j.jpeds.2009.07.028
Busetto L, Segato G, De Luca M, Bortolozzi E, MacCari T, Magon A, Inelmen EM, Favretti F, Enzi G (2004) Preoperative weight loss by intragastric balloon in super-obese patientstreated with laparoscopic gastric banding: a case-control study. Obes Surg 14:671–676. https://doi.org/10.1381/096089204323093471
Zerrweck C, Maunoury V, Caiazzo R, Branche J, Dezfoulian G, Bulois P, Verkindt H, Pigeyre M, Arnalsteen L, Pattou F (2012) Preoperative weight loss with intragastric balloon decreases the risk of significant adverse outcomes of laparoscopic gastric bypass in super-super obese patients. Obes Surg 22:777–782. https://doi.org/10.1007/s11695-011-0571-2
Khan O, Irukulla S, Sanmugalingam N, Vasilikostas G, Reddy M, Wan A (2013) Simultaneous intra-gastric balloon removal and laparoscopic sleeve gastrectomy for the super-super obese patients—a prospective feasibility study. Obes Surg 23:585–587. https://doi.org/10.1007/s11695-013-0871-9
Huerta S, Li Z, Anthony T, Livingston EH (2010) Feasibility of a Supervised inpatient low-calorie diet program for massive weight loss prior to RYGB in superobese patients. Obes Surg 20:173–180. https://doi.org/10.1007/s11695-009-0001-x
Collins J, McCloskey C, Titchner R, Goodpaster B, Hoffman M, Hauser D, Wilson M, Eid G (2011) Preoperative weight loss in high-risk superobese bariatric patients: a computed tomography-based analysis. Surg Obes Relat Dis 7:480–485. https://doi.org/10.1016/j.soard.2010.09.026
Regan JP, Inabnet WB, Gagner M, Pomp A (2003) Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese patient. Obes Surg 13:861–864. https://doi.org/10.1381/096089203322618669
Silecchia G, Rizzello M, Casella G, Fioriti M, Soricelli E, Basso N (2009) Two-stage laparoscopic biliopancreatic diversion with duodenal switch as treatment of high-risk super-obese patients: analysis of complications. Surg Endosc 23:1032–1037. https://doi.org/10.1007/s00464-008-0113-8
Silecchia G, Boru C, Pecchia A, Rizzello M, Casella G, Leonetti F, Basso N (2006) Effectiveness of laparoscopic sleeve gastrectomy (first stage of biliopancreatic diversion with duodenal switch) on co-morbidities in super-obese high-risk patients. Obes Surg 16:1138–1144. https://doi.org/10.1381/096089206778392275
Iannelli A, Schneck AS, Dahman M, Negri C, Gugenheim J (2009) Two-step laparoscopic duodenal switch for superobesity: a feasibility study. Surg Endosc 23:2385–2389. https://doi.org/10.1007/s00464-009-0363-0
Dapri G, Cadière GB, Himpens J (2011) Superobese and super-superobese patients: 2-step laparoscopic duodenal switch. Surg Obes Relat Dis 7:703–708. https://doi.org/10.1016/j.soard.2011.09.007
Alexandrou A, Felekouras E, Giannopoulos A, Tsigris C, Diamantis T (2012) What is the actual fate of super-morbid-obese patients who undergo laparoscopic sleeve gastrectomy as the first step of a two-stage weight-reduction operative strategy? Obes Surg 22:1623–1628. https://doi.org/10.1007/s11695-012-0718-9
Lewis M, Phillips M, Slavotinek J, Kow L, Thompson C, Toouli J (2006) Change in liver size and fat content after treatment with optifast < SUP > ®</SUP > very low calorie diet. Obes Surg 16:697–701. https://doi.org/10.1381/096089206777346682
Fris RJ (2004) Preoperative Low energy diet diminishes liver size. Obes Surg 14:1165–1170. https://doi.org/10.1381/0960892042386977
Frutos MD, Morales MD, Luján J, Hernández Q, Valero G, Parrilla P (2007) Intragastric balloon reduces liver volume in super-obese patients, facilitating subsequent laparoscopic gastric bypass. Obes Surg 17:150–154. https://doi.org/10.1007/s11695-007-9040-3
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
Higgins J, Green S (2011) 16.1.3.1 Imputing standard deviations. In: Cochrane Handb. Syst. Rev. Interv. https://handbook-5-1.cochrane.org/chapter_16/16_1_3_1imputing_standard_deviations.htm. Accessed 2 Feb 2019
Milone L, Strong V, Gagner M (2005) Laparoscopic sleeve gastrectomy is superior to endoscopic intragastric balloon as a first stage procedure for super-obese patients (BMI ≥ 50). Obes Surg 15:612–617. https://doi.org/10.1381/0960892053923833
Coffin B, Maunoury V, Pattou F, Hébuterne X, Schneider S, Coupaye M, Ledoux S, Iglicki F, Huten N, Alfaiate T, Hajage D, Msika S (2017) Impact of intragastric balloon before laparoscopic gastric bypass on patients with super obesity: a randomized multicenter study. Obes Surg 27(4):902–909. https://doi.org/10.1007/s11695-016-2383-x
Moura D, Oliveira J, De Moura EGH, Bernardo W, Neto MG, Campos J, Popov VB, Thompson C (2016) Effectiveness of intragastric balloon for obesity: a systematic review and meta-analysis based on randomized control trials. Surg Obes Relat Dis 12(2):420–429. https://doi.org/10.1016/j.soard.2015.10.077
Brethauer SA, Hammel JP, Schauer PR (2009) Systematic review of sleeve gastrectomy as staging and primary bariatric procedure. SOARD 5:469–475. https://doi.org/10.1016/j.soard.2009.05.011
Van Nieuwenhove Y, Dambrauskas Z, Campillo-Soto A, van Dielen F, Wiezer R, Janssen I, Kramer M, Thorell A (2011) Preoperative very low-calorie diet and operative outcome after laparoscopic gastric bypass. Arch Surg 146:1300. https://doi.org/10.1001/archsurg.2011.273
Arterburn DE, Courcoulas AP (2014) Bariatric surgery for obesity and metabolic conditions in adults. BMJ 349:g3961. https://doi.org/10.1136/BMJ.G3961
Nelson DW, Blair KS, Martin MJ (2012) Analysis of obesity-related outcomes and bariatric failure rates with the duodenal switch vs gastric bypass for morbid obesity. Arch Surg 147:847. https://doi.org/10.1001/archsurg.2012.1654
Lee Y, Ellenbogen Y, Doumouras AG, Gmora S, Anvari M, Hong D (2019) Single- or double-anastomosis duodenal switch versus Roux-en-Y gastric bypass as a revisional procedure for sleeve gastrectomy: a systematic review and meta-analysis. Surg Obes Relat Dis 1:2. https://doi.org/10.1016/j.soard.2019.01.022
Turner PL, Saager L, Dalton J, Abd-Elsayed A, Roberman D, Melara P, Kurz A, Turan A (2011) A nomogram for predicting surgical complications in bariatric surgery patients. Obes Surg 21:655–662. https://doi.org/10.1007/s11695-010-0325-6
Hariri K, Guevara D, Dong M, Kini SU, Herron DM, Fernandez-Ranvier G (2018) Is bariatric surgery effective for co-morbidity resolution in the super-obese patients? Surg Obes Relat Dis 14:1261–1268. https://doi.org/10.1016/j.soard.2018.05.015
Spielman AB, Kanders B, Kienholz M, Blackburn GL (1992) The cost of losing: an analysis of commercial weight-loss programs in a metropolitan area. J Am Coll Nutr 11:36–41. https://doi.org/10.1080/07315724.1992.10718194
Creange C, Lin E, Ren-Fielding C, Lofton H (2016) Use of liraglutide for weight loss in patients with prior bariatric surgery. Surg Obes Relat Dis 12:S157. https://doi.org/10.1016/j.soard.2016.08.281
Acknowledgements
We thank Dr. Chunhong Tian for assistance with the literature search strategy development. We thank Dr. Ben Vandermeer for confirming our statistical method and study design.
Funding
No external funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Yung Lee, Jerry Dang, Noah Switzer, Roshan Malhan, Daniel Birch, and Shahzeer Karmali have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, Y., Dang, J.T., Switzer, N. et al. Bridging interventions before bariatric surgery in patients with BMI ≥ 50 kg/m2: a systematic review and meta-analysis. Surg Endosc 33, 3578–3588 (2019). https://doi.org/10.1007/s00464-019-07027-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07027-y