Abstract
Background
The challenge of performing a good total mesorectal excision (TME) dissection, particularly in the distal 1/3 of the rectum, has spurred interest in new techniques. Robotic surgery is advocated by some, and more recently, a “new” approach, the transanal total mesorectal excision, has been popularized to address this problem. While great interest in this technique exists, little long-term outcome data are available. We have been utilizing a transanal abdominal transanal approach to TME in order to facilitate the distal dissection, and here, we provide our long-term outcomes using this approach in the management of rectal cancer.
Methods
From a prospectively maintained rectal cancer database, we identified 373 consecutive rectal cancers treated with sphincter preservation surgery through a combined transanal and abdominal approach to TME. Perioperative, pathological, and oncologic outcomes were analyzed.
Results
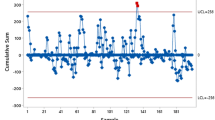
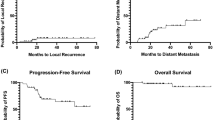
Three hundred and seventy-three patients with rectal cancer underwent a transanally initiated TME with mean follow-up of 5.5 years. 91% of cancers were in the distal rectum. 68.9% were men and 53.2% of cancers were tethered or fixed on presentation. 97.7% received neoadjuvant radiotherapy (mean 5405 cGy, 5-fluorouracil based); average time from completion of neoadjuvant therapy to surgery was 11 weeks. 180 and 193 patients underwent completion of their operation through open and laparoscopic abdominal approaches. 96% of TME specimens were complete/near complete, 94% had a negative circumferential resection margin, and 98.6% had a negative distal margin. Perioperative morbidity and mortality rates were 13.4 and 0.3%. Overall local recurrence (LR), DM, and Kaplan–Meier 5-year actuarial survival were 7.4, 19.5, and 90%, respectively.
Conclusion
This is the first report of long-term data using a transanal approach to TME supporting this approach for rectal cancer. Our data with 5-year follow-up show that adequate distal and circumferential margins with very good-quality TME specimens, and a low risk for LR with excellent overall survival can be achieved using this technique. Our long-term results support the promising reports of early experiences in the literature.

Similar content being viewed by others
References
Miles WE (1924) Discussion on the treatment of carcinoma of the rectum. Proc R Soc Med 17:79
Heald RJ et al (1982) The mesorectum in rectal cancer surgery—the clue to pelvic recurrence? Br J Surg 69:613–616
Heald RJ (1988) The “Holy Plane” of rectal surgery. J R Soc Med 81:503–508
Quirke P, Durdey P, Dixon MF, Williams NS (1986) Local recurrence of rectal adenocarcinoma due to inadequate surgical resection: histopathologic study of lateral tumor spread and surgical excision. Lancet 2:996–999
Hall NR, Finan PJ, al-Jaberi T, Tsang CS, Brown SR, Dixon MF, Quirke P (1998) Circumferential margin involvement after mesorectal excision of rectal cancer with curative intent. Predictor of survival but not local recurrence? Dis Colon Rectum 41:979–983
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M et al (2015) Effect of laparoscopic-assisted resection vs. open resection of stage II or III rectal cancer on pathologic outcomes. The ACOSOG Z6051 randomized clinical trial. JAMA 314(13):1346–1355
Marks GJ, Marks JH, Mohiuddin M, Bradley L (1998) Radical sphincter-preservation surgery with coloanal anastomosis following high dose external irradiation for the very low lying rectal cancer. Recent Results Cancer Res 146:161–174
Marks JH, Valsdottir EB (2015) Total mesorectal excision with coloanal anastomosis: laparoscopic technique. In: Mulholland M (ed) Operative techniques in surgery, vol 2. Lippincott Williams and Wilkins, Philadelphia, pp 1177–1189
Tuech J, Karoui M, Lelong B, Chaisemartin C, Bridoux V et al (2015) A step toward NOTES total mesorectal excision for rectal cancer. Ann Surg 261(2):228–233
Denost Q, Adam J, Rullier A, Buscail E, Laurent C, Rullier E (2014) Perineal transanal approach: a new standard for laparoscopic sphincter-saving resection in low rectal cancer, a randomized trial. Ann Surg 260(6):993–999
Albert MR, Atallah SB, deBeche-Adams TC, Izfar S, Larach W (2013) Transanal minimally invasive surgery (TAMIS) for local excision of benign neoplasms and early-stage rectal cancer: efficacy and outcomes in the first 50 patients. Dis Colon Rectum 56(3):301–307
Atallah S, Albert M, DeBeche-Adams T, Nassif G, Polavarapu H, Larach S (2013) Transanal minimally invasive surgery for total mesorectal excision (TAMIS-TME): a stepwise description of the surgical technique with video demonstration. Tech Coloproctol 17(3):321–325
Wexner SD, Berho M (2014) Transanal TAMIS total mesorectal excision (TME)—a work in progress. Tech Coloproctol 18(5):423–425
Rink AD, Kauff DW, Paschold M, Vestweber KH, Lang H, Kneist W (2016) Hybrid TAMIS total mesorectal excision: a new perspective in treatment of distal rectal cancer—technique and results. Chirurg 87(3):225–232
Knol JJ, D’Hondt M, Souverijns G, Heald B, Vangertruyden G (2015) Transanal endoscopic total mesorectal excision: technical aspects of approaching the mesorectal plane from below—a preliminary report. Tech Coloproctol 19(4):221–229
Aigner F, Hörmann R, Fritsch H, Pratschke J, D’Hoore A, Brenner E, Williams N, Biebl M (2015) Anatomical considerations for transanal minimal-invasive surgery: the caudal to cephalic approach. Colorectal Dis 17(2):47–53
Zorron R, Phillips HN, Wynn G, Neto MP, Coelho D, Vassallo RC (2014) “Down-to-Up” transanal NOTES Total mesorectal excision for rectal cancer: preliminary series of 9 patients. J Minim Access Surg 10(3):144–150
Lacy AM, Tasende MM, Delgado S, Fernandez-Hevia M, Jiminez M et al (2015) Transanal total mesorectal excision for rectal cancer: outcomes after 140 patients. J Am Coll Surg 221(2):415–423
Buess G, Theiss R, Gunther M, Hutterer F, Hepp M, Pichlmaier H (1984) Endoscopic operative procedure for the removal of rectal polyps. Coloproctology 84:254–261
Atallah S (2014) Transanal minimally invasive surgery for total mesorectal excision. Minim Invasive Ther Allied Technol 23(1):10–16
Atallah S, Martin-Perez B, Albert M, deBeche-Adams T, Nassif G, Hunter L, Larach S (2014) Transanal minimally invasive surgery for total mesorectal excision (TAMIS-TME): results and experience with the first 20 patients undergoing curative-intent rectal cancer surgery at a single institution. Tech Coloproctol 18(5):473–480
Marks JH, Nassif G, Schoonyoung H, DeNittis A, Zeger E, Mohiuddin M, Marks GJ (2013) Sphincter-sparing surgery for adenocarcinoma of the distal 3 cm of the true rectum: results after neoadjuvant therapy and minimally invasive radical surgery or local excision. Surg Endosc 27:4469–4477
Quirke P, Steele R, Monson J, MRC CR07/NCIC-CTG CO16 Trial Investigators; NCRI Colorectal Cancer Study Group et al (2009) Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet 373(9666):821–828
Nagtegaal ID, van de Velde CJ, van der Worp E, Kapiteijn E, Quirke P, van Krieken JH (2002) Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. Cooperative Clinical Investigators of the Dutch Colorectal Cancer Group. J Clin Oncol 20(7):1729–1734
Nagtegaal ID, Quirke P (2008) What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol 26(2):303–312
Guillou PJ, Quirke P, Thorpe H et al (2005) Short-term endpoints of convention vs. laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726
Green BL, Marshall HC, Collinson F et al (2013) Long-term follow-up of the Medical Research Council CLASSIC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg 100(1):75–82
Kang SB, Park JW, Jeong SY et al (2010) Open versus laparoscopic surgery for mid to low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 11(7):637–645
Jeong SY, Park JW, Nam BH et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15(7):767–774
Vanderpas MH, Haglind E, Cuesta MA, Colorectal cancer Laparoscopic or Open Resection II (COLOR II) Study Group et al (2013) Laparoscopic vs. open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–212
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, Lacy AM, Bemelman WA, Andersson J, Angenete E, Rosenberg J, Fuerst A, Haglind E (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372(14):1324–1332
Stevenson ARL, Solomon M, Lumley J, Hewett P, Clouston A, Gebski V, Davies L, Wilson K, Hague W, Simes J (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314(13):1356–1363
Marks G, Mohiuddin M, Masoni L, Montori A (1992) High-dose preoperative radiation therapy as the key to extending sphincter preservation surgery for cancer of the distal rectum. Surg Oncol Clin N Am 1:71–85
Marks JH, Lopez-Acevedo N, Krishnan B, Johnson MN, Montenegro GA, Marks GJ (2016) True NOTES TME resection with splenic flexure release, high ligation of IMA, and side-to-end hand-sewn coloanal anastomosis. Surg Endosc 30(10):4626–4631
Marks J, Mizrahi B, Dalane S, Nweze I, Marks G (2010) Laparoscopic transanal abdominal transanal resection with sphincter preservation for rectal cancer in the distal 3 cm of the rectum after neoadjuvant therapy. Surg Endosc 24:2700–2707
Acknowledgements
Supported by Harry Mirabile Colorectal Cancer Fund of the Marks Colorectal Surgical Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
John H. Marks, Elizabeth A. Myers, Erik L. Zeger, Albert S. Denittis, Mounica Gummadi and Gerald J. Marks have no conflicts of interest of financial ties to disclose
Rights and permissions
About this article
Cite this article
Marks, J.H., Myers, E.A., Zeger, E.L. et al. Long-term outcomes by a transanal approach to total mesorectal excision for rectal cancer. Surg Endosc 31, 5248–5257 (2017). https://doi.org/10.1007/s00464-017-5597-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5597-7