Abstract
Background
The aim of this study was to evaluate the benefits of cholecystectomy on mitigating recurrent biliary complications following endoscopic treatment of common bile duct stone.
Methods
We used the data from the Taiwan National Health Insurance Research Database to conduct a population-based cohort study. Among 925 patients who received endoscopic treatment for choledocholithiasis at the first admission from 2005 to 2012, 422 received subsequent cholecystectomy and 503 had gallbladder (GB) left in situ. After propensity score matching with 1:1 ratio, the cumulative incidence of recurrent biliary complication and overall survival was analyzed with Cox’s proportional hazards model. The primary endpoint of this study is recurrent biliary complications, which require intervention.
Results
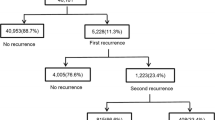
After matching, 378 pairs of patients were identified with a median follow-up time of 53 (1–108) months. The recurrent rate of biliary complications was 8.20% in the cholecystectomy group and 24.87% in the GB in situ group (p < 0.001). In the multivariate Cox regression analysis, the only independent risk factor for recurrent biliary complications was GB left in situ (hazard ratio [HR] 3.55, 95% CI 2.36–5.33).
Conclusions
Cholecystectomy after endoscopic treatment of common bile duct stone reduced the prevalence of recurrent biliary complications.



Similar content being viewed by others
References
Shen HC, Hu YC, Chen YF, Tung TH (2014) Prevalence and associated metabolic factors of gallstone disease in the elderly agricultural and fishing population of taiwan. Gastroenterol Res Pract 2014:876918
Chen CH, Huang MH, Yang JC, Nien CK, Etheredge GD, Yang CC, Yeh YH, Wu HS, Chou DA, Yueh SK (2006) Prevalence and risk factors of gallstone disease in an adult population of Taiwan: an epidemiological survey. J Gastroenterol Hepatol 21:1737–1743
Everhart JE, Khare M, Hill M, Maurer KR (1999) Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology 117:632–639
Tazuma S (2006) Gallstone disease: epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract Res Clin Gastroenterol 20:1075–1083
Classen M, Demling L (1974) Endoscopic sphincterotomy of the papilla of vater and extraction of stones from the choledochal duct (author’s transl). Dtsch Med Wochenschr 99:496–497
Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y (1974) Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc 20:148–151
Boender J, Nix GA, de Ridder MA, Dees J, Schutte HE, van Buuren HR, van Blankenstein M (1995) Endoscopic sphincterotomy and biliary drainage in patients with cholangitis due to common bile duct stones. Am J Gastroenterol 90:233–238
McAlister VC, Davenport E, Renouf E (2007) Cholecystectomy deferral in patients with endoscopic sphincterotomy. Cochrane Database Syst Rev :CD006233
Agresta F, Campanile FC, Vettoretto N, Silecchia G, Bergamini C, Maida P, Lombari P, Narilli P, Marchi D, Carrara A, Esposito MG, Fiume S, Miranda G, Barlera S, Davoli M, Italian Surgical Societies Working G (2015) Laparoscopic cholecystectomy: consensus conference-based guidelines. Langenbecks Arch Surg 400:429–453
Internal Clinical Guidelines T (2014) National Institute for Health and Care Excellence: Clinical Guidelines. Gallstone Disease: Diagnosis and Management of Cholelithiasis, Cholecystitis and Choledocholithiasis. National Institute for Health and Care Excellence, London
Committee ASoP, Maple JT, Ikenberry SO, Anderson MA, Appalaneni V, Decker GA, Early D, Evans JA, Fanelli RD, Fisher D, Fisher L, Fukami N, Hwang JH, Jain R, Jue T, Khan K, Krinsky ML, Malpas P, Ben-Menachem T, Sharaf RN, Dominitz JA (2011) The role of endoscopy in the management of choledocholithiasis. Gastrointest Endosc 74:731–744
Heo J, Jung MK, Cho CM (2015) Should prophylactic cholecystectomy be performed in patients with concomitant gallstones after endoscopic sphincterotomy for bile duct stones? Surg Endosc 29:1574–1579
Lai KH, Lin LF, Lo GH, Cheng JS, Huang RL, Lin CK, Huang JS, Hsu PI, Peng NJ, Ger LP (1999) Does cholecystectomy after endoscopic sphincterotomy prevent the recurrence of biliary complications? Gastrointest Endosc 49:483–487
Boerma D, Rauws EA, Keulemans YC, Janssen IM, Bolwerk CJ, Timmer R, Boerma EJ, Obertop H, Huibregtse K, Gouma DJ (2002) Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: a randomised trial. Lancet 360:761–765
Lau JY, Leow CK, Fung TM, Suen BY, Yu LM, Lai PB, Lam YH, Ng EK, Lau WY, Chung SS, Sung JJ (2006) Cholecystectomy or gallbladder in situ after endoscopic sphincterotomy and bile duct stone removal in Chinese patients. Gastroenterology 130:96–103
Kim MH, Yeo SJ, Jung MK, Cho CM (2016) The impact of gallbladder status on biliary complications after the endoscopic removal of choledocholithiasis. Dig Dis Sci 61:1165–1171
Lai JH, Wang HY, Chang WH, Chu CH, Shih SC, Lin SC (2012) Recurrent cholangitis after endoscopic lithotripsy of common bile duct stones with gallstones in situ: predictive factors with and without subsequent cholecystectomy. J Laparoendosc Adv Surg Tech A 22:324–329
Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M, British Society of G (2008) Guidelines on the management of common bile duct stones (CBDS). Gut 57:1004–1021
(2014) National Health Insurance Administration, Ministry of Health and Welfare, Taiwan, R.O.C. National Health Insurance Annual Report
King G, Ho D, Stuart EA, Imai K (2011) MatchIt: nonparametric preprocessing for parametric causal inference
Oak JH, Paik CN, Chung WC, Lee KM, Yang JM (2012) Risk factors for recurrence of symptomatic common bile duct stones after cholecystectomy. Gastroenterol Res Pract 2012:417821
Cui ML, Cho JH, Kim TN (2013) Long-term follow-up study of gallbladder in situ after endoscopic common duct stone removal in Korean patients. Surg Endosc 27:1711–1716
Sugiyama M, Atomi Y (2002) Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol 97:2763–2767
Nakai Y, Isayama H, Tsujino T, Hamada T, Kogure H, Takahara N, Mohri D, Matsubara S, Yamamoto N, Tada M, Koike K (2016) Cholecystectomy after endoscopic papillary balloon dilation for bile duct stones reduced late biliary complications: a propensity score-based cohort analysis. Surg Endosc 30:3014–3020
Steiner CA, Bass EB, Talamini MA, Pitt HA, Steinberg EP (1994) Surgical rates and operative mortality for open and laparoscopic cholecystectomy in Maryland. N Engl J Med 330:403–408
Csikesz N, Ricciardi R, Tseng JF, Shah SA (2008) Current status of surgical management of acute cholecystitis in the United States. World J Surg 32:2230–2236
Giger UF, Michel JM, Opitz I, Th Inderbitzin D, Kocher T, Krahenbuhl L, Swiss Association of L, Thoracoscopic Surgery Study G (2006) Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: analysis of 22,953 consecutive cases from the Swiss Association of Laparoscopic and Thoracoscopic Surgery database. J Am Coll Surg 203:723–728
Kimura Y, Takada T, Strasberg SM, Pitt HA, Gouma DJ, Garden OJ, Buchler MW, Windsor JA, Mayumi T, Yoshida M, Miura F, Higuchi R, Gabata T, Hata J, Gomi H, Dervenis C, Lau WY, Belli G, Kim MH, Hilvano SC, Yamashita Y (2013) TG13 current terminology, etiology, and epidemiology of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 20:8–23
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Chi-Tung Cheng, Chun-Nan Yeh, Kun-Chun Chiang, Ta-Sen Yeh, Kuan-Fu Chen, Shao-Wei Chen have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cheng, CT., Yeh, CN., Chiang, KC. et al. Effects of cholecystectomy on recurrent biliary complications after endoscopic treatment of common bile duct stone: a population-based cohort study. Surg Endosc 32, 1793–1801 (2018). https://doi.org/10.1007/s00464-017-5863-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5863-8