Abstract
Background
Surgical site infection (SSI) prevention bundles include the simultaneous use of different measures, which individually have demonstrated an effect on prevention of SSI. The implementation of bundles can yield superior results to the implementation of individual measures. The aim of this study was to address the effect of the application of a bundle including intraperitoneal lavage with antibiotic solution, fascial closure with Triclosan-coated sutures and Mupirocin ointment application on the skin staples, on the surgical site infection after elective laparoscopic colorectal cancer surgery.
Methods
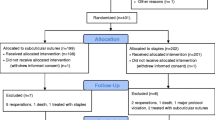
A prospective, randomized study was performed, including patients with diagnosis of colorectal neoplasms and plans to undergo an elective laparoscopic surgery. The patients were randomized into two groups: those patients following standard bundles (Group 1) and those ones following the experimental bundle with three additional measures, added to the standard bundle. Incisional and organ space SSI were investigated. The study was assessor-blinded.
Results
A total of 198 patients were included in the study, 99 in each group. The incisional SSI rate was 16% in Group 1 and 2% in Group 2 [p = 0.007; RR = 5.6; CI 95% (1.4–17.8)]. The organ–space SSI rate was 4% in Group 1 and 0% in Group 2 [p = 0.039; RR = 1.7; CI 95% (1.1–11.6)]. Median hospital stay was 5.5 days in Group 1 and 4 days in Group 2 (p = 0.028).
Conclusions
The addition of intraperitoneal lavage with antibiotic solution, fascial closure with Triclosan-coated sutures and Mupirocin ointment application on the skin staples, to a standard bundle of SSI prevention, reduces the incisional and organ–space SSI and consequently the hospital stay, after elective laparoscopic colorectal cancer surgery (ClinicalTrials.gov Identifier: NCT03081962).

Similar content being viewed by others
References
Weiner LM, Webb AK, Limbago B et al (2016) Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety network at the centers for Disease Control and Prevention, 2011–2014. Infect Control Hosp Epidemiol 31:1288–1301
Itani KMF, Hawn MT (2013) Prevention of surgical site infection in colorectal surgery. Colorectal Cancer 2:467–475
Artinyan A, Orcutt ST, Anaya DA et al (2015) Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer. Ann Surg 261:497–505
Merkow RP, Ju MH, Chung JW et al (2015) Underlying reasons associated with hospital readmission following surgery in the United States. JAMA 313:483–495
Itani KMF (2015) Care bundles and prevention of surgical site infection in colorectal surgery. JAMA 314:289–290
Deierhoi RJ, Dawes LG, Vick C et al (2013) Choice of intravenous antibiotic prophylaxis for colorectal surgery does matter. J Am Coll Surg 217:763–769
Keenan JE, Speicher PJ, Thacker JKM et al (2014) The preventive surgical site infection bundle in colorectal surgery. JAMA Surg 149:1045–1052
Hawn MT, Vick CC, Richman J et al (2011) Surgical site infection prevention. Ann Surg 254:494–499
Tanner J, Kiernan M, Hilliam R et al (2016) Effectiveness of a care bundle to reduce surgical site infections in patients having open colorectal surgery. Ann R Coll Surg Eng 98:270–274
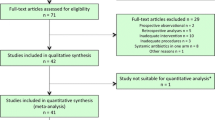
Zywot A, Lau CSM, Fletcher HS et al (2017) Bundles prevent surgical site infections after colorectal surgery: Meta-analysis and systematic review. J Gastrointest Surg. https://doi.org/10.1007/s11605-017-3465-3
Horan TC, Gaynes RP, Martone WJ et al (1992) CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol 13:606–608
Allegranzi B, Zayed B, Bischoff P et al (2016) New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 16:e288–e303
Ban KA, Minei JP, laronga C et al (2017) American College of Surgeons and surgical infection society: surgical site infection guidelines, 2016 update. J Am Coll Surg 224:59–74
Sandini M, Mattavelli I, Nespoli L et al (2016) Systematic review and meta-analysis of sutures coated with Triclosan for the prevention of surgical site infections after elective colorectal surgery according to the PRISMA statement. Medicine 95:35–44
Leaper D, Assadian O, Hubner NO et al (2011) Antimicrobial sutures and prevention of surgical site infection: assessment of the safety of the antiseptic triclosan. Int J Wound 8:556–566
Wang ZX, Jiang CP, Cao Y et al (2013) Systematic review and meta-analysis of Triclosan-coated sutures for the prevention of surgical-site infection. Br J Surg 100:465–473
Henriksen NA, Deerenberg EB, Venclauskas L et al (2017) Triclosan-coated sutures and surgical site infection in abdominal surgery: the TRISTAN review, meta-analysis and trial sequential analysis. Hernia. https://doi.org/10.1007/s10029-017-1681-0
Savage JW, Anderson PA (2013) An update on modifiable factors to reduce the risk of surgical site infections. Spine 13:1017–1029
Hendley JO, Ashe KM (2003) Eradication of resident bacteria of normal human skin by antimicrobial ointment. Antimicrob Agents Chemother 47:1988–1990
McCann M, Moore ZE (2010) Interventions for preventing infectious complications in haemodialysis patients with central venous catheters. Cochrane Database Syst Rev 20:CD006894
Phillips M, Rosenberg A, Shopsin B et al (2014) Preventing surgical site infections: a randomized, open label trial of nasal mupirocin ointment and nasal povidone-iodine solution. Infect Control Hosp Epidemiol 35:826–832
Yang J, Lee D, Kim Y et al (2007) Occurrence of the van genes in Enterococcus faecalis and Enterococcus faecium from clinical isolates in Korea. Arch Pharm Res 30:329–336
Ruiz-Tovar J, Llavero C, Morales V et al (2015) Total occlusive ionic silver-containing dressing vs mupirocin ointment application vs conventional dressing in elective colorectal surgery: effect on incisional surgical site infection. J Am Coll Surg 221:424–429
Platell C, Papadimitriou JM, Hall JC (2000) The influence of lavage on peritonitis. J Am Coll Surg 191:672–680
Adam U, Ledwon D, Hopt UT (1997) Programmed lavage as a basic principle in therapy of diffuse peritonitis. Langenbecks Arch Surg 382:18–21
Hall JC, Heel KA, Papadimitriou J, Platell C (1998) The pathobiology of peritonitis. Gastroenterology 114:185–196
Qadan M, Dajani D, Dickinson A, Polk HC (2010) Meta-analysis of the effect of peritoneal lavage on survival in experimental peritonitis. Br J Surg 97:151–159
Ruiz-Tovar J, Santos J, Arroyo A et al (2012) Effect of peritoneal lavage with clindamycin-gentamicin solution on infections after elective colorectal cancer surgery. J Am Coll Surg 214:202–207
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Jaime Ruiz-Tovar, Carolina Llavero, Vicente Morales, and Carlos Gamallo, have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Ruiz-Tovar, J., Llavero, C., Morales, V. et al. Effect of the application of a bundle of three measures (intraperitoneal lavage with antibiotic solution, fascial closure with Triclosan-coated sutures and Mupirocin ointment application on the skin staples) on the surgical site infection after elective laparoscopic colorectal cancer surgery. Surg Endosc 32, 3495–3501 (2018). https://doi.org/10.1007/s00464-018-6069-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6069-4