Abstract
Introduction
Nonalcoholic fatty liver disease (NAFLD) is an epidemic in the obese population. Bariatric surgery is known to reverse multiple metabolic complications of obesity such as diabetes, dyslipidemia, and NAFLD, but the timing of liver changes has not been well described.
Materials and Methods
This was an IRB-approved, two-institutional prospective study. Bariatric patients received MRIs at baseline and after a pre-operative liquid diet. Liver biopsies were performed during surgery and if NAFLD positive, the patients received MRIs at 1, 3, and 6 months. Liver volumes and proton-density fat fraction (PDFF) were calculated from offline MRI images. Primary outcomes were changes in weight, body mass index (BMI), percent excess weight loss (EWL%), liver volume, and PDFF. Resolution of steatosis, as defined as PDFF < 6.4% based on previously published cutoffs, was assessed. Secondarily, outcomes were compared between patients who underwent laparoscopic sleeve gastrectomy (LSG) versus laparoscopic Roux-en-Y gastric bypass (LRYGB).
Results
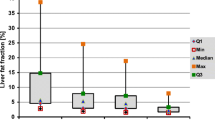
From October 2010 to June 2015, 124 patients were recruited. 49 patients (39.5%) completed all five scans. EWL% at 6 months was 55.6 ± 19.0%. BMI decreased from 45.3 ± 5.9 to 34.4 ± 5.1 kg/m2 and mean liver volume decreased from 2464.6 ± 619.4 to 1874.3 ± 387.8 cm3 with a volume change of 21.4 ± 11.4%. PDFF decreased from 16.6 ± 7.8 to 4.4 ± 3.4%. At 6 months, 83.7% patients had resolution of steatosis. Liver volume plateaued at 1 month, but PDFF and BMI continued to decrease. There were no statistically significant differences in liver volume or PDFF reduction from baseline to 6 months between the LSG versus LRYGB subgroups.
Conclusion
Patients with NAFLD undergoing bariatric surgery can expect significant decreases in liver volume and hepatic steatosis at 6 months, with 83.7% of patients achieving resolution of steatosis. Liver volume reduction plateaus 1-month post-bariatric surgery, but PDFF continues to decrease. LSG and LRYGB did not differ in efficacy for inducing regression of hepatosteatosis.



Similar content being viewed by others
References
Vernon G, Baranova A, Younossi ZM (2011) Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther 34(3):274–285
Loomba R, Sanyal AJ (2013) The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol 10(11):686–690
Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K et al (2012) The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology 55(6):2005–2023
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, Brethauer SA et al (2017) Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med 376(7):641–651
Lassailly G, Caiazzo R, Buob D, Pigeyre M, Verkindt H, Labreuche J et al (2015) Bariatric surgery reduces features of nonalcoholic steatohepatitis in morbidly obese patients. Gastroenterology 149(2):379–388
Noureddin M, Lam J, Peterson MR, Middleton M, Hamilton G, Le TA et al (2013) Utility of magnetic resonance imaging versus histology for quantifying changes in liver fat in nonalcoholic fatty liver disease trials. Hepatology 58(6):1930–1940
Tang A, Tan J, Sun M et al (2013) Nonalcoholic fatty liver disease: MR imaging of liver proton density fat fraction to assess hepatic steatosis. Radiology 267(2):422–431
Tang A, Desai A, Hamilton G, Wolfson T, Gamst A, Lam J et al (2015) Accuracy of MR imaging-estimated proton density fat fraction for classification of dichotomized histologic steatosis grades in nonalcoholic fatty liver disease. Radiology 274(2):416–425
Kang GH, Cruite I, Shiehmorteza M, Wolfson T, Gamst AC, Hamilton G et al (2011) Reproducibility of MRI-determined proton density fat fraction across two different MR scanner platforms. J Magn Reson Imaging 34(4):928–934
Edholm D, Kullberg J, Karlsson FA, Haenni A, Ahlstrom H, Sundbom M (2015) Changes in liver volume and body composition during 4 weeks of low calorie diet before laparoscopic gastric bypass. Surg Obes Relat Dis. 11(3):602–606
González-Pérez J, Sánchez-Leenheer S, Delgado AR, González-Vargas L, Díaz-Zamudio M, Montejo G et al (2013) Clinical impact of a 6-week preoperative very low calorie diet on body weight and liver size in morbidly obese patients. Obes Surg 23(10):1624–1631
Tang A, Chen J, Le TA, Changchien C, Hamilton G, Middleton MS et al (2015) Cross-sectional and longitudinal evaluation of liver volume and total liver fat burden in adults with nonalcoholic steatohepatitis. Abdom Imaging 40(1):26–37
Patel NS, Doycheva I, Peterson MR, Hooker J, Kisselva T, Schnabl B et al (2015) Effect of weight loss on magnetic resonance imaging estimation of liver fat and volume in patients with nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol 13(3):561–568
Johansson L, Roos M, Kullberg J, Weis J, Ahlström H, Sundbom M et al (2008) Lipid mobilization following Roux-en-Y gastric bypass examined by magnetic resonance imaging and spectroscopy. Obes Surg 18(10):1297–1304
Edholm D, Kullberg J, Haenni A, Karlsson FA, Ahlström A, Hedberg J et al (2011) Preoperative 4-week low-calorie diet reduces liver volume and intrahepatic fat, and facilitates laparoscopic gastric bypass in morbidly obese. Obes Surg 21(3):345–350
Iannelli A, Martini F, Schneck AS, Ghavami B, Baudin G, Anty R et al (2013) Preoperative 4-week supplementation with omega-3 polyunsaturated fatty acids reduces liver volume and facilitates bariatric surgery in morbidly obese patients. Obes Surg 23(11):1761–1765
Carlin AM, Zeni TM, English WJ, Hawasli AA, Genaw JA, Krause KR et al (2013) The comparative effectiveness of sleeve gastrectomy, gastric bypass, and adjustable gastric banding procedures for the treatment of morbid obesity. Ann Surg 257(5):791–797
Colquitt JL, Pickett K, Loveman E, Frampton GK (2014) Surgery for weight loss in adults. Cochrane Database Syst Rev 8:CD003641
Froylich D, Corcelles R, Daigle C, Boules M, Brethauer S, Schauer P (2016) Effect of Roux-en-Y gastric bypass and sleeve gastrectomy on nonalcoholic fatty liver disease: a comparative study. Surg Obes Relat Dis 12(1):127–131
Funding
National Institute of Health (NIH) Grants: R01DK088925, R01DK083380, R01DK100651, K24DK102595.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Reeder reports other from Cellectar Biosciences, other from Elucent Medical, other from Calimetrix, LCC, personal fees from Parexel International, outside the submitted work. Dr. Sandler reports personal fees from W.L Gore, personal fees from Bard/Davol, personal fees from ValenTx, Inc. outside the submitted work. Dr. Horgan reports personal fees from Johnson and Johnson/Ethicon, personal fees from W.L. Gore, personal fees from Torax/Ethicon, personal fees from ValenTx, Inc outside the submitted work. Dr. Sirlin reports grants from National Institute of Health, during the conduct of the study; grants from Bayer, grants from Guerbet, grants from Siemens, grants from General Electric, grants from Supersonic, grants from Arterys, personal fees from Alexion, personal fees from AstraZeneca, personal fees from Bioclinica, personal fees from BMS, personal fees from Bracco, personal fees from Celgene, personal fees from Fibrogen, personal fees from Galmed, personal fees from Genentech, personal fees from Genzyme, personal fees from Gilead, personal fees from Icon, personal fees from Intercept, personal fees from Isis, personal fees from Janssen, personal fees from NuSirt, personal fees from Perspectum, personal fees from Pfizer, personal fees from Profil, personal fees from Sanofi, personal fees from Shire, personal fees from Synageva, personal fees from Tobira, personal fees from Takeda, personal fees from Virtual Scopics, outside the submitted work. Dr. Jacobsen reports personal fees from W.L.Gore, personal fees from Davol/Bard, personal fees from Viasite, personal fees from Ethicon, outside the submitted work. Drs. Luo, Suzuki, Liu, Schwimmer, Funk, Greenberg and Campos, Mr. Hooker, Ms. Schlein, and Ms. Covarrubias have no conflicts of interest or financial ties to disclose.
Additional information
Ran B. Luo and Toshiaki Suzuki are co-first authors.
Rights and permissions
About this article
Cite this article
Luo, R.B., Suzuki, T., Hooker, J.C. et al. How bariatric surgery affects liver volume and fat density in NAFLD patients. Surg Endosc 32, 1675–1682 (2018). https://doi.org/10.1007/s00464-017-5846-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5846-9