Abstract
Background
Laparoscopic organ-sparing pancreatectomy (LOSP) is an ideal therapeutic option in selected cases of pancreatic neuroendocrine tumors (PNETs). Nevertheless, given the low frequency of PNETs, there is scarce evidence regarding short and particularly long-term outcomes of LOSP in this clinical setting.
Methods
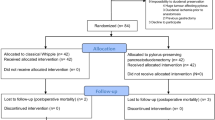
All patients with PNETs who underwent surgery (under a LOSP policy) were retrospectively reviewed from a prospective database maintained at our center. Preoperative characteristics, operative data, pathological features and postoperative outcomes were analyzed.
Results
Between December 2003 and December 2015, 36 patients with PNETs underwent laparoscopic resections. Ten were functional tumors, 26 non-functional and 16 were “incidental” cases. The following procedures were performed: one enucleation, eight central pancreatectomies (LCP), one resection of the uncinate process and 26 distal pancreatectomies (DP) (15 of them laparoscopic vessels-preserving). There were no conversions to open surgery, and no drains were routinely left. Mean operative time was 288 min (SD 99). Hospital stay was 6 days. Eighteen patients (50%) experienced some complication of which most were mild (Clavien–Dindo I/II). Three postoperative bleedings occurred: two grade B/one grade C; two required laparoscopic reoperation. Thirteen (36.1%) patients developed peripancreatic fluid collections: two were symptomatic and were managed with transgastric drainage (one presented post-puncture abscesification requiring surgical drainage and splenectomy). Four patients (11%)—one DP and three LCP—developed new-onset pancreatogenic diabetes mellitus (NODM) in the long term. According to the European Neuroendocrine Tumor Society, 19 cases were stage I, seven IIA, two IIIA, one IIIB and seven stage IV. Over a mean follow-up of 51 months, two patients died, one due to recurrence of the tumor and another due to cirrhosis.
Conclusions
The existing different surgical options must be individually considered according to the location and particular characteristics of every tumor. Results from this single-center study document the effectiveness of LOSP in selected cases of PNETs.

Similar content being viewed by others
Abbreviations
- PNETs:
-
Pancreatic neuroendocrine tumors
- LOSP:
-
Laparoscopic organ-sparing pancreatectomy
- LCP:
-
Laparoscopic central pancreatectomy
- DP:
-
Distal pancreatectomy
- LVPDP:
-
Laparoscopic vessels-preserving distal pancreatectomy
- NODM:
-
New-onset pancreatogenic diabetes mellitus
- LEN:
-
Enucleation
- LDP:
-
Laparoscopic distal pancreatectomy
- WD:
-
Wirsung duct
- LRDPS:
-
Laparoscopic radical distal pancreatosplenectomy
- RAMPS:
-
Radical anterograde modular pancreatosplenectomy
- SD:
-
Standard deviation
- CT:
-
Multislice computer tomography
- MRI:
-
Magnetic resonance imaging
- EUS:
-
Endoscopic ultrasound
- ENETS:
-
European neuroendocrine society
- FNA:
-
Fine-needle aspiration
- BMI:
-
Body mass index
References
Halperin DM, Kulke MH, Yao JC (2015) A tale of two tumors: treating pancreatic and extrapancreatic neuroendocrine tumors. Annu Rev Med 66:1–16. doi:10.1146/annurev-med-061813-012908
Kondo NI, Ikeda Y (2014) Practical management and treatment of pancreatic neuroendocrine tumors. Gland Surg 3:276–283. doi:10.3978/j.issn.2227-684X.2013.12.05
Rindi G, Wiedenmann B (2011) Neuroendocrine neoplasms of the gut and pancreas: new insights. Nat Rev 8:54–64. doi:10.1038/nrendo.2011.120
Reid MD, Balci S, Saka B, Adsay NV (2014) Neuroendocrine tumors of the pancreas: current concepts and controversies. Endocr Pathol 25:65–79. doi:10.1007/s12022-013-9295-2
Liu TC, Hamilton N, Hawkins W, Gao F, Cao D (2013) Comparison of WHO Classifications (2004, 2010), the Hochwald grading system, and AJCC and ENETS staging systems in predicting prognosis in locoregional well-differentiated pancreatic neuroendocrine tumors. Am J Surg Pathol 37:853–859. doi:10.1097/PAS.0b013e31827fcc18
Cherenfant J, Stocker SJ, Gage MK, Du H, Thurow TA, Odeleye M, Schimpke SW, Kaul KL, Hall CR, Lamzabi I, Gattuso P, Winchester DJ, Marsh RW, Roggin KK, Bentrem DJ, Baker MS, Prinz RA, Talamonti MS (2013) Predicting aggressive behavior in nonfunctioning pancreatic neuroendocrine tumors. Surgery 154:783–785. doi:10.1016/j.surg.2013.07.004
Cherenfant J, Talamonti MS, Hall CR, Thurow TA, Gage MK, Stocker SJ, Lapin B, Wang E, Silverstein JC, Mangold K, Odeleye M, Kaul KL, Lamzabi I, Gattuso P, Winchester DJ, Marsh RW, Roggin KK, Bentrem DJ, Baker MS, Prinz RA (2014) Comparison of tumor markers for predicting outcomes after resection of nonfunctioning pancreatic neuroendocrine tumors. Surgery 156:1501–1504. doi:10.1016/j.surg.2014.08.043
Clancy TE (2016) Surgical management of pancreatic neuroendocrine tumors. Hematol Oncol Clin North Am 30:103–118. doi:10.1016/j.hoc.2015.09.004
Mehta SS, Doumane G, Mura T, Nocca D, Fabre JM (2012) Laparoscopic versus open distal pancreatectomy: a single-institution case-control study. Surg Endosc 26:402–407. doi:10.1007/s00464-011-1887-7
Venkat R, Edil BH, Schulick RD, Lidor AO, Makary MA, Wolfgang CL (2012) Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann Surg 255:1048–1059. doi:10.1097/SLA.0b013e318251ee09
Hwang HK, Kang CM, Chung YE, Kim KA, Choi SH, Lee WJ (2013) Robot-assisted spleen-preserving distal pancreatectomy: a single surgeon’s experiences and proposal of clinical application. Surg Endosc 27:774–781. doi:10.1007/s00464-012-2551-6
Klimstra DS, Modlin IR, Adsay NV, Chetty R, Deshpande V, Gonen M, Jensen RT, Kidd M, Kulke MH, Lloyd RV, Moran C, Moss SF, Oberg K, O’Toole D, Rindi G, Robert ME, Suster S, Tang LH, Tzen CY, Washington MK, Wiedenmann B, Yao J (2010) Pathology reporting of neuroendocrine tumors: application of the Delphic consensus process to the development of a minimum pathology data set. Am J Surg Pathol 34:300–313. doi:10.1097/PAS.0b013e3181ce1447
Kloppel G (2011) Classification and pathology of gastroenteropancreatic neuroendocrine neoplasms. Endocr Relat Cancer 18(Suppl 1):S1–S16. doi:10.1530/ERC-11-0013
Kloppel G, Rindi G, Perren A, Komminoth P, Klimstra DS (2010) The ENETS and AJCC/UICC TNM classifications of the neuroendocrine tumors of the gastrointestinal tract and the pancreas: a statement. Virchows Arch 456:595–597. doi:10.1007/s00428-010-0924-6
Gagner M, Pomp A (1994) Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 8:408–410
Abu Hilal M, Hamdan M, Di Fabio F, Pearce NW, Johnson CD (2012) Laparoscopic versus open distal pancreatectomy: a clinical and cost-effectiveness study. Surg Endosc 26:1670–1674. doi:10.1007/s00464-011-2090-6
Fernandez-Cruz L, Cosa R, Blanco L, Levi S, Lopez-Boado MA, Navarro S (2007) Curative laparoscopic resection for pancreatic neoplasms: a critical analysis from a single institution. J Gastrointest Surg 11:1602–1607. doi:10.1007/s11605-007-0266-0
Fox AM, Pitzul K, Bhojani F, Kaplan M, Moulton CA, Wei AC, McGilvray I, Cleary S, Okrainec A (2012) Comparison of outcomes and costs between laparoscopic distal pancreatectomy and open resection at a single center. Surg Endosc 26:1220–1230. doi:10.1007/s00464-011-2061-y
Datta J, Vollmer CM Jr (2016) Advances in surgical management of pancreatic diseases. Gastroenterol Clin North Am 45:129–144. doi:10.1016/j.gtc.2015.10.002
Nakamura M, Wakabayashi G, Miyasaka Y, Tanaka M, Morikawa T, Unno M, Tajima H, Kumamoto Y, Satoi S, Kwon M, Toyama H, Ku Y, Yoshitomi H, Nara S, Shimada K, Yokoyama T, Miyagawa S, Toyama Y, Yanaga K, Fujii T, Kodera Y, JHBPS SG of JSEPS, Tomiyama Y, Miyata H, Takahara T, Beppu T, Yamaue H, Miyazaki M, Takada T (2015) Multicenter comparative study of laparoscopic and open distal pancreatectomy using propensity score-matching. J Hepatobiliary Pancreat Sci. doi:10.1002/jhbp.268
Nakamura M, Nakashima H (2013) Laparoscopic distal pancreatectomy and pancreatoduodenectomy: is it worthwhile? A meta-analysis of laparoscopic pancreatectomy. J Hepatobiliary Pancreat Sci 20:421–428. doi:10.1007/s00534-012-0578-7
Mehrabi A, Hafezi M, Arvin J, Esmaeilzadeh M, Garoussi C, Emami G, Kossler-Ebs J, Muller-Stich BP, Buchler MW, Hackert T, Diener MK (2015) A systematic review and meta-analysis of laparoscopic versus open distal pancreatectomy for benign and malignant lesions of the pancreas: it’s time to randomize. Surgery 157:45–55. doi:10.1016/j.surg.2014.06.081
Nigri GR, Rosman AS, Petrucciani N, Fancellu A, Pisano M, Zorcolo L, Ramacciato G, Melis M (2011) Metaanalysis of trials comparing minimally invasive and open distal pancreatectomies. Surg Endosc 25:1642–1651. doi:10.1007/s00464-010-1456-5
Ejaz A, Sachs T, He J, Spolverato G, Hirose K, Ahuja N, Wolfgang CL, Makary MA, Weiss M, Pawlik TM (2014) A comparison of open and minimally invasive surgery for hepatic and pancreatic resections using the Nationwide Inpatient Sample. Surgery 156:538–547. doi:10.1016/j.surg.2014.03.046
Drymousis P, Raptis DA, Spalding D, Fernandez-Cruz L, Menon D, Breitenstein S, Davidson B, Frilling A (2014) Laparoscopic versus open pancreas resection for pancreatic neuroendocrine tumours: a systematic review and meta-analysis. HPB (Oxford) 16:397–406. doi:10.1111/hpb.12162
Jin T, Altaf K, Xiong JJ, Huang W, Javed MA, Mai G, Liu XB, Hu WM, Xia Q (2012) A systematic review and meta-analysis of studies comparing laparoscopic and open distal pancreatectomy. HPB (Oxford) 14:711–724. doi:10.1111/j.1477-2574.2012.00531.x
DiNorcia J, Ahmed L, Lee MK, Reavey PL, Yakaitis EA, Lee JA, Schrope BA, Chabot JA, Allendorf JD (2010) Better preservation of endocrine function after central versus distal pancreatectomy for mid-gland lesions. Surgery 148:1246–1247. doi:10.1016/j.surg.2010.09.003
De Rooij T, Sitarz R, Busch OR, Besselink MG, Abu Hilal M (2015) Technical aspects of laparoscopic distal pancreatectomy for benign and malignant disease: review of the literature. Gastroenterol Res Pract 2015:472906. doi:10.1155/2015/472906
Fernandez Ranvier GG, Shouhed D, Inabnet WB 3rd (2016) Minimally invasive techniques for resection of pancreatic neuroendocrine tumors. Surg Oncol Clin N Am 25:195–215. doi:10.1016/j.soc.2015.08.009
Strasberg SM, Drebin JA, Linehan D (2003) Radical antegrade modular pancreatosplenectomy. Surgery 133:521–527. doi:10.1067/msy.2003.146
Strasberg SM, Fields R (2012) Left-sided pancreatic cancer: distal pancreatectomy and its variants: radical antegrade modular pancreatosplenectomy and distal pancreatectomy with celiac axis resection. Cancer J 18:562–570. doi:10.1097/PPO.0b013e31827596c5
Fernandez-Cruz L, Molina V, Vallejos R, Jimenez Chavarria E, Lopez-Boado MA, Ferrer J (2012) Outcome after laparoscopic enucleation for non-functional neuroendocrine pancreatic tumours. HPB (Oxford) 14:171–176. doi:10.1111/j.1477-2574.2011.00422.x
Crippa S, Bassi C, Warshaw AL, Falconi M, Partelli S, Thayer SP, Pederzoli P, Fernandez-del Castillo C (2007) Middle pancreatectomy: indications, short- and long-term operative outcomes. Ann Surg 246:69–76. doi:10.1097/01.sla.0000262790.51512.57
Rotellar F, Pardo F, Cervera M, Gil A, Valenti V, Pastor C, Cienfuegos JA (2006) Laparoscopic distal pancreatectomy with or without splenectomy. Surgical technique. SurgEndosc 20(Suppl 1):S245
Rotellar F, Pardo F, Montiel C, Benito A, Regueira FM, Poveda I, Marti-Cruchaga P, Cienfuegos JA (2008) Totally laparoscopic Roux-en-Y duct-to-mucosa pancreaticojejunostomy after middle pancreatectomy: a consecutive nine-case series at a single institution. Ann Surg 247:938–944. doi:10.1097/SLA.0b013e3181724e4a
Rotellar F, Pardo F, Benito A, Marti-Cruchaga P, Zozaya G, Cienfuegos JA (2011) Laparoscopic resection of the uncinate process of the pancreas: the inframesocolic approach and hanging maneuver of the mesenteric root. Surg Endosc 25:3426–3427. doi:10.1007/s00464-011-1740-z
Fernández-Cruz L, Cosa R, Blanco L, Levi S, Lopez-Boado MA, Navarro S (2007) Curative laparoscopic resection for pancreatic neoplasms: a critical analysis from a single institution. J Gastrointest Surg 11:1607–1621. doi:10.1007/s11605-007-0266-0
NCCN clinical practice guidelines in Oncology. Neuroendocrine tumors (2016)). https://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed 26 May 2016
Rindi G, Falconi M, Klersy C, Albarello L, Boninsegna L, Buchler MW, Capella C, Caplin M, Couvelard A, Doglioni C, Delle Fave G, Fischer L, Fusai G, de Herder WW, Jann H, Komminoth P, de Krijger RR, La Rosa S, Luong TV, Pape U, Perren A, Ruszniewski P, Scarpa A, Schmitt A, Solcia E, Wiedenmann B (2012) TNM staging of neoplasms of the endocrine pancreas: results from a large international cohort study. J Natl Cancer Inst 104:764–777. doi:10.1093/jnci/djs208
American Diabetes Association (2011) Diagnosis and classification of diabetes mellitus. Diabetes Care 34(Suppl 1):S62–S69. doi:10.2337/dc11-S062
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M, Definition ISG on PF (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Buchler MW (2007) Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142:20–25
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Buchler MW (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142:761–768
Ricci C, Casadei R, Taffurelli G, Campana D, Ambrosini V, Pagano N, Santini D, De Giorgio R, Ingaldi C, Tomassetti P, Zani E, Minni F (2016) Validation of the 2010 WHO classification and a new prognostic proposal: a single centre retrospective study of well-differentiated pancreatic neuroendocrine tumours. Pancreatol Off J Int Assoc Pancreatol. et al
Klimstra DS (2016) Pathologic classification of neuroendocrine neoplasms. Hematol Oncol Clin North Am 30:1–19. doi:10.1016/j.hoc.2015.08.005
Hamilton NA, Liu TC, Cavatiao A, Mawad K, Chen L, Strasberg SS, Linehan DC, Cao D, Hawkins WG (2012) Ki-67 predicts disease recurrence and poor prognosis in pancreatic neuroendocrine neoplasms. Surgery 152:107–113. doi:10.1016/j.surg.2012.02.011
Ellison TA, Wolfgang CL, Shi C, Cameron JL, Murakami P, Mun LJ, Singhi AD, Cornish TC, Olino K, Meriden Z, Choti M, Diaz LA, Pawlik TM, Schulick RD, Hruban RH, Edil BH (2014) A single institution’s 26-year experience with nonfunctional pancreatic neuroendocrine tumors: a validation of current staging systems and a new prognostic nomogram. Ann Surg 259:204–212. doi:10.1097/SLA.0b013e31828f3174
Strosberg JR, Cheema A, Weber JM, Ghayouri M, Han G, Hodul PJ, Kvols LK (2012) Relapse-free survival in patients with nonmetastatic, surgically resected pancreatic neuroendocrine tumors: an analysis of the AJCC and ENETS staging classifications. Ann Surg 256:321–325. doi:10.1097/SLA.0b013e31824e6108
Fischer L, Bergmann F, Schimmack S, Hinz U, Priess S, Muller-Stich BP, Werner J, Hackert T, Buchler MW (2014) Outcome of surgery for pancreatic neuroendocrine neoplasms. Br J Surg. doi:10.1002/bjs.9603
Kim MJ, Choi DW, Choi SH, Heo JS, Park HJ, Choi KK, Jang KT, Sung JY (2012) Surgical strategies for non-functioning pancreatic neuroendocrine tumours. Br J Surg 99:1562–1568. doi:10.1002/bjs.8892
Birnbaum DJ, Gaujoux S, Cherif R, Dokmak S, Fuks D, Couvelard A, Vullierme MP, Ronot M, Ruszniewski P, Belghiti J, Sauvanet A (2014) Sporadic nonfunctioning pancreatic neuroendocrine tumors: prognostic significance of incidental diagnosis. Surgery 155:13–21. doi:10.1016/j.surg.2013.08.007
Hochwald SN, Zee S, Conlon KC, Colleoni R, Louie O, Brennan MF, Klimstra DS (2002) Prognostic factors in pancreatic endocrine neoplasms: an analysis of 136 cases with a proposal for low-grade and intermediate-grade groups. J Clin Oncol 20:2633–2642
Jusoh AC, Ammori BJ (2012) Laparoscopic versus open distal pancreatectomy: a systematic review of comparative studies. Surg Endosc 26:904–913. doi:10.1007/s00464-011-2016-3
Pericleous S, Middleton N, McKay SC, Bowers KA, Hutchins RR (2012) Systematic review and meta-analysis of case-matched studies comparing open and laparoscopic distal pancreatectomy: is it a safe procedure? Pancreas 41:993–1000. doi:10.1097/MPA.0b013e31824f3669
Sui CJ, Li B, Yang JM, Wang SJ, Zhou YM (2012) Laparoscopic versus open distal pancreatectomy: a meta-analysis. Asian J Surg 35:1–8. doi:10.1016/j.asjsur.2012.04.001
Xie K, Zhu YP, Xu XW, Chen K, Yan JF, Mou YP (2012) Laparoscopic distal pancreatectomy is as safe and feasible as open procedure: a meta-analysis. World J Gastroenterol 18:1959–1967. doi:10.3748/wjg.v18.i16.1959
Strosberg JR, Weber JM, Feldman M, Coppola D, Meredith K, Kvols LK (2013) Prognostic validity of the American Joint Committee on Cancer staging classification for midgut neuroendocrine tumors. J Clin Oncol 31:420–425. doi:10.1200/JCO.2012.44.5924
Kuroki T, Eguchi S (2014) Laparoscopic parenchyma-sparing pancreatectomy. J Hepatobiliary Pancreat Sci 21:323–327. doi:10.1002/jhbp.29
Crippa S, Bassi C, Salvia R, Falconi M, Butturini G, Pederzoli P (2007) Enucleation of pancreatic neoplasms. Br J Surg 94:1254–1259. doi:10.1002/bjs.5833
Huttner FJ, Koessler-Ebs J, Hackert T, Ulrich A, Buchler MW, Diener MK (2015) Meta-analysis of surgical outcome after enucleation versus standard resection for pancreatic neoplasms. Br J Surg. doi:10.1002/bjs.9819
Haugvik SP, Marangos IP, Rosok BI, Pomianowska E, Gladhaug IP, Mathisen O, Edwin B (2013) Long-term outcome of laparoscopic surgery for pancreatic neuroendocrine tumors. World J Surg 37:582–590. doi:10.1007/s00268-012-1893-5
Hwang HK, Chung YE, Kim KA, Kang CM, Lee WJ (2012) Revisiting vascular patency after spleen-preserving laparoscopic distal pancreatectomy with conservation of splenic vessels. Surg Endosc 26:1765–1771. doi:10.1007/s00464-011-2108-0
Martin LW, Ryckman FC, Sheldon CA (1984) Experience with 95% pancreatectomy and splenic salvage for neonatal nesidioblastosis. Ann Surg 200:355–362
Jain G, Chakravartty S, Patel AG (2013) Spleen-preserving distal pancreatectomy with and without splenic vessel ligation: a systematic review. HPB (Oxford) 15:403–410. doi:10.1111/hpb.12003
Fernandez-Cruz L, Martinez I, Gilabert R, Cesar-Borges G, Astudillo E, Navarro S (2004) Laparoscopic distal pancreatectomy combined with preservation of the spleen for cystic neoplasms of the pancreas. J Gastrointest Surg 8:493–501. doi:10.1016/j.gassur.2003.11.014
Melotti G, Butturini G, Piccoli M, Casetti L, Bassi C, Mullineris B, Lazzaretti MG, Pederzoli P (2007) Laparoscopic distal pancreatectomy: results on a consecutive series of 58 patients. Ann Surg 246:77–82. doi:10.1097/01.sla.0000258607.17194.2b
Baldwin KM, Katz SC, Espat NJ, Somasundar P (2011) Laparoscopic spleen-preserving distal pancreatectomy in elderly subjects: splenic vessel sacrifice may be associated with a higher rate of splenic infarction. HPB (Oxford) 13:621–625. doi:10.1111/j.1477-2574.2011.00341.x
Zhou ZQ, Kim SC, Song KB, Park KM, Lee JH, Lee YJ (2014) Laparoscopic spleen-preserving distal pancreatectomy: comparative study of spleen preservation with splenic vessel resection and splenic vessel preservation. World J Surg 38:2973–2979. doi:10.1007/s00268-014-2671-3
Mabrut JY, Fernandez-Cruz L, Azagra JS, Bassi C, Delvaux G, Weerts J, Fabre JM, Boulez J, Baulieux J, Peix JL, Gigot JF, Surgery H and PS (HBPS) of the RBS of, (BGES) BG for ES, Coelio C (2005) Laparoscopic pancreatic resection: results of a multicenter European study of 127 patients. Surgery 137:597–605
Kimura W, Tezuka K, Hirai I (2011) Surgical management of pancreatic neuroendocrine tumors. Surg Today 41:1332–1343. doi:10.1007/s00595-011-4547-6
Gianduzzo TR, Colombo JR Jr, Haber GP, Magi-Galluzzi C, Dall’Oglio MF, Ulchaker J, Gill IS (2009) KTP laser nerve sparing radical prostatectomy: comparison of ultrasonic and cold scissor dissection on cavernous nerve function. J Urol 181:2760–2766. doi:10.1016/j.juro.2009.01.095
Yoon YS, Lee KH, Han HS, Cho JY, Ahn KS (2009) Patency of splenic vessels after laparoscopic spleen and splenic vessel-preserving distal pancreatectomy. Br J Surg 96:633–640. doi:10.1002/bjs.6609
Fendrich V, Merz MK, Waldmann J, Langer P, Heverhagen AE, Dietzel K, Bartsch DK (2011) Neuroendocrine pancreatic tumors are risk factors for pancreatic fistula after pancreatic surgery. Dig Surg 28:263–269. doi:10.1159/000328667
Heeger K, Falconi M, Partelli S, Waldmann J, Crippa S, Fendrich V, Bartsch DK (2014) Increased rate of clinically relevant pancreatic fistula after deep enucleation of small pancreatic tumors. Langenbecks Arch Surg 399:315–321. doi:10.1007/s00423-014-1171-0
Atema JJ, Jilesen AP, Busch OR, van Gulik TM, Gouma DJ, Nieveen van Dijkum EJ (2015) Pancreatic fistulae after pancreatic resections for neuroendocrine tumours compared with resections for other lesions. HPB (Oxford) 17:38–45. doi:10.1111/hpb.12319
Mehta VV, Fisher SB, Maithel SK, Sarmiento JM, Staley CA, Kooby DA (2013) Is it time to abandon routine operative drain use? A single institution assessment of 709 consecutive pancreaticoduodenectomies. J Am Coll Surg 216:634–635. doi:10.1016/j.jamcollsurg.2012.12.040
Adham M, Chopin-Laly X, Lepilliez V, Gincul R, Valette PJ, Ponchon T (2013) Pancreatic resection: drain or no drain? Surgery 154:1069–1077. doi:10.1016/j.surg.2013.04.017
Tosoian JJ, Hicks CW, Cameron JL, Valero V 3rd, Eckhauser FE, Hirose K, Makary MA, Pawlik TM, Ahuja N, Weiss MJ, Wolfgang CL (2015) Tracking early readmission after pancreatectomy to index and nonindex institutions: a more accurate assessment of readmission. JAMA Surg 150:152–158. doi:10.1001/jamasurg.2014.2346
Strobel O, Cherrez A, Hinz U, Mayer P, Kaiser J, Fritz S, Schneider L, Klauss M, Buchler MW, Hackert T (2015) Risk of pancreatic fistula after enucleation of pancreatic tumours. Br J Surg. doi:10.1002/bjs.9843
Tjaden C, Hinz U, Hassenpflug M, Fritz F, Fritz S, Grenacher L, Buchler MW, Hackert T (2016) Fluid collection after distal pancreatectomy: a frequent finding. HPB (Oxford) 18:35–40
Tilara A, Gerdes H, Allen P, Jarnagin W, Kingham P, Fong Y, DeMatteo R, D’Angelica M, Schattner M (2014) Endoscopic ultrasound-guided transmural drainage of postoperative pancreatic collections. J Am Coll Surg 218:33–40. doi:10.1016/j.jamcollsurg.2013.09.001
Pradella S, Mazza E, Mondaini F, Colagrande S (2013) Pancreatic fistula: a proposed percutaneous procedure. World J Hepatol 5:33–37. doi:10.4254/wjh.v5.i1.33
Gurusamy KS, Koti R, Fusai G, Davidson BR (2013) Somatostatin analogues for pancreatic surgery. Cochrane Database Syst Rev 4:CD008370. doi:10.1002/14651858.CD008370.pub3
Fernandez-Cruz L, Jimenez Chavarria E, Taura P, Closa D, Boado MA, Ferrer J (2013) Prospective randomized trial of the effect of octreotide on pancreatic juice output after pancreaticoduodenectomy in relation to histological diagnosis, duct size and leakage. HPB (Oxford) 15:392–399. doi:10.1111/j.1477-2574.2012.00608.x
Alghamdi AA, Jawas AM, Hart RS (2007) Use of octreotide for the prevention of pancreatic fistula after elective pancreatic surgery: a systematic review and meta-analysis. Can J surgeryJournal Can Chir 50:459–466
Li-Ling J, Irving M (2001) Somatostatin and octreotide in the prevention of postoperative pancreatic complications and the treatment of enterocutaneous pancreatic fistulas: a systematic review of randomized controlled trials. Br J Surg 88:190–199
De Bruijn KM, van Eijck CH (2015) New-onset diabetes after distal pancreatectomy: a systematic review. Ann Surg 261:854–861. doi:10.1097/SLA.0000000000000819
Lillemoe KD, Kaushal S, Cameron JL, Sohn TA, Pitt HA, Yeo CJ (1999) Distal pancreatectomy: indications and outcomes in 235 patients. Ann Surg 229:693–700
King J, Kazanjian K, Matsumoto J, Reber HA, Yeh MW, Hines OJ, Eibl G (2008) Distal pancreatectomy: incidence of postoperative diabetes. J Gastrointest Surg 12:1548–1553. doi:10.1007/s11605-008-0560-5
Shirakawa S, Matsumoto I, Toyama H, Shinzeki M, Ajiki T, Fukumoto T, Ku Y (2012) Pancreatic volumetric assessment as a predictor of new-onset diabetes following distal pancreatectomy. J Gastrointest Surg 16:2212–2219. doi:10.1007/s11605-012-2039-7
Dumitrascu T, Scarlat A, Ionescu M, Popescu I (2012) Central pancreatectomy versus spleen-preserving distal pancreatectomy: a comparative analysis of early and late postoperative outcomes. Dig Surg 29:400–407. doi:10.1159/000343927
Maeda H, Hanazaki K (2011) Pancreatogenic diabetes after pancreatic resection. Pancreatol Off J Int Assoc Pancreatol 11:268–276. doi:10.1159/000328785
Kendall DM, Sutherland DE, Najarian JS, Goetz FC, Robertson RP (1990) Effects of hemipancreatectomy on insulin secretion and glucose tolerance in healthy humans. N Engl J Med 322:898–903. doi:10.1056/NEJM199003293221305
Menge BA, Tannapfel A, Belyaev O, Drescher R, Muller C, Uhl W, Schmidt WE, Meier JJ (2008) Partial pancreatectomy in adult humans does not provoke beta-cell regeneration. Diabetes 57:142–149. doi:10.2337/db07-1294
Acknowledgements
The authors are grateful to Paul Miller Ph.D. for his help with the English and Lydia Munárriz for transcribing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Javier A. Cienfuegos, Joseba Salguero, Núñez-Córdoba Jorge M, Miguel Ruiz-Canela, Alberto Benito, Sira Ocaña, Gabriel Zozaya, Pablo Martí-Cruchaga, Fernando Pardo, José Luis Hernández-Lizoáin and Fernando Rotellar have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Cienfuegos, J.A., Salguero, J., Núñez-Córdoba, J.M. et al. Short- and long-term outcomes of laparoscopic organ-sparing resection in pancreatic neuroendocrine tumors: a single-center experience. Surg Endosc 31, 3847–3857 (2017). https://doi.org/10.1007/s00464-016-5411-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5411-y